This article has been
cited by other articles in ScienceCentral.
Abstract
This study identified the explanatory power of the Korean rehabilitation patient group (KRPG) v1.1 for acquired brain injury (ABI) on medical expenses in the rehabilitation hospitals and the correlation of functional outcomes with the expenses. Here, the design is a retrospective analysis from the claim data of the designated rehabilitation hospitals. Data including KRPG information with functional status and medical expenses were collected from 1 January and 31 August 2018. Reduction of variance (R2) was statistically analyzed for the explanation power of the KRPG. Association between functional status and the medical expenses was carried out using the Spearman's rank order correlation (rho). From the claim data of 365 patients with ABI, the KRPG v1.1 explained 8.6% of variance for the total medical expenses and also explained 9.8% of variance for the rehabilitation therapy costs. Cognitive function and spasticity showed very weak correlation with the total medical expenses (rho = −0.17 and −0.14, respectively). Motor power and performance of activities of daily living were associated weakly (rho = −0.27 and −0.30, respectively). The KRPG and related functional status in ABI reflects the total medical expenses and rehabilitation therapy costs insufficiently in the designated rehabilitation hospitals. Thus, the current KRPG algorithm and variables for ABI may need to be ameliorated in the future.
Highlights
• The KRPG v1.1 explained 8.6% of variance for the total medical expenses of rehabilitation inpatients and also explained 9.8% of variance for the rehabilitation therapy costs from the claim data of the designated rehabilitation hospitals.
• The KRPG and related functional items for the patients with ABI reflects the total medical expenses and rehabilitation therapy costs insufficiently.
• The current KRPG algorithm and variables for the ABI may need to be ameliorated in the future.
Keywords: Diagnosis-Related Groups, Fee-for-Service Plans, Neurological Rehabilitation, Brain Diseases
INTRODUCTION
The patient classification system sorts patients to the groups homogeneous in use of resources and similar in clinical characteristics according to their diagnoses, procedures, functions, etc. This case-mix information can be used as the basis for reimbursement, and also for comparing the medical programs, practice patterns, and patient outcomes of medical institutions.
Even though the Korean diagnosis related group (KDRG) and the Korean out-patient group (KOPG) are the representative patient grouping system in the republic of Korea, they are for the acute patients and have lack of validity for the rehabilitation patients in subacute phase. In acute medical or surgical episodes, the majority of medical expenses are incurred within the early period of hospital stay and tail off thereafter, while in the rehabilitation phase the cost curve is largely flat throughout the length of stay [
1].
It is well-known that rehabilitation poses particular challenges for the development of case-mix system; therefore, some countries have developed an independent rehabilitation patient classification system after acute medical or surgical period. For example, the United States uses the case-mix groups (CMGs), Australia has the Australian National Subacute and Non-Acute Patient Case-mix Classification (AN-SNAP), and Canada makes use of the rehabilitation patient groups (RPG) [
123].
In Korea, as the elderly population increases rapidly, a necessity for the novel rehabilitation patient classification system and designated rehabilitation hospitals has been raised to establish the national rehabilitation delivery system after the acute period.
In 2015, the Health Insurance Review & Assessment Service (HIRA) had developed the first version of the Korean rehabilitation patient group (KRPG) focused on the patients with central nervous system lesion through the consultation with the Korean Academy of Rehabilitation Medicine and the National Rehabilitation Center. Then, the pilot project of rehabilitation hospital designation has also launched in accordance with the Act on Guarantee of Right to Health and Access to Medical Services for Persons with Disabilities in 2017.
The HIRA revised the first version of KRPG to version 1.1 prior to the pilot project with the addition of the Korean rehabilitation impairment category (KRIC) for musculoskeletal and amputation patients in early 2017. However, the additional grouping of KRPG v1.1 except for the existing grouping for central nervous system lesion is very flimsy and divided only by the age of patient. This is partly due to the fact that only the acquired brain injury (ABI) accounts for the majority of the rehabilitation inpatients with its devastating complications and is covered better by the National Health Insurance than other impairments rehabilitation in Korea [
4]. Patients with brain injury are classified into 204 disease groups. The number of subdivided disease groups of stroke (Korean Rehabilitation Impairment Category, or KRIC 01), traumatic brain injury (KRIC 02), and non-traumatic brain injury (KRIC 03) are 32, 32, and 32 respectively. Then, the pilot project does not yet have its own reimbursement system; HIRA would develop the unique payment model to promote the rehabilitation in the period of convalescence with the information of KRPG v1.1 from the designated rehabilitation hospitals.
