1. Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, Kim S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J. 2015; 45:1479–1481.

2. Iyer VN, Lim KG. Chronic cough: an update. Mayo Clin Proc. 2013; 88:1115–1126.

3. Irwin RS, French CL, Chang AB, Altman KW. CHEST Expert Cough Panel*. Classification of cough as a symptom in adults and management algorithms: CHEST guideline and expert panel report. Chest. 2018; 153:196–209.
4. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008; 63:Suppl 86. 8–160.
5. Katelaris CH, Lee BW, Potter PC, Maspero JF, Cingi C, Lopatin A, et al. Prevalence and diversity of allergic rhinitis in regions of the world beyond Europe and North America. Clin Exp Allergy. 2012; 42:186–207.

6. Meltzer EO. Allergic rhinitis: burden of illness, quality of life, comorbidities, and control. Immunol Allergy Clin North Am. 2016; 36:235–248.
7. Hong Q, Bai C, Wang X. Characteristics of Chinese patients with cough in primary care centre. J Transl Med. 2011; 9:149.

8. Cho SH, Lin HC, Ghoshal AG, Bin Abdul Muttalif AR, Thanaviratananich S, Bagga S, et al. Respiratory disease in the Asia-Pacific region: cough as a key symptom. Allergy Asthma Proc. 2016; 37:131–140.

9. Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:63S–71S.
10. Tajiri T, Niimi A, Matsumoto H, Ito I, Oguma T, Otsuka K, et al. Prevalence and clinical relevance of allergic rhinitis in patients with classic asthma and cough variant asthma. Respiration. 2014; 87:211–218.

11. Lai K, Liu B, Xu D, Han L, Lin L, Xi Y, et al. Will nonasthmatic eosinophilic bronchitis develop into chronic airway obstruction?: a prospective, observational study. Chest. 2015; 148:887–894.
12. Wang Z, Pianosi P, Keogh K, Zaiem F, Alsawas M, Alahdab F, et al. The clinical utility of fractional exhaled nitric oxide (FeNO) in asthma management. Rockville (MD): Agency for Healthcare Research and Quality;2017.
13. Ciprandi G, Gallo F, Ricciardolo FL, Cirillo I. Fractional exhaled nitric oxide: a potential biomarker in allergic rhinitis? Int Arch Allergy Immunol. 2017; 172:99–105.

14. Krantz C, Janson C, Borres MP, Nordvall L, Alving K, Malinovschi A. Nasal nitric oxide is associated with exhaled NO, bronchial responsiveness and poor asthma control. J Breath Res. 2014; 8:026002.

15. Sato S, Saito J, Sato Y, Ishii T, Xintao W, Tanino Y, et al. Clinical usefulness of fractional exhaled nitric oxide for diagnosing prolonged cough. Respir Med. 2008; 102:1452–1459.

16. Maniscalco M, Faraone S, Sofia M, Molino A, Vatrella A, Zedda A. Extended analysis of exhaled and nasal nitric oxide for the evaluation of chronic cough. Respir Med. 2015; 109:970–974.

17. Bommarito L, Migliore E, Bugiani M, Heffler E, Guida G, Bucca C, et al. Exhaled nitric oxide in a population sample of adults. Respiration. 2008; 75:386–392.

18. Linhares D, Jacinto T, Pereira AM, Fonseca JA. Effects of atopy and rhinitis on exhaled nitric oxide values - a systematic review. Clin Transl Allergy. 2011; 1:8.

19. Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:75S–79S.
20. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of lung function testing: the authors' replies to readers' comments. Eur Respir J. 2010; 36:1496–1498.

21. Burgel PR. The role of small airways in obstructive airway diseases. Eur Respir Rev. 2011; 20:23–33.

22. Ciprandi G, Tosca MA, Signori A, Cirillo I. Bronchial hyperreactivity in patients with allergic rhinitis: forced expiratory flow between 25 and 75% of vital capacity might be a predictive factor. Allergy Asthma Proc. 2011; 32:4–8.

23. Ciprandi G, Tosca MA, Castellazzi AM, Cairello F, Salpietro C, Arrigo T, et al. FEF(25–75) might be a predictive factor for bronchial inflammation and bronchial hyperreactivity in adolescents with allergic rhinitis. Int J Immunopathol Pharmacol. 2011; 24:17–20.

24. Sposato B, Scalese M, Migliorini MG, Di Tomassi M, Scala R. Small airway impairment and bronchial hyperresponsiveness in asthma onset. Allergy Asthma Immunol Res. 2014; 6:242–251.

