INTRODUCTION
Lung transplant (LTx) has been accepted as a standard treatment for patients with end-stage lung disease.
1 The first LTx in Korea was performed in July 1996.
2 Since the outbreak of lung injuries caused by humidifier disinfectants in 2010,
3 the number of LTx has been rapidly increasing in Korea, from 18 cases in 2010 to 93 cases in 2017. However, the number of patients on the waitlist for LTx has also been increasing, from 39 patients in 2010 to 168 patients in 2017.
4 Due to organ donor shortages and increasing number of transplant candidates, some candidates may inevitably die while on the waitlist, without getting a chance to receive LTx. For this reason, efficient allocation systems for donor lungs are of great importance in Korea.
Each country has its own allocation system. The lung allocation score (LAS) system is the most widely used allocation system in the world. It is based on the statistical model developed by analyzing the national transplant database of the United States,
56 which takes into account both the urgency and the benefits of the transplant. In Korea, allocation system for donor lungs is based only on urgency of transplant. It divides patients into four groups according to urgency criteria, which are determined empirically. Status 0 is the most urgent status and designates hospitalized patients requiring a ventilator and/or extracorporeal life support. The Korean allocation system has rarely been evaluated and validated by large data. Previously, a single center retrospective study was conducted to evaluate the Korean allocation system by simulating LAS system. This study found that most LTx were performed in Status 0 or Status 1 patients. Status 0 patients had significantly higher LASs and poorer post-transplant survival rates than Status 1 patients.
7
The Korean Organ Transplant Registry (KOTRY) was established in 2014 as a service of the Korean Centers for Disease Control (KCDC), and it began to resister LTx cases in 2015.
8 It is the first nationwide multi-center registry for LTx in Korea. This study aimed to investigate the characteristics of donor lung allocation using this urgency-based lung allocation system, and to evaluate the outcomes of LTx according to the Korean urgency status using KOTRY database.
Go to :

MATERIALS AND METHODS
Korean allocation system of donor lungs
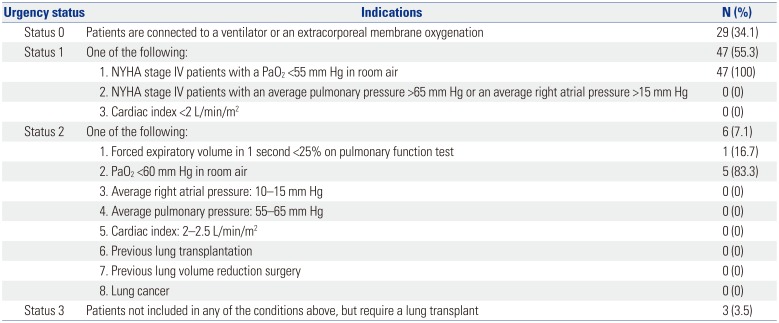
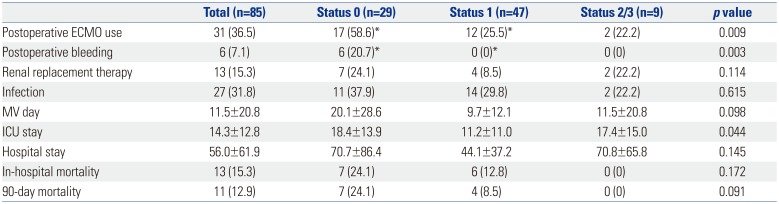
The definition of urgency status is described in
Table 1.
79 Donor lungs are allocated to the most urgent patients based on urgency status. When the urgency status of a transplant candidate changes, the institution of the candidate must inform the Korean Network for Organ Sharing (KONOS). Then, KONOS uses the urgency status to determine the allocation of donor lungs. Among patients with the same urgency status, candidates are selected using a scoring system that takes into account waiting time, blood type, presence of infectious disease, distance between the donor and recipient hospitals, age, primary lung diagnosis, and difference in the donor's and recipient's estimated lung volumes.
