Abstract
This study compared the effect of preservative-containing (PC) and preservative-free (PF) prostaglandin analogue (PGA) formulations on the ocular surface, especially on the meibomian gland (MG) in patients with open-angle glaucoma (OAG). This is a retrospective study of treatment-naïve patients with OAG (n=80) and healthy controls (n=40). OAG patients were randomized into groups using either PC-PGA or PF-PGA for 12 months. All participants underwent ocular surface and MG examinations including their meibum score, meiboscore, and lid margin abnormality score (LAS). Eighty OAG patients were randomized into two groups (n=42 in PC, n=38 in PF). All PGA and control groups showed similar ocular surface and MG parameters at the baseline. Both PC- and PF-PGA groups showed increased meibum scores, meiboscores, and LASs at 12 months compared to the baseline (all p<0.05). At the 12-months visit, PC-PGA group showed severe OSDI, shorter TBUT, greater OSS, and worse MG parameters than those of the other two groups (all p<0.05). In addition, PF-PGA group showed worse meiboscores, meibum scores, and severe OSS scores than those of the control group (all p<0.05). Both PC and PF formulations can cause damage to the MG in patients using PGA. However, PC formulations induced more ocular discomfort, poorer ocular surface, and more severe MG loss compared to PF formulations. Therefore, it would be advisable to use PF formulations in patients with a preexisting or concomitant ocular surface disease or MGD.
Prostaglandin analogues (PGAs) have become the first-line option for the medical treatment of open-angle glaucoma (OAG) because of their superior 24-hour intraocular pressure (IOP) lowering effect, favorable systemic adverse profile, and convenient once-daily dosing.1 However, long-term use of PGAs is associated with ocular adverse effects including ocular discomfort, conjunctival hyperemia, keratopathy, dry eye disease, and blepharitis. In addition, meibomian gland dysfunction (MGD), which is characterized by an obstruction of the terminal ducts and qualitative/quantitative changes in glandular secretion, has been observed frequently in PGA-treated patients.2
Healthy meibomian glands (MGs) are essential for maintaining the stability of the ocular surface; MGD is associated with the tear film alteration, symptoms of irritation, clinically apparent inflammation, and ocular surface disease.3 Moreover, MGD can impact quality of life, compliance with medical treatment, and progression of glaucoma in medically treated glaucoma patients.4 In this regard, glaucoma management might be significantly improved by preserving the structural and functional integrity of MG while utilizing PGAs.
However, it is still debatable whether MGD in PGA users is induced by the active component, preservatives, or by both. Some studies have shown that MGD is more specific to PGAs than to other types of medications. Mocan et al.5 found that MGD prevalence was higher in patients treated with PGA monotherapy (92.0%) than those receiving non-PGA medications (58.3%), and the majority of MGD was of the obstructive type (95.7%). In addition, Cho et al.6 showed that, compared to PGAs, non-PGAs had a lower effect on MG dropout. However, other studies found that long-term use of glaucoma eye drops affected morphology and function of the meibomian gland, irrespective of the number or type of medication. Arita et al.7 reported similar meibomian gland dropout in PGA and beta-blocker treated eyes. It is speculated that rather than active components, preservative such as benzalkonium chloride (BAK) may exert a primary and dose-dependent toxic effect on MG. These findings are supported by multiple experimental and clinical studies that demonstrate that preservative free PGAs (PF-PGAs) induce lower MG damage than preservativecontaining PGAs (PC-PGAs).89
However, most previous studies did not provide the pretreatment status of MG in glaucoma patients, and changes in MG over the PGA treatment duration, owing to the cross-sectional design of these studies. Moreover, few studies have directly compared the morphology and function of MG between PC-PGA-treated and PF-PGA-treated patients. In this study, we aimed to compare the changes of the morphology and function of MG in OAG patients treated with PC-PGA or PF-PGA.
This is a retrospective analysis of medical records of patients with OAG (n=80) and healthy controls (n=40) who visited Chonnam National University Hospital, a tertiary referral eye center in Gwangju, South Korea, from 2017 to 2018. This study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Chonnam National University Hospital (IRB: CNUH-2018-289).
