Abstract
Objective
This study evaluated the efficiency of anchorage provided by temporary anchorage devices (TADs) in maxillary bicuspid extraction cases during retraction of the anterior teeth using a fixed appliance.
Methods
Patients aged 12 to 50 years with malocclusion for which bilateral first or second maxillary bicuspid extractions were indicated were included in the study and randomly allocated to the TAD or control groups. Retraction of the anterior teeth was achieved using skeletal anchorage in the TAD group and conventional dental anchorage in the control group. A computed tomography (CT) scan was performed after alignment of teeth, and a second CT scan was performed at the end of extraction space closure in both groups. A three-dimensional superimposition was performed to visualize and quantify the maxillary first molar movement during the retraction phase, which was the primary outcome, and the stability of TAD movement, which served as the secondary outcome.
Results
Thirty-four patients (17 in each group) underwent the final analysis. The two groups showed a significant difference in the movement of the first maxillary molars, with less significant anchorage loss in the TAD group than that in the control group. In addition, TAD movement showed only a slight mesial movement on the labial side. On the palatal side, the mesial TAD movement was greater.
Anchorage loss is one of the main concerns associated with orthodontic procedures. Although some appliances have been developed to control anchorage, they require patient compliance (e.g., head gear) or are not very efficient in maintaining anchorage. The use of skeletal anchorage to retract anterior maxillary teeth is an old concept developed by Gainsforth and Higley1 in 1945 on a canine model. Following this experiment, other authors published studies on skeletal anchorage, including Linkow,2 Wehrbein et al.,3 and Melsen et al.4 Park5 developed micro-implants measuring 1.2 mm in diameter and 6 mm in length for “en masse” maxillary dental retraction. Lee et al.,6 in his study, positioned temporary anchorage devices (TADs) in the palate for anterior tooth retraction. About the same time, numerous clinical cases were published by Kyung et al.,7 Maino et al.,8 and Park et al.9 Over the past decade, scientific research in this field has continued to progress, and numerous randomized clinical trials on TADs have been reported.101112131415
The purpose of this study was to compare TAD anchorage and conventional dental anchorage in patients requiring maxillary bicuspid extractions for treatment during en masse retraction of anterior teeth. The primary outcome of this multicentric randomized clinical trial was the molar anchorage loss and the secondary outcome was the TAD movement during en masse retraction of the anterior teeth using a fixed labial appliance. Movements were evaluated by computed tomography (CT) scans and three-dimensional (3D) superimpositions.
Ninety-nine patients aged between 12 and 50 years requiring orthodontic treatment by extraction of the maxillary bicuspids with the need for anchorage were selected between February 2009 and February 2012. All patients were in good general health. Written consent signed by the patients and the parents of children was mandatory for inclusion in the study. This multicentric trial involved eight centers.
A stratified randomization was performed using separate randomization lists for each location along with blocking to ensure equal-sized trial arms. An independent and centralized assignment protocol involving any persons associated with the trial in the eight centers ensured randomization. The trial was approved by the ethics committee of Necker Hospital and was conducted in accordance with the Helsinki declaration (agreement No. SCR07011). The patients were divided randomly into two groups: those in the TAD group received TAD-supported anchorage, while those in the control group received conventional dental anchorage with a Nance appliance, transpalatal bar, and banding or bonding of the second molars. No patient received headgear anchorage.
All patients were treated with a 0.022 × 0.028 slot fixed appliance with self-ligating or conventional brackets, since the literature has demonstrated that there is no difference in sliding mechanics between conventional and self-ligating brackets.16
Extractions were performed after leveling when there was no or minor crowding and, for ethical reasons, at the beginning of treatment when crowding was moderate or severe in order to avoid increasing the overjet and for periodontal considerations. All patients underwent either first or second bicuspid extractions. During en masse space closure, 0.019 × 0.025 Stainless Steel archwires with power arms were applied. The length of the power arm was adjusted to obtain horizontal force between the power arm and the TAD. On the palatal side, a power arm was bonded to the palatal side of the cuspid with length adjusted as described above (Figure 1A and 1B).
Immediately after leveling, four TADs were placed: two on the buccal side and two on the palatal side between the second bicuspid and the first molar. Abso-Anchor TADs manufactured by Dentos™ (Daegu, Korea) were inserted in every case. On the buccal side, TADs measuring 1.3 to 1.2 mm or 1.4 to 1.3 mm in diameter and 8 mm in length were inserted depending on the inter-radicular spaces, as recommended by Wu et al.17 On the palatal side, thicker and longer TADs (diameter, 1.6–1.7 mm; length, 10 mm) were chosen to compensate for the mucosal thickness. TAD insertion was performed in the attached gingival tissue without predrilling, in accordance with the recommendations made by Dalessandri et al.18
