Abstract
Purpose
The aim of this study was to determine the reasons and solutions for intraoral phosphor storage plate (PSP) image artifacts and errors, and to develop an appropriate classification of the artifacts.
Materials and Methods
This study involved the retrospective examination of 5,000 intraoral images that had been obtained using a phosphor plate system. Image artifacts were examined on the radiographs and classified according to possible causative factors.
Results
Artifacts were observed in 1,822 of the 5,000 images. After examination of the images, the errors were divided into 6 groups based on their causes, as follows: images with operator errors, superposition of undesirable structures, ambient light errors, plate artifacts (physical deformations and contamination), scanner artifacts, and software artifacts. The groups were then re-examined and divided into 45 subheadings.
In the practice of dental radiology, the use of digital intraoral imaging systems has become increasingly common from the 1980s to the present day, especially with recent developments in technology. The first intraoral phosphor storage plate (PSP) (Digora, Orion Co./Soredex, Helsinki, Finland) system was introduced in 1994.1 These systems include PSPs that are stimulated by light, a scanner that scans PSP data after exposure, a computer to record the data, and a software program for image processing.
PSP systems, which use digital radiology technology, are preferred over traditional radiology because of features such as lower radiation doses and higher acquisition speeds, and environmental advantages, since certain chemicals are not needed. In addition to these features, PSPs have a wide dynamic range that provides flexibility for correcting underexposed and overexposed images. When compared to charge-coupled device (CCD) or complementary metal-oxide semiconductor (CMOS) direct digital sensors, PSP is thought to be more acceptable to patients because of its outstanding features such as wireless connectivity, flexibility, and thin design. Despite these advantages, PSP is susceptible to bending and damage during handling, which causes permanent scratching on the receptor. Furthermore, PSP has a lower spatial resolution and a higher image acquisition time; additionally, more steps are needed to visualize the images compared to CCD and CMOS sensors.2
Understanding this technology is very important for resolving image errors and obtaining successful radiographic imaging, as well as for developing innovations in the system. Çalışkan and Sumer3 reported a comprehensive classification of intraoral PSP image errors and artifact types. Chiu et al.4 examined PSP artifacts under the headings of operator errors, scanning machine errors, and sensor defects. In Gulsahi and Secgin's study,5 the effect of visible light on exposed PSPs was studied. In previous studies, the effects of visible light on exposed PSPs and physical damage of the plates were emphasized comprehensively, but scanner and software errors were not mentioned in an all-inclusive manner. In this study, the aim was to determine and classify dental PSP system artifacts in a comprehensive way according to the classifications proposed in previous studies.
Ethical approval for this retrospective study protocol was obtained from the institutional review board (Ondokuz Mayıs University Ethics Committee of the Health Sciences). The radiographic database of Samsun Dental Hospital was used for this study. The digital imaging system in the hospital consists of 4 VistaScan Mini Easy PSP scanners (Dürr Dental, Bietigheim-Bissingen, Germany), 4 VistaScan Mini PSP scanners (Dürr Dental, Bietigheim-Bissingen, Germany), and 2-size and 0-size PSPs (Dürr Dental, Bietigheim-Bissingen, Germany, Apixia Phosphor Plates US).
Anonymized periapical radiographic images in the Digital Imaging and Communications in Medicine (DICOM) format were obtained from the Samsun Dental Hospital PACS system (Ak Dental Ltd., Samsun, Turkey) using the DICOM Query/Retrieve tool. The first 250 images taken every month, between January 2017 and August 2018, for a total of 5000 periapical images, were examined. The images were evaluated on an Eonis 22 monitor (MDRC-2222, Barco, Kortrijk, Belgium) under semi-dark lighting conditions. All the radiographs were evaluated by a single oral radiologist. Image errors and artifacts were classified according to the classifications presented in the studies of Çalışkan and Sumer,3 Chiu et al.,4 Shetty et al.,6 and Langland et al.7 Additionally, especially for scanner artifacts, the user manuals of Digora PSP scanners (Kavo/Soredex, Helsinki, Finland)8 and VistaScan Mini Easy PSP scanners (Dürr Dental, Bietigheim-Bissingen, Germany)9 were consulted, and for software artifacts, the report of the American Association of Physicists in Medicine task group10 and Seeram's study11 were used.
