This article has been
cited by other articles in ScienceCentral.
Abstract
Central odontogenic fibroma (COF) is defined as a fibroblastic odontogenic tumor characterized by varying density of the tooth epithelium. It is an extremely rare benign neoplasm that occurs in the maxilla and the mandible; only a few reports of COF are available in the literature. Diagnosis of the lesion based only on the radiological features of COF is difficult due to variation in the findings regarding this condition. This report describes 2 clinical cases of middle-aged women with COF. Clinical examination revealed palatal mucosal depression; additionally, oral examination, as well as panoramic radiographs, intraoral radiographs, and computed tomography scans, revealed severe root resorption. This report highlights the clinical and radiological imaging features of COF, with the goal of enabling straightforward differential diagnosis of the lesion by the clinician and thereby appropriate treatment of the patient.
Keywords: Benign Tumor, Diagnosis, Differential, Myxofibroma, Odontogenic Tumors
Central odontogenic fibroma (COF) is a rare benign tumor of the jawbones, accounting for less than 0.1% of all odontogenic tumors.
1 The World Health Organization (WHO) defines COF as a fibroblastic neoplasm that contains variable amounts of inactive odontogenic epithelium embedded in mature fibrous stroma. Since 1992, COFs have been classified into 2 types according to their histological features: the epithelium-poor type (formerly known as the simple type) and the epithelium-rich (WHO) type.
2 The epithelium-poor type contains mature fibrous tissue with sparsely scattered odontogenic epithelial nests, whereas the epithelium-rich type is more cellular, has more epithelial nests, and may contain calcifications that resemble dysplastic dentin, the cementum, or osteoid tissue.
COF has a slow, persistent growth rate that leads to asymptomatic buccal or lingual cortical plate expansion. It occurs more frequently in women than in men.
3 Clinically, the tumor occurs in the mandible and the maxilla with equal frequency. In the maxilla, it typically appears in the anterior region, whereas in the mandible, it tends to be located in the posterior region.
4 It is often accompanied by a palatal depression, which indicates progression of the osteolytic change.
56 On radiographs, the lesion appears as a well-defined unilocular or multilocular radiolucent lesion.
7 The lesion grows slowly in the bone without perforating the thin cortical outline of the anatomical structures, thereby preserving them. Root resorption of the associated teeth is frequent, and the lesion, when located between the teeth, often causes root divergence. In general, the treatment approach for the tumor is surgical excision, and the tumor lacks a tendency for malignant transformation.
In this report, we describe our experience with 2 cases of middle-aged female patients with COF in the anterior maxillary region, and we discuss the clinical, radiological, and histological features that enabled the differential diagnosis.
Case Report
Case 1
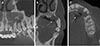
A 47-year-old female patient was referred to the Kyung Hee University Dental Hospital for further evaluation and treatment of a radiolucent lesion on the left maxillary lateral incisor. Upon oral examination at the time of the hospital visit, a soft-tissue depression of the left palatal mucosa of the left lateral incisor and canine area was revealed. No signs of inflammation were present, and no response to palpation around the area of the lesion was noted (
Fig. 1). The percussion test was positive, and changes in the mobility of the teeth were observed. Panoramic radiographs showed a poorly-defined radiolucent lesion with an irregular border extending from the left maxillary lateral incisor to the first premolar region. The tumor extended into the alveolar ridge (
Fig. 2A). Intraoral radiographs displayed significant resorption of the roots of the involved teeth (
Fig. 2B). Cone-beam computed tomographic (CBCT) images revealed the presence of an osteolytic lesion with an undulating border around the upper left anterior area, as well as external root resorption of the involved tooth, destruction of the palatal cortical bone, and thinning of the bone on the labial side; however, expansion of the bone in the labio-palatal direction was absent, and a shadow around the area of the palatal mucosal depression was observed (
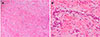
Fig. 3). Based on the radiographic findings of an ill-defined border and invasive bony destruction, clinicians considered minor salivary gland malignancy or a benign odontogenic tumor with strong osteolytic activity sufficient to cause root resorption in the diagnosis, and surgical enucleation was performed accordingly. The results of the histopathological examination revealed islands of odontogenic epithelial cells present in fibrous connective tissue without calcification. A smaller amount of scattered odontogenic epithelium than that usually found in ameloblastomas was present without signs of polarization in the cells (
Fig. 4). Based on these findings, the lesion was diagnosed as COF.
Case 2
A 50-year-old female patient presenting chiefly with a radiolucent lesion in the left maxillary premolar area was referred to the Kyung Hee University Dental Hospital. The patient was unable to feel the presence of the lesion or associated pain. Oral examination revealed soft-tissue depression of the palatal mucosa at the left lateral incisor and canine. Signs of inflammation, such as swelling, drainage, edema, or redness, were absent. Responses to percussion and palpation were within the normal range. Panoramic radiographs displayed a well-defined unilocular radiolucent lesion extending from the left maxillary canine to the region of the first premolar, along with significant resorption of the first premolar root (
Fig. 5). CBCT images showed a unilocular radiolucent lesion with a circumferential border and thin cortication extending to the alveolar ridge of the lateral canine and the first premolar, and external root resorption of the involved teeth was clearly visualized. Moreover, the images showed destruction of the cortical bone of the palate and thinning of the labial cortical bone. Depression of the soft tissue was observed at the perforation site (
Fig. 6). Based on a tentative diagnosis of an infected radicular cyst, surgical enucleation was performed. The results of the histopathological examination of the lesion revealed the presence of scattered odontogenic epithelial cells in fibrous connective tissue, and the lesion was confirmed as COF (
Fig. 7).
Discussion
COF is very rare, accounting for less than 0.1% of all odontogenic tumors, as reported in a previous study.