In the TAD group, a loading force of 100 g (3.5 ounce) was applied on the labial and buccal sides immediately after TAD insertion between the TADs and the power arms on the archwire by using power chains, according to the method described by Hsieh et al.19 The power chains were replaced every month. In the control group, space closure was performed by en masse retraction of the six anterior teeth by means of conventional sliding mechanics with the same amount of force.
The first CT scan was obtained immediately after TAD placement for every patient in the TAD group and at the beginning of en masse retraction of the six anterior teeth in the control group. The second CT scan was obtained immediately after space closure in both groups before debonding (Figure 1C and 1D).
All CT scans were processed with Meshlab™ software (ISTI [Italian National Research Council], Rome, Italy) to eliminate artifacts caused by the orthodontic appliance and to prepare the images for the superimpositions. The 3D superimpositions were performed with the best-fit method using only a local maxillary superimposition considering the maxilla base as a fixed surface to assess dental movement alone. This local superimposition was performed in accordance with the study by Treil et al.,20 which used the infraorbital foramen as a fixed point with the best-fit method. The superimposition was performed with the Cloudcompare™ v2.6.0 software (Research and Development Electricity Institute EDF, Paris, France). The color palette was changed a second time to shades of grey to enhance visualization of TADs and tooth movement.
The power analysis showed that a set of at least 16 subjects per group would yield an 80% probability of detecting a significant difference between the two groups at a 5% statistical significance level (Stata Corp., College Dtation, TX, USA), as described in the study by Upadhyay et al.11
All measurements were performed by two independent evaluators specialized in 3D imaging and not involved in the clinical part of the study. The assessment of 3D images was not blinded as the TADs were visible on the CT scans, but each evaluator analyzed the results independently from the other without any knowledge of the results obtained by the other evaluator, and the correlation between evaluators' measurements was assessed with analysis of variance (ANOVA). Statistical analyses were performed with SigmaStat 3.5™ software (Systat Software, Inc., Chicago, IL, USA). Paired and unpaired t-tests as well as repeated-measures ANOVA (Satterthwaite's method) were performed.
Ninety-nine patients were assessed for eligibility according to the inclusion criteria. Twenty-four were excluded for different reasons (change in treatment plan or refusal to undergo treatment after signing the written consent). Seventy-five patients were randomized, 36 in the skeletal anchorage (TAD) group and 39 in the dental anchorage (control) group. During the trial, several subjects were lost to follow-up (19 in the TAD group and 22 in the control group) due to loss of TAD in the TAD group (n = 14) and due to the absence of a second CT scan following technical problems (n = 3 in the TAD group and n = 9 in the control group) or withdrawal from treatment (n = 2 in the TAD group and n = 13 in the control group).
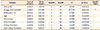
Mean patient age was 18.00 ± 9.37 years in the TAD group and 14.11 ± 3.99 years in the control group. ANOVA revealed that the age was not significantly different between the two groups (p = 0.552). The sex distribution in the two groups was comparable, with 10 females and seven males in the TAD group and 11 females and six males in the control group. The extraction site was also homogeneously distributed between the two groups, with 12 extractions of maxillary first bicuspids, three extractions of maxillary second bicuspids, and two cases of asymmetrical extractions (first bicuspid on one side and second bicuspid on the other) in the TAD group, and 12 extractions of maxillary first bicuspids, four extractions of maxillary second bicuspids, and one case of asymmetrical extraction in the control group.
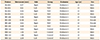
The stability of the first molars was evaluated at the mesiobuccal cusp. Mesial movement of the maxillary first molars was observed in the TAD group (mean, 0.56 ± 0.53 mm) and in the control group (mean, 1.30 ± 0.69 mm), and the difference in this movement was statistically significant (p < 0.05). ANOVA with Satterthwaite's method revealed that differences related to age, evaluator, and the side (left or right) were not statistically significant. The absence of differences between the left and right sides enabled us to aggregate the results for the two sides (Tables 1 and 2).
A total of 124 TADs were placed in 31 patients (four TADs per patient), and 17 TADs were lost in 14 patients during the treatment period, indicating a TAD loss proportion of 13.7%.
On the buccal side, the measurements were made at the head of the miniscrew, and a mesial movement (mean, 0.63 ± 0.83 mm) was observed in the direction of the orthodontic loading of the TADs. The measurements on the palatal side revealed a mesial movement (mean, 1.35 ± 1.91 mm). TAD movement showed a significant difference, with the TADs being less stable on the palatal side than on the buccal side (p < 0.05).
This study revealed a significant difference between TAD group and control group concerning the first molar anchorage loss during en masse anterior teeth retraction (TAD group, 0.56 ± 0.53 mm; control group, 1.30 ± 0.69 mm). A TAD loss proportion of 13.7% was observed. The mesial TAD movement observed was significantly higher on the buccal side (mean, 0.63 ± 0.83 mm) in comparison to the palatal side (mean, 1.35 ± 1.91 mm).