Identified errors and artifacts were classified according to their possible causes. Errors and artifacts that were not observed during this study but were reported in previous studies were also included in the classification. All the radiographs were evaluated under semi-dark lighting conditions. The 500 radiographs that were selected were re-evaluated 2 weeks after the first evaluations under the same conditions to determine intraobserver reliability. Statistical analyses were performed with SPSS version 21 (IBM Corp., Armonk, NY, USA). Intraobserver reliability was analyzed with the kappa statistic, which was interpreted as follows: 0.00–0.10, no agreement; 0.10–0.40, poor agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; and 0.81–1.00, very good agreement. P values <0.05 were considered to indicate statistical significance.
Artifacts and errors were observed in 1,822 periapical radiographic images. The kappa values were found to be between 0.78 and 1.00 for various image artifacts. Based on these values, good or very good agreement was found for intra-observer reliability. After examination of the images, the reasons for the errors and artifacts were divided into 6 categories, which were in turn divided into 45 subheadings. Table 1 shows the frequency of the PSP-specific image artifacts and errors.
In this study, the most common errors were operating errors (34.7%), and the main errors within this group were projection geometry errors (31.9%). The second most common errors were sub-operator errors; this group included artifacts related to the placement of PSPs into the mouth. The most common error in this sub-group was incorrect dot position. Bending the PSP to reduce the patient's discomfort causes a slight line on the bent area, and this also produces distortion and density differences on the bent areas of the images. If the PSP is bent when placed in the mouth, a mirror image occurs. Bent parts and opposite parts have the same radiographic appearance.
In the study, the third most common error involved short scratches (Table 1). These deformations are shown as irregular or straight radiopaque lines anywhere on the radiograph. Using a plate that is not properly matched with the scanner causes the image to elongate longitudinally and produces bright stripes (Table 2, Fig. 2).89
Errors related to the scanner were quite rare; the most common scanner error was horizontal white lines caused by the accumulation of dust and dirt on the narrow window of the scanner (Table 3, Figs. 3, 4, 5, 6). In this study, errors related to the scanner were identified with the help of our technical support team and previous studies.346891011
Incorrect settings of processing menus can result in improper histogram normalization, incorrect dynamic range scaling, and inappropriate output film density.10 In the current study, the actual reasons for incorrect settings could not be determined because this study was conducted retrospectively. Other software artifacts include edge masking defects and bisection of images. Edge masking is designed to improve the quality of clinical images.8911 Defective edge masking causes part of an image to be missing, so that it resembles a cone-cut image or a metal artifact.89 In addition, inadequate edge masking causes image blurring.11 This study found 2 images with the artifact presenting as a blurred image. In this retrospective examination, we could not securely differentiate a defective edge masking artifact from cone-cut images. However, in the clinic, when we encountered this type of edge masking defect, the system gave the edge masking defect error for consecutive images that had a cone-cut appearance in the same region of images (Fig. 7). The solution was to update the software program. However, if the software program cannot be updated, the edge masking tool should be closed. Another software artifact is bisection of images. This error is caused by the image being divided into 2 parts, 1 of which is saved on the screen of the previous patient and the other part saved on the screen of the correct patient (Fig. 8).89 Software artifacts encountered in the clinic that have been reported previously (Table 1).1011
This study found no conveyor belt peeling3 or tongue artifacts,7 excessive cleaning of the plate surface artifacts,89 incorrect settings of processing menus,10communication error artifacts,11 or data cable malfunctions,11 but these artifacts were included in our classification because they had been defined in previous studies and reports.
Very few studies have investigated PSP technology errors and artifacts, and most of the studies that have done so are related to medical radiology.3456 This study aimed to classify the image artifacts of intraoral phosphor plates in an in-depth way and to define the causes of and solutions for errors in this recently developed, popular imaging modality.
This study found that the most common errors were operating errors, with a predominance of projection geometry errors within this group. Several studies and reports have analyzed projection geometry errors.12131415 The projection errors that are generally known are shape distortion errors (foreshortening, elongation, image lengthening, and distortion), horizontal angulation artifacts (overlapping), cone-cutting errors (crown or apices being cut-off), and cone vertical level errors (crowns or apices not showing).