8 While COF occurs in patients within a wide age range, it is diagnosed most frequently between the second and fourth decades of life. A previous study reported its occurrence in 49 of 70 women (70%), with a mandible-to-maxilla ratio of 1:1 and no change at the respective site in the jaws; in these patients, COF appeared as a multilocular radiolucent lesion with well-defined borders. In some cases, COF may show a mixed radiolucent/radiopaque (12%) appearance with poorly defined or diffuse borders.
9 Findings obtained from both conventional radiographs and CT images are nonspecific for COF. According to previous reports, variability in the radiological appearance of COF made differential diagnosis difficult.
8 Magnetic resonance imaging (MRI) studies of COF revealed characteristic findings of homogeneous isointensity on T1-weighted images, isointensity to hyperintensity on short T1 inversion recovery images, and heterogeneous strong enhancement on contrast-enhanced T1-weighted images that were similar to images of odontogenic tumors, but that were still considered useful for differentiating them from jawbone cysts. Dynamic contrast-enhanced MRI was useful in differentiating COF from some benign tumor types, such as ameloblastoma and odontogenic myxoma.
10
In this report, case 1 presented the clinical and radiological features of a crater-like depression in the palate and ill-defined bony destruction, respectively, which suggested a malignant tumor. Radiographs showed prominent external root resorption of the 3 teeth affected by the lesion, which was considered an exceptional finding because malignant tumors of the jaw generally do not cause root resorption due to the highly rapid rate of tumor invasion.
11 Case 2 showed radiographic findings of cystic lesions around the apical region, indicating the presence of an infected radicular cyst and an adenomatoid odontogenic tumor of the extrafollicular type. However, the definitive diagnosis of an inflammatory odontogenic cyst should take into account the presence of other possible features. Our patient displayed invasive cortical loss, considered an unusual radiographic feature of an odontogenic cyst, and no clear etiologic factor of inflammation was identified; therefore, the authors were unable to exclude other possibilities.
Clinically, COF tumors are usually asymptomatic and are detected incidentally before the patient perceives the lesion. Patients usually become aware of significant tooth mobility and depression of the palatal mucosa at an advanced stage of the disease in which osteolysis has progressed to encompass a larger volume. Previously, some authors have described cases of palatal mucosal depression around the tumor
459 and soft-tissue depression of the palate. Clinically, other fibroblastic tumors demonstrate osseous swelling through the expanding jaw bones, whereas fibroblastic tumors related to COF show soft-tissue depression of the palate. Hirshber et al.
12 differentiated between hyperplastic dental follicle and COF by performing Picrosirius red staining of the lesion to visualize the polarity of collagen fibrils; they reported that the collagen-rich structure of COF was loosely arranged and comprised several premature collagen components. This histological characteristic of COF suggests replacement of the bone by the lesion and development of a palatal mucosal depression.
Radiography indicates that growth of COF located along the inside of the jaw causes thinning of the cortical plate and maintains the margin of the cortical bone, which suggests non-aggressive behavior of COF compared to that of other odontogenic lesions. Iordanidis et al.
13 conducted analyses using immunochemical staining and electron microscopy, and they reported that the number of myofibroblasts (MFs) was significantly lower in COF than in other odontogenic tumors. Previous studies evaluating the mean number of MFs in some odontogenic cysts and tumors have reported a positive correlation between the number of MFs and the biological behavior of these lesions; accordingly, the presence of a low number of MFs in the stroma predicts less aggressive behavior of the odontogenic cyst or tumor.
14 The findings regarding the lack of massive bony swelling and preservation of the cortical bone could be explained by the non-aggressive biological behavior of COFs.
15
Radiologically, a high growth rate of COF is associated with the presence of root resorption. Kaffe and Buchner
9 reported 51 case reviews of patients with COFs, among which external root resorption was present in 29% of the lesions. Another study reported root resorption in 11 of 39 cases of COF
5 and external root resorption of the involved teeth in all 11 of those cases; however, no histological studies exist to explain this finding. The fibroblastic cells that replace the bone within the lesion or the metabolic products from the patient's immune response may have the potential to mediate absorption of the bone as well as the root. Root resorption at the dental area of the tumor site is a key consideration in the differential diagnosis; therefore, clinicians should consider the impact of the tumor on the root.
In both of our patients, the histological findings of the enucleated tissues were consistent with a diagnosis of COF, as they displayed inactive odontogenic epithelial cells scattered in the fibrous connective tissue. Based on the World Health Organization definition (2005) of an odontogenic tumor, the presence of inactive odontogenic epithelia is a prerequisite for the diagnosis of COF. In general, COF of the epithelium-rich type has a greater proportion of fibroblasts and odontogenic epithelium than that of the epithelium-poor type.
16 Only a few reports of COF of the epithelium-poor type are available in the literature. However, immunohistochemical staining or ultrastructure analysis cannot distinguish between the 2 types of COF. Therefore, investigators should consider that any single COF entity may exhibit 2 different histological patterns.
17
In conclusion, COF is a very rare neoplasm occurring in the maxilla or mandible. It presents characteristic features of palatal soft-tissue depression of the affected tooth without any specific etiology, asymptomatic infrabony swelling with preservation of the thin cortical outline of the buccal/labial cortical plates, and external root resorption of the affected teeth. Due to the rarity of the lesion, clinicians or radiologists may misdiagnose COF as a malignant tumor or a periapical lesion. Accurate diagnosis may be achieved using an integrated approach that includes an assessment of all available clinical and radiological information.
Acknowledgements
The authors thank Young-Ah Cho, former Assistant Professor of the Department of Oral and Maxillofacial Pathology, Kyung Hee University Graduate School, for guidance in the histological evaluation and editing of the manuscript.
References
1. Wesley RK, Wysocki GP, Mintz SM. The central odontogenic fibroma. Clinical and morphologic studies. Oral Surg Oral Med Oral Pathol. 1975; 40:235–245.
2. Philipsen HP, Reichart PA. Classification of odontogenic tumours. A historical review. J Oral Pathol Med. 2006; 35:525–529.