So, the purpose of this study was to investigate the explanatory power of KRPG v1.1 for acquired brain injury on medical expenses in the designated hospitals and to identify the correlation of functional outcomes with the expenses. This will show how the current rehabilitation patient classification system in Korea reflects the costs and related functional status of inpatient rehabilitation.
MATERIALS AND METHODS
Subjects
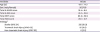
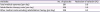
Data were collected from all patients who were subject to the pilot project of implementation of designated rehabilitation hospitals; 18 years of age or older within 90 days after onset or surgery during an 8-month period between 1 January and 31 August 2018. A total of 365 patients (207 males and 158 females) whose etiologic diseases were classified as stroke (KRIC 01), traumatic brain injury (KRIC 02), or non-traumatic brain injury (KRIC 03) confirmed by computed tomography or magnetic resonance imaging were included. Subjects with 1) the underlying neurological conditions other than ABI such as degenerative brain diseases (KRIC 04), multiple trauma with brain and spinal cord injury (KRIC 07), cerebral palsy (KRIC 09), or other diseases of central nervous system (KRIC 10) were excluded. Demographic details are presented in
Table 1.
Table 1
Demographics and clinical characteristics of the study population (n = 365)
|
Variables |
Values |
|
Age (yr) |
67.1 ± 14.3 |
|
Sex (male/female) |
207/158 |
|
Total K-MMSE score |
18.4 ± 8.6 |
|
Total K-MBI score |
41.0 ± 25.8 |
|
Total MMT score |
92.8 ± 26.9 |
|
Total MAS score |
29.1 ± 21.7 |
|
Etiology*
|
|
|
Stroke (KRIC 01) |
332 (91.0) |
|
Traumatic brain injury (KRIC 02) |
25 (6.9) |
|
Non-traumatic brain injury (KRIC 03) |
8 (2.2) |

Setting
The designated rehabilitation hospitals by the Ministry of Health and Welfare provide the patients of central nervous system lesion with a comprehensive rehabilitation service for at least 6 months. We collected the data from the six designated rehabilitation hospitals located in Seoul, Gyeonggi-do, Gangwon-do, and Pusan.
Variables
Independent variables examined in the study were criterion measures of KRPG v1.1 and the medical expenses. Classification variables of KRPG v1.1 were composed of age, Korean version of Mini-Mental State Exam (K-MMSE), total K-MBI (Korean version of modified Barthel Index, total MMT (manual muscle testing), and total MAS (modified Ashworth scale) scores at admission. All the items were based on standardized evaluation tools of the KRPG algorithm [
5].
For the costs during admission episode, total medical expenses per day and rehabilitation therapy costs per day of each subject were collected. The total medical expenses were indicated as the entire costs during hospitalization including both reimbursement and non-reimbursement payment. The rehabilitation therapy costs were defined as the sum of both reimbursement and non-reimbursement payments for rehabilitation fee mainly based on Chapter 7 of the National Health Insurance's fee schedule.
Dependent variables were predictive validity and explanatory power of KRPG v1.1.
Data collection and statistical analysis
Data were extracted from the raw claim data of the designated hospitals. The analysis was processed with the SAS, version 9.4, software (SAS institute, Cary, NC, USA) using traditional methods within the outline recommended by Medical Outcome Trust [
6].
We examined the predictive validity of the 5 classification variables of KRPG v1.1 using the Spearman rank correlation coefficient (rho). Correlation between functional status assessed by age, K-MMSE, K-MBI, MMT, and MAS scores at admission and in-hospital costs such as total medical expenses per day and rehabilitation therapy costs per day were investigated, respectively. In addition, we examined the coefficient of determination or the reduction of variance (R2) of the KRPGv1.1 with respect to the total medical expenses per day and rehabilitation therapy costs per day. R2 explains how much variance of the data is “explained” by the model. “To explain” means to reduce the residual variance. Thus, the coefficient of determination is the ratio of explained variance to the total variance that tells about the strength of association between the variables.
yi: medical expenses for the i th patient
A: Overall average value of medical expenses
Ag: Average value of medical expenses in the g group
For the total medical expenses per day and the rehabilitation therapy costs per day, the statistical analysis began by removing all observed values more than 1.5 interquartile ranges (IQR) above the 75th percentile or below the 25th percentile. The Spearman's correlation and coefficient of determination of the trimmed sample were then used for the final analysis as to predictive validity and explanatory power.