The second most common error was whitening caused by unsuitable ambient light. If the scanning of an exposed PSP is delayed without protection from the ambient light, latent electrons in the image are released spontaneously. These electrons cause noisy and whiter image views. In this study, the artifacts related to ambient light were caused mainly by removal of the plate from its protective cover after exposure to prevent contamination, similar to the findings of Çalışkan and Sümen.3 In addition, Akdeniz et al.16 reported that exposed plates began to release electrons after 10 minutes. Signal loss initially occurs on the periphery of the image because the photons that are exposed on the periphery of the plate have a lower intensity than those that are exposed on the center of the plate.4 Additionally, the highest attenuation value areas, such as fixed prostheses and metallic dental materials, lose photons and have a shiny appearance when exposed to ambient light (Fig. 1B).
Another common error came from short scratches caused by deformations in the plates. Damage to the photo-stimulating luminescence layer and cracking in the supporting polyester layer can occur for a variety of reasons, including careless manipulation when positioning the PSP in the mouth, excessive bending, unintentional biting by the patient, using force when placing the film into the scanner, and mechanical stresses of the rollers and holders during the scanning process. Manufacturers recommend using protective covers to minimize mechanical damage to the plates.89 Previous studies have suggested that plastic barrier envelopes were not able to prevent bite marks.4 PSP damage can be handled using Roberts and Mol's method,17 which involves placing double-sided pieces of tape around the sensor plate cover. It has also been reported that the use of both cardboard sheaths and disposable plastic envelopes prevents PSP damage; however, this also causes movement of the phosphor plates in the disposable packets.13 PSPs should be checked every day for scratches. If scratches are found on the surface, a test image should be taken and, if necessary, the PSP should be replaced. It was observed that the rate of physical damage to the PSPs was much higher than reported by Chiu et al.4 and Gülsahi et al.,5 but similar to that reported by Çalışkan and Sümer.3 In this study, the high rate of the PSP damages was due to the fact that new PSPs could not be purchased when needed because of the hospital's financial situation and the high costs of the PSPs.
Manufacturers recommend opening the adhesive side of the protective cover and placing the PSP onto the scanner input unit with the light protection cover.9 The image plate should then be slid out of its protective cover downwards into the unit until the image plate is automatically drawn in. The aim of this process is to prevent handling and ambient light-induced errors and artifacts.
Dust particles, glove powder, body oil, saliva, adhesive material for the protective covers, and dental adhesive material are agents that have been reported as being responsible for dirt on the plate.35 Dirt on the active side of the plate blocks the laser light and causes radiopaque artifacts.35
Wiping the plates may also have a negative effect on plate quality. For this reason, Kalathingal et al.18 advised that plates should be given a light wipe only when needed and should be cleaned with 95% alcohol and a soft cloth to remove any surface dust particles, body oil contamination, and smudges. The current study found no wiping artifacts, because the plates were cleaned with cleaning pads only when the PSP surface was contaminated.
Errors related to the scanner in the current study were identified with the help of technical support staff, but these errors were, in fact, rarely observed. The direction of the laser beams, which is guided by the mirrors, is referred to as the “fast scan direction.” The transport mechanism guides the plate through the unit, and this movement direction is called “slow scan direction.” It was reported that white lines extending in the fast scan direction are caused by dirt on the transport mechanism, and that white lines extending in the slow scan direction are caused by dirt on the light guide.4 Dirt on the narrow scanning window may block the stimulating laser light at the same place on every fast scan cycle. Dirt on the parabolic mirrors or light collector may block the signal from reaching the photomultiplier tube and cause a focal no-signal area. If the blocking agent remains present throughout the entire scanning procedure of the plate, it may generate a radiopaque straight line on the radiographic image. Çalışkan and Sümer3 reported that zigzag lines are probably related to minimal movement of the dirt agent because of scanner vibration during the scanning process. Manufacturers recommend that the scanner transport mechanism and laser slit should be cleaned if these elements are contaminated. Spray cleaning agents should not be used to clean the unit because liquid may penetrate into the unit.9 In addition, an air spray may push dirt deeper into the device on the narrow scanning window.
An inadequate erasing process causes a ghost image of the previous exposure to appear on the image. The solution is to check the setting. The eraser setting should be at the highest erasing power, while the scanning speed should be at the slowest setting.89