Table 1
Indication and Distributions of Urgency Status of Lung Transplantation Recipients
|
Urgency status |
Indications |
N (%) |
|
Status 0 |
Patients are connected to a ventilator or an extracorporeal membrane oxygenation |
29 (34.1) |
|
Status 1 |
One of the following: |
47 (55.3) |
|
1. NYHA stage IV patients with a PaO2 <55 mm Hg in room air |
47 (100) |
|
2. NYHA stage IV patients with an average pulmonary pressure >65 mm Hg or an average right atrial pressure >15 mm Hg |
0 (0) |
|
3. Cardiac index <2 L/min/m2
|
0 (0) |
|
Status 2 |
One of the following: |
6 (7.1) |
|
1. Forced expiratory volume in 1 second <25% on pulmonary function test |
1 (16.7) |
|
2. PaO2 <60 mm Hg in room air |
5 (83.3) |
|
3. Average right atrial pressure: 10–15 mm Hg |
0 (0) |
|
4. Average pulmonary pressure: 55–65 mm Hg |
0 (0) |
|
5. Cardiac index: 2–2.5 L/min/m2
|
0 (0) |
|
6. Previous lung transplantation |
0 (0) |
|
7. Previous lung volume reduction surgery |
0 (0) |
|
8. Lung cancer |
0 (0) |
|
Status 3 |
Patients not included in any of the conditions above, but require a lung transplant |
3 (3.5) |

Data source and variables
This study was approved by Institutional Review Board (IRB) at Severance Hospital, Yonsei University College of Medicine (IRB number 4-2017-0815). Patients in this study were selected from the LTx cohort of KOTRY. Patients who received heart-lung transplantation were excluded. LTx cohort of KOTRY began in 2015, and five institutions have contributed to LTx registry. Written informed consent was obtained from all participants prior to LTx at relevant institutions; therefore, the need for patient consent was waived for this study. Patients who received LTx from the beginning of the cohort to June 2017 were enrolled in this study. Follow-up was completed in December 2017.
According to the urgency status of recipient at the time of LTx, we compared recipient and donor characteristics, operative characteristics, and postoperative outcomes. Recipient characteristics included age, sex, primary pulmonary diagnosis, intensive care unit (ICU) care, mechanical ventilation, extracorporeal membrane oxygenator (ECMO) support at the time of LTx, and wait time. Wait time was measured from the date of enrollment for LTx to the date of transplant. Donor characteristics included age, sex, smoking, and partial pressure of oxygen (PaO2) in the arterial blood/fraction of inspired oxygen ratio (P/F ratio). Operative characteristics included unilateral or bilateral LTx, intraoperative extracorporeal life support (ECLS), operative time, and intraoperative transfusion. Postoperative outcomes included measured major postoperative complications (postoperative ECMO use, bleeding, need for renal replacement therapy, infection), length of mechanical ventilation, length of ICU stay, and survival.
Statistical analysis
Statistical analysis was performed using SPSS version 23.0 (IBM Corp, Armonk, NY, USA) and R version 3.4.4 (R Foundation for Statistical Computing, Vienna, Austria). Clinical variables were described as mean±standard deviation or median (range) for continuous variables, and as frequency (percentage) for categorical variables. Continuous variables were compared using one-way analysis of variance. Categorical variables were compared using chi-squared test or Fisher's exact test. Bonferroni correction was used in multiple comparisons with continuous and categorical variables. Survival analysis was performed using Kaplan-Meier method, and comparisons were made using log-rank test. p values less than 0.05 were considered statistically significant.
Go to :

RESULTS
During the study period, a total of 86 patients were enrolled in KOTRY. After excluding one patient who received heart-lung transplant, 85 patients were included in this study. Twenty-nine Status 0 patients (34.1%) received LTx. There were 47 Status 1 patients and six Status 2 patients who received LTx. All Status 1 patients and 83.3% of Status 2 patients were classified based on the criteria of PaO
2 in arterial blood gas analysis and functional status (
Table 1).
