INTRODUCTION
Table 1
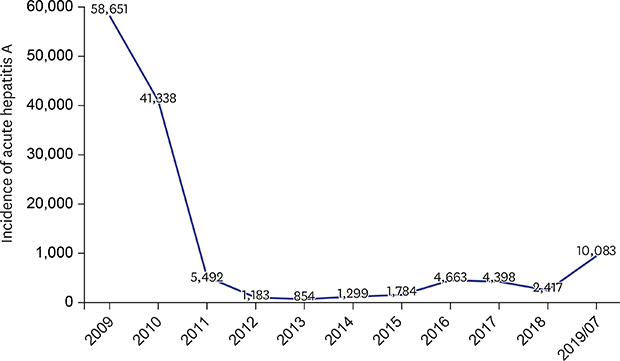
Age-related incidence of acute hepatitis A according to KCDC
Journal List > J Korean Med Sci > v.34(Suppl 1) > 1133388
Funding This work was supported by National Research Foundation of Korea grants funded by the Korean government (2017R1A2B4009199, 2017R1A5A2015369 and 2018R1C1B5044890) and the Yonsei University Wonju Campus Future-Leading Research Initiative of 2018 (2018-62-0041). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Seong Hee Kang 
https://orcid.org/0000-0002-0783-509X
Moon Young Kim 
https://orcid.org/0000-0002-2501-2206
Soon Koo Baik 
https://orcid.org/0000-0001-6245-2537