Failures of laser units on intraoral imaging systems have not been comprehensively reported in previous studies. The laser unit can contribute to a wide variety of errors, of which separation of images into 2 parts and image fragmentation occurred in this study. A sandy view and a gearlike image are shown in the user guide, but they were not observed in this study. The manufacturers recommend changing the laser unit to solve this problem.9
In this study, 2 images with radiolucent bands were observed and these artifacts appeared as 4 straight lines in the same image, equidistant from each other. It was reported that such scan lines were caused by dust/dirt particles on the pickup light guide.10 Shetty et al.6 reported that non-visualized areas and missing lines or pixels may be caused by sudden power failures. In addition to that, before this study was performed, radiolucent bands with different characteristics were observed in 4 consecutive images taken from a phantom jaw. These radiolucent bands in phantom images were seem as multiple radiolucent lines parallel to the fast scan direction (Fig. 6). After the device connections had been repeatedly put in place, the error was diminished. The manufacturers report that electromagnetic interference artifacts are caused by the existence of power lines in the immediate vicinity, which is a physical phenomenon that can affect electronic equipment in general.9 Manufacturers suggest adding appropriate electromagnetic shielding, and that the quality of the supply voltage should corresponded to a typical commercial or hospital environment. The device should also be powered from an uninterruptible power supply or from a battery.9 Çalışkan and Sumer3 referred to this as the ridging artifact, and suggested that these multiple radiolucent lines parallel to the fast scan direction are caused by momentary changes in the light intensity of the stimulating lasers and loss of synchronization between fast scan cycles and image plate transitions. A full consensus about radiolucent artifacts has not been achieved; further research is needed on this type of artifacts.
Plate size determination error most likely occurs when the scanner detects a different size from that of the scanned plate. The current study observed this artifact when the number 2 plate was detected as being the number 0 plate, causing half of the image to be missing. Çalışkan and Sümer3 reported that this error occurs when multiple intraoral-sized plates are scanned and the scanner mistakenly detects the size as panoramic or cephalometric.
In the current study, software artifacts, except the edge masking defect and the bisection artifact, could not be identified because this study was conducted retrospectively. However, in the clinic, when there was a disturbance in connectivity, the exposed and then scanned plate represented the image as an image of the unexposed plate on the screen and the system gave a connection error. However, it has been reported that communication errors result from power failure during image transmission, causing missing lines or pixels in the resulting image.11
In conclusion, PSP systems have characteristic artifact properties. Some of these artifacts can be solved by making corrective interventions such as updating software or replacing damaged scanner parts. In addition, checking the plates regularly and working with appropriate procedures may prevent the physical deformation of the plates and contribute to the reduction of some artifacts. Knowledge of basic physics and the technology of the PSP system may result in more successful radiographic imaging. However, there is a need to conduct further research into PSP artifacts and errors to help make radiographic imaging more useful.
Figures and Tables
 | Fig. 1A. Phalangioma (arrow). B. The dental fillings (highest attenuation value areas) lost photons and had a shiny appearance when exposed to ambient light. C. A text pattern caused by exposure to visible light. |
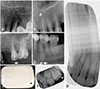 | Fig. 2Phosphor storage plate (PSP) damage. A. Stretches. B. Crescent-shaped bending (arrow). C. Bite marks (arrow). D. Partial stripping (arrow). E. Peeled plate surface. F. Reticulation caused by a peeled PSP surface. G. Elongation of the image resulting from use of a mismatched plate. |
 | Fig. 3Scanner artifacts. A. The gray lines extend in the fast scan direction (thick arrow) (caused by dust on the light guide) and dust particles (thin arrow). B. The gray line extends in the fast scan direction (arrow). C. Transport belt artifact (caused by the belt motor not moving at the correct speed, resulting in an abnormal elongation of the image). |
 | Fig. 6Scanner artifacts. A. Straight radiolucent lines (with the likely cause being dust/dirt particles on the pickup light guide). B and C. Parallel multiple radiolucent lines images obtained from a phantom head. The likely cause was electromagnetic interference. |
 | Fig. 7Software artifacts. A. An edge masking defect causing a noisy view. B. An edge masking defect simulating a cone-cut image. |
References
1. Wakoh M, Kuroyanagi K. Digital imaging modalities for dental practice. Bull Tokyo Dent Coll. 2001; 42:1–14.