In total, 80 treatment-naïve OAG patients who received either PC-PGA (n=42) or PF-PGA (n=38) monotherapy for 1 year were included in this study. The PC-PGA group used either latanoprost (Xalatan®, Pfizer Inc., New York, USA) or tafluprost (Taflotan®, Santen Pharmaceutical Co, Ltd, Osaka, Japan), and the PF-PGA group used preservative free latanoprost (Monoprost®, Thea Pharmaceutical Co, Ltd, Clermont-Ferrand, France) or preservative free tafluprost (Taflotan-S®, Santen Pharmaceutical Co. Ltd, Osaka, Japan) in this study.
The exclusion criteria were as follows: previous history of ocular surgery, current use of contact lenses, history of recent ocular inflammation or infection, previous or current use of other ocular medications including artificial tear therapy, systemic treatments that are known to affect tear secretion, and any history or slit-lamp evidence of ocular surface disorders.
Normal controls were recruited from patients who came for a routine eye examination, patient relatives, and hospital staff. The inclusion criteria for the normal controls were as follows: healthy participants with no family history of glaucoma, no previous intraocular surgery, IOP <21 mmHg, and non-glaucomatous optic nerve head. The control group did not have clinical signs and/or symptoms of dry eye (Ocular surface disease index [OSDI] score <10) or significant ocular surface disease.
Participants were required to complete the ocular surface disease index (OSDI) questionnaire, which gives a score ranging from 0 (no symptoms) to 100 (severe symptoms).10
The interval between a complete blink and the appearance of the first dry spot after the instillation of fluorescein was recorded as the tear film break-up time (TBUT).11 The TBUT was measured three times, and the mean value was recorded (seconds).12 Ocular surface staining (OSS) was evaluated using the Oxford grading scale from 0 to 5 with increased significance.13 The Schirmer's test was performed by instilling one drop of proparacaine 0.5% anesthetic, placing a standard Schirmer's test strip between the lateral and middle third of the lower eyelid, and waiting for 5 minutes with the patient's eyes closed. The length of the wet strip was measured using the millimeter scale.
The meibomian gland evaluation consisted of the assessment of gland morphology (gland dropout), function (meibum expressibility and quality), and the lid margin. For evaluating gland dropout, infrared images of the upper lid MGs were recorded using Oculus Keratograph 5M (Oculus GmbH, Wetzlar, Germany) and the area of gland loss was measured with the ImageJ software (Java software program developed by the National Institutes of Health; available at http://rsb.info.nih.gov/ij),14 and its ratio to the total area was noted as the meiboscore (0–100%).15
To assess the expressbility and quality of meibum, the center of the upper tarsus was expressed with digital pressure, and the meibum score was graded as follows: 0 = clear meibum was easily expressed, 1=cloudy meibum was expressed with mild pressure, 2=cloudy meibum was expressed with more than moderate pressure, and 3=meibum could not be expressed even with hard pressure.11
The lid margin abnormality scores (LAS) were recorded based on the existence of the following four signs: lid margin irregularity, vascular engorgement, glandular orifices obstruction, and anterior or posterior displacement of the mucocutaneous junction. The eye was scored from 0 to 4.16
Primary outcome of this study was to compare the MG parameters among the three groups (PC-PGAs, PF-PGAs, and controls) at the 12-month visit. In addition, changes from the baseline values of ocular surface parameters and MG parameters were investigated in each group. Statistical analyses were conducted using SPSS version 19.0 (SPSS Institute Inc., Chicago, IL, USA). The data was described as the mean (±SD). Differences in the various parameters among the three groups were evaluated using the chi-square test and the one-way analysis of variance (ANOVA) with Bonferroni post hoc analysis. Comparison between baseline and follow-up visits in each group was performed using Paired t-test. A p value<0.05 was considered as statistically significant.
Demographic and clinical characteristics of participants are summarized in Table 1. There were no significant differences in age and sex among the three groups. Both PC-PGA and PF-PGA groups showed a higher IOP than that of the control group (p<0.001) but there were no differences in IOP values between the PC-PGA and PF-PGA groups (PC-PGA: 13.67±2.66 vs PF-PGA: 17.65±2.76; p=0.682) at baseline. The PGA eye drops comprised latanoprost (n=24), and tafluprost (n=18) in PC-PGA and latanoprost (n=20), and tafluprost (n=18) in PF-PGA groups; the difference was not statistically significant (p=0.221).
