A 50-year-old, previously healthy woman was admitted to the hospital because of severe epigastric pain. Her vital signs were normal with a maximum blood pressure of 135/70 mmHg. Physical examination revealed decreased bowel sounds and tenderness in the epigastric area with 2+ of pretibial pitting edema. Urinalysis revealed 3+ proteinuria and hematuria. The urine protein/creatinine ratio was 7,496 mg/g creatinine. First, to avoid surgery, we performed contrast-enhanced abdominal computerized tomography (CT). The origin of the celiac trunk was encapsulated by a hemorrhagic lesion and showed focal narrowing in the vascular lumen, which was associated with arterial wall dissection in the coronal view (arrow, Fig. 1A). Further laboratory examination revealed that serologic tests for C3 and C4 were 44 and 7.5 mg/dL, respectively. The anti-nuclear antibody titer was 1:1280, with a speckled pattern. Autoantibodies including anti-SSA/Ro, anti-SSB/La, anti-RNP, and anti-dsDNA were positive over 200 U/ml. Therefore, we suspected isolated celiac trunk dissection associated with lupus vasculitis. We administered high-dose methylprednisolone pulse therapy. After improvement of the abdominal pain, we performed a renal biopsy for evaluation of proteinuria. There are endocapillary proliferation, mesangial expansion with hypercellularity and diffuse glomerular basement membrane thickening (H&E stain, ×400, Fig. 2A). There was positive immunofluorescence staining of IgG on the glomerular basement membrane (×400, Fig. 2B). There were subepithelial and subendothelial electron-dense deposits with foot process effacement (electron micrograph, ×2,500, Fig. 2C). A tubuloreticular structure (arrow) was present in the endothelial cell (electron micrograph, ×4,000, Fig. 2D). We confirmed lupus nephritis, class V and class III (A/C). After renal biopsy, we added 2 g of mycofenolate mofetil and an antiplatelet agent with 100 mg of aspirin. Three months after immunosuppressive treatment, a follow-up CT scan showed a decrease in the hemorrhagic lesion around the celiac trunk and improved vascular luminal narrowing (arrowhead, Fig. 1B). Urinalysis also showed 1+ protein with microscopic hematuria.
The natural history of isolated spontaneous celiac artery dissection is unclear, however, most recently reports have shown that it is benign in nature and primarily treated by conservative measures, such as the control of blood pressure and vascular thrombosis prevention.1 In cases of bleeding, bowel ischemia, or aneurysm formation, endovascular or open surgical interventions are needed.2 Vascular involvement is frequently observed in SLE patients, presenting as an acute or subacute manifestation.3 Usually, vascular diseases in SLE involve medium- and small-sized vessels are known as lupus vasculitis with inflammatory and vascular wall necrosis and a thrombus formation in the lumen of the affected artery.4 Cutaneous vasculitis is the common form of lupus vasculitis; however, visceral involvement is reported in about 10% of cases, which can be life-threatening and require aggressive treatment.5 In this case a timely diagnostic and treatment measurements prevented further progression of bowel ischemia.
In conclusion, isolated spontaneous celiac artery dissection is a rare clinical condition but should be kept in mind as a differential diagnosis of abdominal pain in normotensive women who suspected autoimmue vasulitis.
Figures and Tables
FIG. 1
Contrast enhaced abdominal computed tomography (CT) of Celiac trunk. (A) Origin of Celiac trunk is encapsulated by hemorrhagic lesion and shows focal narrowing in vascular lumen. This lesion is associated with dissection of arterial wall in coronal scan view (arrow). (B) Follow-up CT scan shows much improved encapsulated hemorrhagic lesion and focal narrowing of vascular lumen after 3 months of diagnosis (arrowhead).
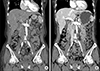
FIG. 2
Renal biopsy of the patient. (A) Representative glomerulus showing endocapillary proliferation, mesangial expansion with hypercellularity and diffuse glomerular basement thickening (H&E stain, ×400). (B) Immunofluorescence staining of IgG showing positive deposition in the glomerular basement membrane (IgG immunofluorescence stain, ×400). (C) There are subepithelial and subendothelial electron-dense deposits with foot process effacement (electronmicrograph, ×2,500). (D) Tubuloreticular structure (arrow) is present in the endothelial cell (electronmicrograph, ×4,000).

ACKNOWLEDGEMENTS
This research was supported by the National Research Foundation of Korea (NRF) funded by the Korean government (NRF-2018R1D1A1B07045790, to K.P.K).
References
1. Kim SR, Park TK, Choi SH, Kim SM, Choe YH, Heo SH, et al. Natural history of spontaneous isolated celiac artery dissection after conservative treatment. J Vasc Surg. 2018; 68:55–63.

2. DiMusto PD, Oberdoerster MM, Criado E. Isolated celiac artery dissection. J Vasc Surg. 2015; 61:972–976.

3. D'Cruz D. Vasculitis in systemic lupus erythematosus. Lupus. 1998; 7:270–274.
4. Radic M, Martinovic Kaliterna D, Radic J. Vascular manifestations of systemic lupus erythematosis. Neth J Med. 2013; 71:10–16.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download