During space closure, our study demonstrated a significant difference between the TAD and control groups; the former had less anchorage loss compared with latter group. Other studies revealed the same results, but most of them used two-dimensional cephalometric tracing, which is less precise.11131421 The study by Liu et al.22 with 3D superimposition showed a mean mesial movement higher than that in the present study. In contrast, the study by Sandler et al.15 found no statistically significant difference between the conventional anchorage groups (headgear and Nance) and the TAD group. Their study was performed using 3D superimpositions on dental casts from 78 patients. However, the sample was quite different from the one in our study, since there were only 59 cases with bicuspid extractions; 19 cases involved other types of extraction including the first molars, and one case involved no extractions. In a systematic review published in 2014, Jambi et al.23 showed that the mean mesiodistal movement of the upper first permanent molars in the control group ranged from 1.47 to 3.22 mm and was 1.68 mm lower (2.27 to 1.09 mm lower) in the TAD group. Some recent meta-analyses and systematic reviews242526272829 confirmed the efficacy of en masse retraction of the anterior teeth in comparison to conventional anchorage or two-step retraction, with the difference in anchorage loss of around 2.5 mm being in favor of en masse retraction with TADs. In our study, the difference in anchorage loss between the TAD group and conventional anchorage group was significant but at a lower level (0.74 mm). The previous studies were also mainly performed on lateral cephalograms, which are not very precise, especially for assessing maxillary molar movement, when the left and right molars are not perfectly superimposed on the lateral ceph.
The TAD loss rate in our study was 13.7%. This result is in agreement with the literature concerning the rate of TAD loss.3031 Patients with TAD loss were excluded from the study, since the main objective was to assess the mesial movement of the maxillary first molar. Indeed, when TAD loss occurs, some time may be required to replace the TAD and so the anchorage may be lost.
On the buccal side, the TADs were quite stable with a slight movement in the direction of the loading force. In the literature, there are few studies assessing TAD movement. Liou et al.32 assessed 16 adult female patients using TADs measuring 17 mm in length and 2 mm in diameter and revealed a similar 0.4-mm mesial movement ranging from −1 mm in the distal direction to 1.5 mm in the mesial direction. In our trial, we also noted three patients with limited backward movement ranging between 0.11 and 1.06 mm. This finding could perhaps be explained by archwire friction on the orthodontic appliance during the space closure phase. The most similar study evaluating the movement of TADs was conducted by Liu et al.22 on 60 patients with 3D CT scans. They found the same range of mesial movement (0.23 ± 0.08 mm). On the palatal side, we observed a double mesial movement in contrast to that on the buccal side. On this side, the cortical bone is thicker, but the mucosa is also thicker, so the lever arm is longer on the palatal side, which could explain the difference in movement between the buccal and palatal TADs. The study by Büchter et al.33 demonstrated that if the lever arm increases, the bone-TAD contact ratio decreases at 70 days.
The number of patients lost to follow-up decreased the power of the study. The fact that the study included growing patients may have distorted the superimpositions we made, even though we took a fixed point on the maxilla. However, this is probably only a minor distortion since the CT scans were taken before space closure and at the end of space closure and not at the beginning and at the end of treatment; thus, the interval between the two images was quite short. The patients in the TAD group were older (18 years) than those the control group (14.11 years), and this difference might have affected the results, although there was no statistical difference between the groups in term of age. In this randomized clinical trial, it was impossible to blind patients and operators to treatment allocation.
In this randomized clinical trial on the stability of the first maxillary molars during en masse retraction of the anterior teeth, when skeletal anchorage was used, posterior anchorage was statistically superior to conventional dental anchorage. This study also revealed the TAD movement under orthodontic loading forces, with less TAD movement on the buccal side as opposed to the palatal side.
Figures and Tables
Figure 1
A, Intra-oral photograph of temporary anchorage device (TAD) insertion on the labial side with an elastomeric chain for the en masse retraction of the six anterior teeth. B, Intra-oral view of TAD insertion on the palatal side. C, Computed tomography (CT) scan performed on the day of TAD insertion. D, CT scan performed after extraction space closure.
ACKNOWLEDGEMENTS
The authors would like to deeply thank Dr. Alain Decker from Paris Descartes University who initiated this project but unfortunately passed away before the writing of this article, and also Jean Baptiste Dagorne and François Boutin for their precious help in this research.
Notes
References
1. Gainsforth BL, Higley LB. A study of orthodontic anchorage possibilities in basal bone. Am J Orthod Oral Surg. 1945; 31:406–417.