All three groups showed similar subjective symptoms, ocular surface evaluations, and MG parameters at baseline (Table 2).
After treatment, OSDI and OSS score were increased and TBUT was decreased in both PC-PGA and PF-PGA groups and reached significance at 12 months compared to the baseline (all p<0.05). However, there was no significant change in Schirmer's test results during the 12 months of follow-up in all three groups (Fig. 1).
In addition, both PC-PGA and PF-PGA groups showed an increase in meibum score, meiboscore, and LAS at 12 months compared to baseline (all p<0.05). Further, meibum score and meiboscore at 9 months of PC-PGA group were higher than those at baseline (p=0.02 and p=0.01; Fig. 2).
Comparing the three groups at the 12-month visit, the PC-PGA group showed severe OSDI, shorter TBUT, greater OSS, and worse MG parameters than those of the other two groups (all p<0.05). In addition, PF-PGA group also showed worse meiboscore, meibum score, and severe OSS score than those of the control group (all p<0.05; Table 3).
By comparing the effect of PC-PGA and PF-PGA on the MG in treatment-naïve participants in this study, we aimed to investigate whether the active component or the preservative could cause damage to the MG in PGA users. We observed that both PC-PGA and PF-PGA caused considerable damage to the ocular surface and the MG over 12 months of therapy. However, patients using PF-PGA had a more stable ocular surface and less severe MG damage than those of patients on PC-PGA. Our results suggest that both the active component and the preservative in PGA drops may contribute to MGD in PGA-treated patients.
Previous studies have revealed an association between MGD and PGA use. Cunniffe et al.17 reported a relatively high incidence of chalazion in patients on PGA. They postulated that topical PGA may contribute to the formation of chalazion by acting directly to stimulate or alter MG secretion. This can result in MGD features such as blepharitis, MG obstruction, chalazion, or secondary tear film abnormalities. Cho et al.6 reported that PGA might be the predominant IOP-lowering agent causing MGD. In their subgroup analysis comparing the patients under PGA monotherapy with those under combined PGA and other IOP-lowering agents, they found a shorter TBUT in the latter group but no significant difference in MG dropout. These results suggest that non-PGA medication may aggravate tear film instability, but PGA medication had a more notable effect than non-PGA medication. Our data also showed that both PC-PGA and PF-PGA induce an increase in meibum score and meiboscore at 12 months. This suggests that even without preservatives, the PGA active component itself can cause gland loss and poor expressibility and quality of meibum.
While the association of PGA with MGD has long been demonstrated, the mechanism underlying MGD induction by PGA remains unclear.5678 Mocan et al.5 suggested that prolonged exposure of the lid margin to topical PGA may induce keratinization of the MG acini along with the induction of hypertrichosis and periocular pigmentation, resulting in obstructive MGD. A recent in vivo confocal study by Agnifili et al.18 also proposed that drug-induced inflammation, allergy, and toxicity within the conjunctiva might diffuse contiguously to the tarsal and acinar units, leading to meibum stagnation followed by the keratinization of MG orifices. They suggest that the PGA active compound plays a key role in inducing MG alteration that mean area of acinar and density of the meibomian gland in patients treated with PC-PGA were less than those treated with PF-PGA and PC beta-blockers.
All PC-PGAs used in this study were BAK-preserved PGA and induced more severe damage to the ocular surface and MGs than that by PF-PGA. The most frequently used preservative, BAK, has been demonstrated to have toxic effects on many ocular structures in laboratory, experimental, and clinical studies.192021 It has been shown to cause tear film instability, loss of goblet cells, conjunctival squamous metaplasia and apoptosis, disruption of the corneal epithelium barrier, and damage to deeper ocular tissues.19 Regarding the impact of preservatives on MGs, in vitro studies have shown that cytotoxic effects of BAK on the human MG epithelial cells are apparent at very low concentrations (0.00001%) and in vivo confocal microscopy studies have indicated that acinar dropout and inflammation were much less evident in patients with low cumulative doses of preservatives.22 The potential mechanisms are toxicity and an inflammatory or immune-mediated response, with inflammation probably being the first step in the cascade of glandular modifications leading to acinar dropout.