2. Mol A. Digital Imaging. In : Mallya SM, Lam EW, editors. White and Pharoah's oral radiology: principles and interpretation. 8rd ed. St. Louis: Elsevier;2019. p. 40–60.
3. Çalışkan A, Sumer AP. Definition, classification and retrospective analysis of photostimulable phosphor image artefacts and errors in intraoral dental radiography. Dentomaxillofac Radiol. 2017; 46:20160188.

4. Chiu HL, Lin SH, Chen CH, Wang WC, Chen JY, Chen YK, et al. Analysis of photostimulable phosphor plate image artifacts in an oral and maxillofacial radiology department. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:749–756.

5. Gulsahi A, Secgin CK. Assessment of intraoral image artifacts related to photostimulable phosphor plates in a dentomaxillofacial radiology department. Niger J Clin Pract. 2016; 19:248–253.

6. Shetty CM, Barthur A, Kambadakone A, Narayanan N, Kv R. Computed radiography image artifacts revisited. AJR Am J Roentgenol. 2011; 196:W37–W47.

7. Langland OE, Langlais RP, Preece JW. Analysis of errors and artifacts. Principles of dental imaging. Baltimore: Williams & Wilkins;2002. p. 160.

8. Kavo.com [Internet]. Biberach: SOREDEX™ DIGORA™ Optime;c2019. cited 2019 Jan 7. Available from: https://www.kavo.com/dental-x-ray-machines-and-diagnostics/scan-exam-intraoral#docs.
9. Duerrdental.com [Internet]. Bietigheim-Bissingen: VistaScan Mini Easy;Available from: https://www.duerrdental.com/en/products/imaging/vistascan-image-plate-scanner/vistascan-mini-easy/.
10. Seibert JA, Bogucki TM, Ciona T, Huda W, Karellas A, Mercier JR, et al. Report No. 093 - Acceptance testing and quality control of photostimulable storage phosphor imaging systems. Alexandria: American Association of Physicists in Medicine;2006.
11. Seeram E. Computed radiography: physics and technology. Digital radiography. Singapore: Springer;2019. p. 41–63.
12. Duckworth JE, Judy PF, Goodson JM, Socransky SS. A method for the geometric and densitometric standardization of intraoral radiographs. J Periodontol. 1983; 54:435–440.

13. Webber RL, Ruttimann UE, Groenhuis RA. Computer correction of projective distortions in dental radiographs. J Dent Res. 1984; 63:1032–1036.

14. Menchini-Fabris GB, Covani U, Toti P, Marconcini S, Barone A, Martuscelli R. A methodological approach to standardize and control the quality of the position and alignment of lamina implants on two-dimensional radiographs. Oral Radiol. (in press).

15. Sanghvi S, Rao A, Karuna YM, Shetty K, Nayak A. Image distortion of the roots of maxillary deciduous molars on Iopa's recorded with bisecting angle or a modified paralleling technique. Biomed Pharmacol J. 2018; 11:1039–1042.

16. Akdeniz BG, Gröndahl HG, Kose T. Effect of delayed scanning of storage phosphor plates. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 99:603–607.

17. Roberts MW, Mol A. Clinical techniques to reduce sensor plate damage in PSP digital radiography. J Dent Child (Chic). 2004; 71:169–170.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download