Ethical considerations
This study was approved by the Institutional Review Board of National Traffic Injury Rehabilitation Hospital (No. NTRH-19005). It was conducted in accordance with the Declaration of Helsinki.
RESULTS
The KRPG v1.1 was applied to the patient demographics and functional status data collected in this study. Total 365 patients of 34 groups with acquired brain injury (KRIC 01, 02, 03) were recruited. Among them, 332 stroke (KRIC 01) patients of 19 groups accounted for 91.0%. Demographics and clinical characteristics of patients were as shown in
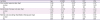
Table 1. After trimming 1.5 IQR for cost outliers, 281 and 229 subjects were analyzed for predictive validity and explanatory power of KRPG v1.1 in terms of the total medical expenses per day and the rehabilitation therapy costs per day, respectively (
Tables 2 and
3).
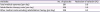
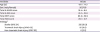
Table 2
Evaluation results of KRPG version 1.1 after trimming 1.5 IQR for outliers
|
Variables |
No. of episodes |
Reduction of variation (%) |
|
Total medical expenses (per day) |
281 |
8.6 |
|
Rehabilitation therapy costs (per day) |
229 |
9.8 |
|
Other medical costs excluding rehabilitation therapy (per day) |
229 |
8.3 |

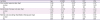
Table 3
Correlations between the charges for inpatient rehabilitation and functional status variables of KRPG v1.1 after trimming 1.5 IQR for outliers
|
Variables |
Age |
K-MMSE |
K-MBI |
MMT |
MAS |
|
Total medical expenses (per day) |
0.58 |
−0.17*
|
−0.30*
|
−0.27*
|
−0.14*
|
|
p value |
0.33 |
0.00 |
0.00 |
0.00 |
0.00 |
|
No. |
281 |
281 |
281 |
281 |
281 |
|
Rehabilitation therapy costs (per day) |
−0.00 |
−0.078 |
−0.22*
|
−0.18*
|
−0.03 |
|
p value |
0.95 |
0.24 |
0.00 |
0.01 |
0.62 |
|
No. |
229 |
229 |
229 |
229 |
229 |
|
Medical costs excluding rehabilitation therapy (per day) |
0.10 |
−0.12 |
−0.16†
|
−0.14†
|
−0.15†
|
|
p value |
0.14 |
0.08 |
0.12 |
0.04 |
0.02 |
|
No. |
229 |
229 |
229 |
229 |
229 |

Predictive validity of KRPG v1.1
Classification variables of KRPG v1.1 showed little correlation with either total medical expenses per day or rehabilitation therapy costs per day. Age of the patient was not correlated with the medical expenses. Cognitive function (MMSE) and spasticity (MAS) were found to have a very weak correlation with total medical expenses per day (rho = −0.17 and −0.14, p < 0.01, respectively), and motor power and performance of activities of daily living was associated weakly with the total medical expenses per day (rho = −0.27 and −0.30, p < 0.01, respectively) (
Table 3). In terms of rehabilitation therapy cost, motor power and performance of activities of daily living showed very weak and weak correlations (rho = −0.18 and −0.22, p < 0.05, respectively) (
Table 3).
Explanatory power of KRPG v1.1
The KRPG v1.1, which include age, K-MMSE, K-MBI, MMT, and MAS yielded an R
2 = 0.086 for the total medical expenses per day and an R
2 = 0.098 for the rehabilitation therapy costs per day in terms of inpatient rehabilitation of the patients with ABI (
Table 2).