2. Linkow LI. The endosseous blade implant and its use in orthodontics. Int J Orthod. 1969; 7:149–154.
3. Wehrbein H, Glatzmaier J, Mundwiller U, Diedrich P. The orthosystem--a new implant system for orthodontic anchorage in the palate. J Orofac Orthop. 1996; 57:142–153.
4. Melsen B, Petersen JK, Costa A. Zygoma ligatures: an alternative form of maxillary anchorage. J Clin Orthod. 1998; 32:154–158.
5. Park HS. The skeletal cortical anchorage using titanium microscrew implants. Korean J Orthod. 1999; 29:699–706.
6. Lee JS, Park HS, Kyung HM. Micro-implant anchorage for lingual treatment of a skeletal class II malocclusion. J Clin Orthod. 2001; 35:643–647. quiz 620.
7. Kyung HM, Park HS, Bae SM, Sung JH, Kim IB. Development of orthodontic micro-implants for intraoral anchorage. J Clin Orthod. 2003; 37:321–328. quiz 314.
8. Maino BG, Bednar J, Pagin P, Mura P. The spider screw for skeletal anchorage. J Clin Orthod. 2003; 37:90–97.
9. Park HS, Lee SK, Kwon OW. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod. 2005; 75:602–609.
10. Benson PE, Tinsley D, O'Dwyer JJ, Majumdar A, Doyle P, Sandler PJ. Midpalatal implants vs headgear for orthodontic anchorage: a randomized clinical trial: cephalometric results. Am J Orthod Dentofacial Orthop. 2007; 132:606–615.