The active compound of PGA and BAK may have synergistic effects on MGs in patients using PC-PGA. Agnifili et al.23 found that preserved drugs induced higher inflammatory reaction compared to overall PF formulations, but especially PC-PGAs induce more inflammation than PF-PGAs without significant differences between PC- and PF-β-blockers.51322
In addition to a direct toxic effect, BAK may enhance these effects of the PGA active component by promoting the drug's penetration into the glands.24 Since MGs are located in the tarsal plate of the eyelid, which is at a relatively deeper position than that of the superficial ocular surface, theoretically, resistance is higher in MGs than in superficial ocular structures. However, owing to BAK, toxicity and inflammation of the conjunctiva can easily diffuse into the MGs.
It is noteworthy that a statistically significant increase in meibum score and meiboscore appeared only after 9 months of treatment in both PC- and PF-PGA groups. MG alteration was concurrent with discomfort and damage to the ocular surface in patients receiving PGA in this study. Considering that glaucoma is a chronic disease, alteration of the MG occurring at 9 months is relatively early during treatment. Previous studies, and this study, have shown that obstructive MGD is the most common type after glaucoma medication. Furthermore, obstructive MGD responds to treatment with improvement of symptoms and OSS scores. Therefore, identification and treatment of MGD may be beneficial for PGA-treated patients. Further long-term studies are necessary to evaluate whether MGD progresses once the PGA is stopped.
There were some potential limitations to this study. First, this was a retrospective study performed in a single academic institute within a relatively brief period of treatment: therefore, we cannot provide data on the long-term effects of PGA on MGs and the ocular surface. Although most previous studies were cross-sectional in design, we tracked the changes on the ocular surface and MGs in treatment-naïve patients receiving PGA over 12 months. We believe that our data revealed the early course of ocular surface and MG damage with topical PGA therapy. Second, the concentrations of BAK in the two PGAs used in this study were different. The BAK concentrations of latanoprost and tafluprost were 0.02% and 0.001%, respectively, and latanoprost had a 20-fold higher concentration than that of tafluprost. Benzalkonium chloride is known to have dose-dependent detrimental effects on healthy ocular tissues; it can cause the arrest of cellular growth at 0.0001% and induce cellular apoptosis at 0.01%. However, in another clinical study of MG damage after using various PGAs, there was no significant difference in the MG area among patients with latanoprost (0.02% BAK), travoprost (0.001% polyquad), or bimatorpost (0.005% BAK).22 This suggests that 0.001% BAK was enough to induce MG damage and difference in the concentration of preservative may not be important in the analysis of our results.
In conclusion, both PC and PF formulations can cause damage in the MG in patients using PGA. However, compared to PF formulations, PC formulations induce more ocular discomfort and tear film instability, poorer ocular surface, and more severe MG loss. Therefore, the morphology and function of the MG should be assessed carefully before PGA treatment and it would be advisable to use PF formulations in patients with a preexisting or concomitant ocular surface disease or MGD, which are frequent in glaucoma patients.
Figures and Tables
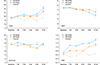 | FIG. 1Changes of ocular surface parameters during 12-months treatment. OSDI and OSS score were increased and TBUT was decreased in both PC-PGA and PF-PGA groups and reached significance at 12 months compared to the baseline (all *p<0.05). However, there was no significant change in Schirmer's test results during the 12 months of follow-up in all three groups. |
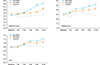 | FIG. 2Changes of meibomian gland parameters during 12-months treatment. Both PC-PGA and PF-PGA groups showed increased meibum score, meiboscore, and LAS at 12 months compared to baseline (all *p<0.05). Further, meibum score and meiboscore at 9 months of PC-PGA group were higher than those at baseline (p=0.02 and p=0.01). |
TABLE 3
Comparing the results of 12 months follow-up visits