25. Morice AH, Fontana GA, Belvisi MG, Birring SS, Chung KF, Dicpinigaitis PV, et al. ERS guidelines on the assessment of cough. Eur Respir J. 2007; 29:1256–1276.

26. Kanemitsu Y, Matsumoto H, Oguma T, Nagasaki T, Ito I, Izuhara Y, et al. Independent factors contributing to daytime and nighttime asthmatic cough refractory to inhaled corticosteroids. J Investig Allergol Clin Immunol. 2019; 29:30–39.

27. Good JT Jr, Rollins DR, Kolakowski CA, Stevens AD, Denson JL, Martin RJ. New insights in the diagnosis of chronic refractory cough. Respir Med. 2018; 141:103–110.

28. Dreborg S. Skin testing. The safety of skin tests and the information obtained from using different methods and concentrations of allergen. Allergy. 1993; 48:473–475.
29. American Thoracic Society. European Respiratory Society. ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med. 2005; 171:912–930.
30. Sohn SW, Lee HS, Park HW, Chang YS, Kim YK, Cho SH, et al. Evaluation of cytokine mRNA in induced sputum from patients with allergic rhinitis: relationship to airway hyperresponsiveness. Allergy. 2008; 63:268–273.
31. Birnbaum S, Barreiro TJ. Methacholine challenge testing: identifying its diagnostic role, testing, coding, and reimbursement. Chest. 2007; 131:1932–1935.
32. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983; 148:839–843.

33. Lai K, Chen R, Lin J, Huang K, Shen H, Kong L, et al. A prospective, multicenter survey on causes of chronic cough in China. Chest. 2013; 143:613–620.

34. Mims JW. Asthma: definitions and pathophysiology. Int Forum Allergy Rhinol. 2015; 5:Suppl 1. S2–S6.

35. Yi F, Chen R, Luo W, Xu D, Han L, Liu B, et al. Validity of fractional exhaled nitric oxide in diagnosis of corticosteroid-responsive cough. Chest. 2016; 149:1042–1051.

36. Westerhof GA, Korevaar DA, Amelink M, de Nijs SB, de Groot JC, Wang J, et al. Biomarkers to identify sputum eosinophilia in different adult asthma phenotypes. Eur Respir J. 2015; 46:688–696.

37. Tang W, Zhou J, Miao L, Shi G. Clinical features in patients of cough variant asthma with normal and high level of exhaled fractional nitric oxide. Clin Respir J. 2018; 12:595–600.

38. Oh MJ, Lee JY, Lee BJ, Choi DC. Exhaled nitric oxide measurement is useful for the exclusion of nonasthmatic eosinophilic bronchitis in patients with chronic cough. Chest. 2008; 134:990–995.

39. Song WJ, Kim HJ, Shim JS, Won HK, Kang SY, Sohn KH, et al. Diagnostic accuracy of fractional exhaled nitric oxide measurement in predicting cough-variant asthma and eosinophilic bronchitis in adults with chronic cough: a systematic review and meta-analysis. J Allergy Clin Immunol. 2017; 140:701–709.
40. Song DJ, Song WJ, Kwon JW, Kim GW, Kim MA, Kim MY, et al. KAAACI evidence-based clinical practice guidelines for chronic cough in adults and children in Korea. Allergy Asthma Immunol Res. 2018; 10:591–613.

41. Hsu JY, Wang CY, Cheng YW, Chou MC. Optimal value of fractional exhaled nitric oxide in inhaled corticosteroid treatment for patients with chronic cough of unknown cause. J Chin Med Assoc. 2013; 76:15–19.

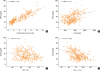
42. Bao W, Zhang X, Lv C, Bao L, Yin J, Huang Z, et al. The value of fractional exhaled nitric oxide and forced mid-expiratory flow as predictive markers of bronchial hyperresponsiveness in adults with chronic cough. J Allergy Clin Immunol Pract. 2018; 6:1313–1320.

43. Muñoz-López F, Ríos-Alcolea M. The interest of FEF(25–75) in evaluating bronchial hyperresponsiveness with the methacholine test. Allergol Immunopathol (Madr). 2012; 40:352–356.

44. Niimi A. Cough associated with gastro-oesophageal reflux disease (GORD): Japanese experience. Pulm Pharmacol Ther. 2017; 47:59–65.

45. Kahrilas PJ, Altman KW, Chang AB, Field SK, Harding SM, Lane AP, et al. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest. 2016; 150:1341–1360.
46. Hulme K, Deary V, Dogan S, Parker SM. Psychological profile of individuals presenting with chronic cough. ERJ Open Res. 2017; 3:00099-2016.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download