3. Covani U, Crespi R, Perrini N, Barone A. Central odontogenic fibroma: a case report. Med Oral Patol Oral Cir Bucal. 2005; 10 Suppl 2:E154–E157.
4. Ramer M, Buonocore P, Krost B. Central odontogenic fibroma - report of a case and review of the literature. Periodontal Clin Investig. 2002; 24:27–30.
5. Handlers JP, Abrams AM, Melrose RJ, Danforth R. Central odontogenic fibroma: clinicopathologic features of 19 cases and review of the literature. J Oral Maxillofac Surg. 1991; 49:46–54.

6. Huey MW, Bramwell JD, Hutter JW, Kratochvil FJ. Central odontogenic fibroma mimicking a lesion of endodontic origin. J Endod. 1995; 21:625–627.

7. Rebai-Chabchoub N, Marbaix E, Iriarte Ortabe JI, Reychler H. Central odontogenic fibroma. Rev Stomatol Chir Maxillofac. 1993; 94:271–275.
8. Daniels JS. Central odontogenic fibroma of mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:295–300.

9. Kaffe I, Buchner A. Radiologic features of central odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1994; 78:811–818.

10. Hara M, Matsuzaki H, Katase N, Yanagi Y, Unetsubo T, Asaumi J, et al. Central odontogenic fibroma of the jawbone: 2 case reports describing its imaging features and an analysis of its DCE-MRI findings. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:e51–e58.

11. Kawai N, Wakasa T, Asaumi J, Kishi K. A radiographic study on resorption of tooth root associated with malignant tumors. Oral Radiol. 2000; 16:55–65.

12. Hirschberg A, Buchner A, Dayan D. The central odontogenic fibroma and the hyperplastic dental follicle: study with Picrosirius red and polarizing microscopy. J Oral Pathol Med. 1996; 25:125–127.

13. Iordanidis S, Poulopoulos A, Epivatianos A, Zouloumis L. Central odontogenic fibroma: report of case with immunohistochemical study. Indian J Dent Res. 2013; 24:753–755.

14. Vered M, Shohat I, Buchner A, Dayan D. Myofibroblasts in stroma of odontogenic cysts and tumors can contribute to variations in the biological behavior of lesions. Oral Oncol. 2005; 41:1028–1033.

15. Cercadillo-Ibarguren I, Berini-Aytés L, Marco-Molina V, Gay-Escoda C. Locally aggressive central odontogenic fibroma associated to an inflammatory cyst: a clinical, histological and immunohistochemical study. J Oral Pathol Med. 2006; 35:513–516.

16. Veeravarmal V, Madhavan RN, Nassar MM, Amsaveni R. Central odontogenic fibroma of the maxilla. J Oral Maxillofac Pathol. 2013; 17:319.

17. Mosqueda-Taylor A, Martínez-Mata G, Carlos-Bregni R, Vargas PA, Toral-Rizo V, Cano-Valdéz AM, et al. Central odontogenic fibroma: new findings and report of a multicentric collaborative study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112:349–358.









 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download