Data are expressed as mean±standard deviation unless otherwise indicated. Bold font denotes significant. OSDI: ocular surface disease index, TBUT: tear film break-up time, OSS: ocular surface staining score, LAS: lid margin abnormality score. 1p value: PC-PGA vs PF-PGA. 2p value: PC-PGA vs Control. 3p value: PF-PGA vs Control.
References
1. Bean GW, Camras CB. Commercially available prostaglandin analogs for the reduction of intraocular pressure: similarities and differences. Surv Ophthalmol. 2008; 53 Suppl1:S69–S84.

2. Aydin Kurna S, Acikgoz S, Altun A, Ozbay N, Sengor T, Olcaysu OO. The effects of topical antiglaucoma drugs as monotherapy on the ocular surface: a prospective study. J Ophthalmol. 2014; 2014:460483.

3. Nichols KK, Foulks GN, Bron AJ, Glasgow BJ, Dogru M, Tsubota K, et al. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011; 52:1922–1929.

4. Lee TH, Sung MS, Heo H, Park SW. Association between meibomian gland dysfunction and compliance of topical prostaglandin analogs in patients with normal tension glaucoma. PLoS One. 2018; 13:e0191398.

5. Mocan MC, Uzunosmanoglu E, Kocabeyoglu S, Karakaya J, Irkec M. The association of chronic topical prostaglandin analog use with meibomian gland dysfunction. J Glaucoma. 2016; 25:770–774.

6. Cho WH, Lai IC, Fang PC, Chien CC, Tseng SL, Lai YH, et al. Meibomian gland performance in glaucomatous patients with long-term instillation of IOP-lowering medications. J Glaucoma. 2018; 27:176–183.

7. Arita R, Itoh K, Maeda S, Maeda K, Furuta A, Tomidokoro A, et al. Effects of long-term topical anti-glaucoma medications on meibomian glands. Graefes Arch Clin Exp Ophthalmol. 2012; 250:1181–1185.

8. Rath A, Eichhorn M, Träger K, Paulsen F, Hampel U. In vitro effects of benzalkonium chloride and prostaglandins on human meibomian gland epithelial cells. Ann Anat. 2019; 222:129–138.

9. Baudouin C, Liang H, Hamard P, Riancho L, Creuzot-Garcher C, Warnet JM, et al. The ocular surface of glaucoma patients treated over the long term expresses inflammatory markers related to both T-helper 1 and T-helper 2 pathways. Ophthalmology. 2008; 115:109–115.

10. Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000; 118:615–621.

11. Shimazaki J, Goto E, Ono M, Shimmura S, Tsubota K. Meibomian gland dysfunction in patients with Sjögren syndrome. Ophthalmology. 1998; 105:1485–1488.

12. Rabinowitz MP, Katz LJ, Moster MR, Myers JS, Pro MJ, Spaeth GL, et al. Unilateral prostaglandin-associated periorbitopathy: a syndrome involving upper eyelid retraction distinguishable from the aging sunken eyelid. Ophthalmic Plast Reconstr Surg. 2015; 31:373–378.
13. Arita R, Itoh K, Maeda S, Maeda K, Furuta A, Tomidokoro A, et al. Comparison of the long-term effects of various topical antiglaucoma medications on meibomian glands. Cornea. 2012; 31:1229–1234.

14. Ban Y, Shimazaki-Den S, Tsubota K, Shimazaki J. Morphological evaluation of meibomian glands using noncontact infrared meibography. Ocul Surf. 2013; 11:47–53.

15. Arita R, Suehiro J, Haraguchi T, Shirakawa R, Tokoro H, Amano S. Objective image analysis of the meibomian gland area. Br J Ophthalmol. 2014; 98:746–755.

16. Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology. 2008; 115:911–915.

17. Cunniffe MG, Medel-Jiménez R, González-Candial M. Topical antiglaucoma treatment with prostaglandin analogues may precipitate meibomian gland disease. Ophthalmic Plast Reconstr Surg. 2011; 27:e128–e129.

18. Agnifili L, Fasanella V, Costagliola C, Ciabattoni C, Mastropasqua R, Frezzotti P, et al. In vivo confocal microscopy of meibomian glands in glaucoma. Br J Ophthalmol. 2013; 97:343–349.

19. Baudouin C, Labbé A, Liang H, Pauly A, Brignole-Baudouin F. Preservatives in eyedrops: the good, the bad and the ugly. Prog Retin Eye Res. 2010; 29:312–334.

20. Steven DW, Alaghband P, Lim KS. Preservatives in glaucoma medication. Br J Ophthalmol. 2018; 102:1497–1503.
21. Lee W, Lee S, Bae H, Kim CY, Seong GJ. Efficacy and tolerability of preservative-free 0.0015% tafluprost in glaucoma patients: a prospective crossover study. BMC Ophthalmol. 2017; 17:61.

22. Fasanella V, Agnifili L, Mastropasqua R, Brescia L, Di Staso F, Ciancaglini M, et al. In vivo laser scanning confocal microscopy of human meibomian glands in aging and ocular surface diseases. Biomed Res Int. 2016; 2016:7432131.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download