11. Upadhyay M, Yadav S, Nagaraj K, Patil S. Treatment effects of mini-implants for en-masse retraction of anterior teeth in bialveolar dental protrusion patients: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008; 134:18–29.e1.

12. Garfinkle JS, Cunningham LL Jr, Beeman CS, Kluemper GT, Hicks EP, Kim MO. Evaluation of orthodontic mini-implant anchorage in premolar extraction therapy in adolescents. Am J Orthod Dentofacial Orthop. 2008; 133:642–653.

13. Feldmann I, Bondemark L. Anchorage capacity of osseointegrated and conventional anchorage systems: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008; 133:339–352.

14. Sharma M, Sharma V, Khanna B. Mini-screw implant or transpalatal arch-mediated anchorage reinforcement during canine retraction: a randomized clinical trial. J Orthod. 2012; 39:102–110.

15. Sandler J, Murray A, Thiruvenkatachari B, Gutierrez R, Speight P, O'Brien K. Effectiveness of 3 methods of anchorage reinforcement for maximum anchorage in adolescents: a 3-arm multicenter randomized clinical trial. Am J Orthod Dentofacial Orthop. 2014; 146:10–20.

16. Miles PG. Self-ligating vs conventional twin brackets during en-masse space closure with sliding mechanics. Am J Orthod Dentofacial Orthop. 2007; 132:223–225.

17. Wu TY, Kuang SH, Wu CH. Factors associated with the stability of mini-implants for orthodontic anchorage: a study of 414 samples in Taiwan. J Oral Maxillofac Surg. 2009; 67:1595–1599.

18. Dalessandri D, Salgarello S, Dalessandri M, Lazzaroni E, Piancino M, Paganelli C, et al. Determinants for success rates of temporary anchorage devices in orthodontics: a meta-analysis (n > 50). Eur J Orthod. 2014; 36:303–313.

19. Hsieh YD, Su CM, Yang YH, Fu E, Chen HL, Kung S. Evaluation on the movement of endosseous titanium implants under continuous orthodontic forces: an experimental study in the dog. Clin Oral Implants Res. 2008; 19:618–623.

20. Treil J, Casteigt J, Borianne P, Madrid C, Jaeger M, de Bonnecaze P. [Thearchitectural balance of the face: a 3D cephalometric concept]. Rev Stomatol Chir Maxillofac. 1999; 100:111–122. French.
21. Liu YH, Ding WH, Liu J, Li Q. Comparison of the differences in cephalometric parameters after active orthodontic treatment applying mini-screw implants or transpalatal arches in adult patients with bialveolar dental protrusion. J Oral Rehabil. 2009; 36:687–695.

22. Liu H, Lv T, Wang NN, Zhao F, Wang KT, Liu DX. Drift characteristics of miniscrews and molars for anchorage under orthodontic force: 3-dimensional computed tomography registration evaluation. Am J Orthod Dentofacial Orthop. 2011; 139:e83–e89.
23. Jambi S, Walsh T, Sandler J, Benson PE, Skeggs RM, O'Brien KD. Reinforcement of anchorage during orthodontic brace treatment with implants or other surgical methods. Cochrane Database Syst Rev. 2014; (8):CD005098.

24. Al-Sibaie S, Hajeer MY. Assessment of changes following en-masse retraction with mini-implants anchorage compared to two-step retraction with conventional anchorage in patients with class II division 1 malocclusion: a randomized controlled trial. Eur J Orthod. 2014; 36:275–283.

25. Antoszewska-Smith J, Sarul M, Łyczek J, Konopka T, Kawala B. Effectiveness of orthodontic miniscrew implants in anchorage reinforcement during enmasse retraction: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2017; 151:440–455.

26. Rizk MZ, Mohammed H, Ismael O, Bearn DR. Effectiveness of en masse versus two-step retraction: a systematic review and meta-analysis. Prog Orthod. 2018; 18:41.

27. Becker K, Pliska A, Busch C, Wilmes B, Wolf M, Drescher D. Efficacy of orthodontic mini implants for en masse retraction in the maxilla: a systematic review and meta-analysis. Int J Implant Dent. 2018; 4:35.

28. Pervin S, Rolland S, Taylor G. En masse versus two-step retraction of the anterior segment. Evid Based Dent. 2018; 19:111–112.

29. Alharbi F, Almuzian M, Bearn D. Anchorage effectiveness of orthodontic miniscrews compared to headgear and transpalatal arches: a systematic review and meta-analysis. Acta Odontol Scand. 2019; 77:88–98.

30. Schätzle M, Männchen R, Zwahlen M, Lang NP. Survival and failure rates of orthodontic temporary anchorage devices: a systematic review. Clin Oral Implants Res. 2009; 20:1351–1359.

31. Aly SA, Alyan D, Fayed MS, Alhammadi MS, Mostafa YA. Success rates and factors associated with failure of temporary anchorage devices: a prospective clinical trial. J Investig Clin Dent. 2018; 9:e12331.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download