DISCUSSION
In this study, the KRPG v1.1 was applied to the patients with ABI corresponding to KRIC 01, 02, 03 and as a performance outcome measure of the PCS (case-mix system) the explanatory power on the medical expenses was 8.6%, similar to 11.8% reported by Hwang et al. [
5] in 2016. In addition, as classification variables the functional status of the patients with ABI have very weak or weak association with the medical expenses, and which is consistent with previous studies [
7]. This means that KRPG does not sufficiently reflect the resource consumption during medical rehabilitation phase. It is derived from the fact that the KRPG has been developed based on the clinical aspects rather than the resource consumption or rehabilitation needs, and this is also owing to the low contributions and a limited benefits design of the National Health Insurance.
In 2016, when developing the KRPG v1.0, Hwang et al. analyzed the three-year claims from 2011 and retrospective medical records of 42 hospitals active in medical rehabilitation. Then, they explained the variance in total charge for inpatient rehabilitation with 9 KRIC (204 number of groups) of KRPG v1.0. However, because it is based on the retrospective medical record review, the patients were biased by some of chronic phase without any criteria related to the lag-time from the onset to admission, and the data may be incomplete and imprecise without standardized scheme. In addition, they could have collect only the reimbursement expenses by the National Health Insurance without non-reimbursement payment data from the hospitals, so they could not reflect the real expenses for the medical rehabilitation.
KRPG v1.1 used in our study is the latest revision of the existing KRPG v1.0 with 15 KRICs and subgroups including musculoskeletal injuries and fractures, but there was no change in the classification of patients with ABI corresponding to KRIC 01, 02, 03.
The admission criteria to the designated rehabilitation hospitals are somewhat strict to the patient with ABI; they must be admitted to the rehabilitation hospital within 3 months from the ictus, and then, they are guaranteed for at least six months of hospital stay. In addition, the dedicated hospitals are obliged to collect and to report the standardized form about the functional status of patients with claim data. So, our study could have use a standardized data-set from the pilot project of subacute phase requiring more intensive rehabilitation therapy and medical care. Besides, not only the medical costs reimbursed from the National Health Insurance but also non-reimbursement payment data were completely collected and analyzed directly from the hospital participating in the project. Our data may reflect the current status of subacute comprehensive inpatient rehabilitation better than the previous study.
The limitation of this study is that it did not include all the designated rehabilitation hospitals (15 of total) participating in the pilot project, and the periods of collecting episodes were relatively short of about 8 months. Although the number of patients of our study is sufficient to statistical analysis, it is desirable to include a larger number of patients over a longer period of time considering regional distribution of the hospitals.
Nevertheless, it is meaningful that KRPG v1.1 was used and analyzed for the first time to confirm the patient composition and how they explain the variance in the medical expense from the first pilot project of the 'designated rehabilitation hospital' according to the Act on Right to Health for Persons with Disabilities.
The KRPG is an independent rehabilitation patient classification system that is separate from the acute phase patient classification system such as KDRG and KOPG. It classifies the rehabilitation patients considering age and several functional statuses in the major rehabilitation impairment category similar to USA and Australia [
1,
3].
In United States (CMG) and Australia (AN-SNAP), the aspect of resource consumption to increase the accuracy of the payment model of the medical care is considered with more importance. They have use only the FIM scores as a functional assessment variable, whereas the KRPG values on clinical characteristics of the rehabilitation patient and includes age and various functional assessment items (e.g. K-MMSE, MMT, K-MBI, and MAS in ABI) as classification variables. The each item of functional status showed little association with the medical costs, and consequently grouping algorithm results in the excessive granularity and low explanatory power on the medical expenses and rehabilitation therapy costs.
According to Turner-Stokes et al. [
1], the case-mix system should be simple and timely for the prompt application by medical staff in the clinical field, and it should reflect well on the cost-determinants of the major resources for a fair payment on the treatment with the complexity of inquiries. In addition, the completeness of the patient classification system depends on not only the similarity of resource consumption but also the clinical similarity of the patient grouping, and which are the key to the development of optimal PCS [
8].
The KRPG v1.1 is newly developed for the rehabilitation patient classification and it has been started to be practically utilized through the ‘designated rehabilitation hospitals,’ it might be necessary to improve or complement the KRPG with considering the clinical resource allocation according to rehabilitation needs of the patients. Besides, the case-mix information such as KRPG is the basic data that can be used to establish the healthcare system and policies. Multidisciplinary rehabilitation specialists need to make efforts to know and improve the classification system.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download