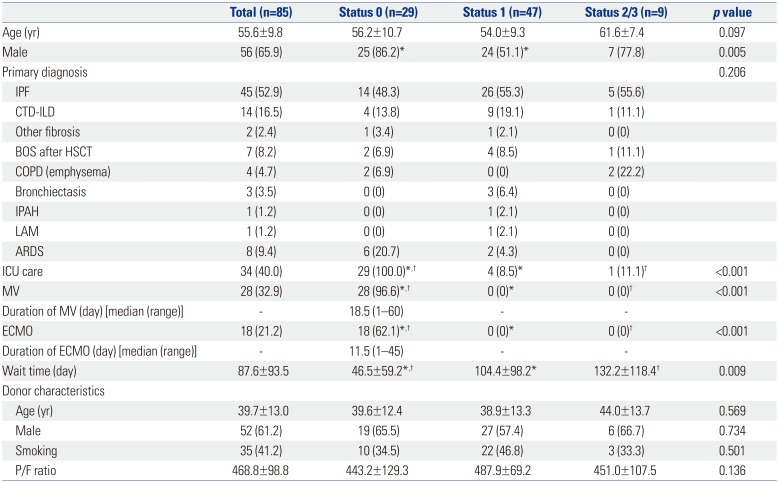
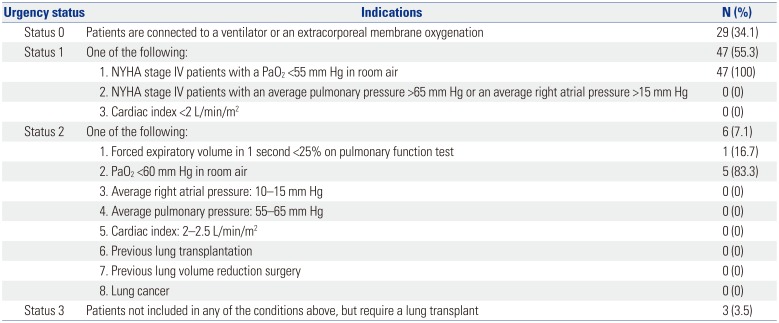
Patient and donor characteristics are summarized in
Table 2. The mean age of all patients was 55.6±9.8, and 65.9% of patients were men. There were more male patients with Status 0 than with Status 1 (
p=0.012). Idiopathic pulmonary fibrosis (IPF) was the most frequent indication for LTx in all urgency status groups. All Status 0 patients were under care in ICU at the time of transplant. Among Status 0 patients, 28 (96.6%) and 18 (62.1%) were supported by mechanical ventilation and ECMO, respectively. The mean wait time was 87.6±93.5 days, and Status 0 patients had significantly shorter wait times than Status 1 patients (
p=0.022) or Status 2/3 patients (
p=0.042). There was no significant difference in donor characteristics based on urgency status.
Table 2
Baseline Characteristics of Patients
|
Total (n=85) |
Status 0 (n=29) |
Status 1 (n=47) |
Status 2/3 (n=9) |
p value |
|
Age (yr) |
55.6±9.8 |
56.2±10.7 |
54.0±9.3 |
61.6±7.4 |
0.097 |
|
Male |
56 (65.9) |
25 (86.2)*
|
24 (51.1)*
|
7 (77.8) |
0.005 |
|
Primary diagnosis |
|
|
|
|
0.206 |
|
IPF |
45 (52.9) |
14 (48.3) |
26 (55.3) |
5 (55.6) |
|
|
CTD-ILD |
14 (16.5) |
4 (13.8) |
9 (19.1) |
1 (11.1) |
|
|
Other fibrosis |
2 (2.4) |
1 (3.4) |
1 (2.1) |
0 (0) |
|
|
BOS after HSCT |
7 (8.2) |
2 (6.9) |
4 (8.5) |
1 (11.1) |
|
|
COPD (emphysema) |
4 (4.7) |
2 (6.9) |
0 (0) |
2 (22.2) |
|
|
Bronchiectasis |
3 (3.5) |
0 (0) |
3 (6.4) |
0 (0) |
|
|
IPAH |
1 (1.2) |
0 (0) |
1 (2.1) |
0 (0) |
|
|
LAM |
1 (1.2) |
0 (0) |
1 (2.1) |
0 (0) |
|
|
ARDS |
8 (9.4) |
6 (20.7) |
2 (4.3) |
0 (0) |
|
|
ICU care |
34 (40.0) |
29 (100.0)*,†
|
4 (8.5)*
|
1 (11.1)†
|
<0.001 |
|
MV |
28 (32.9) |
28 (96.6)*,†
|
0 (0)*
|
0 (0)†
|
<0.001 |
|
Duration of MV (day) [median (range)] |
- |
18.5 (1–60) |
- |
- |
|
|
ECMO |
18 (21.2) |
18 (62.1)*,†
|
0 (0)*
|
0 (0)†
|
<0.001 |
|
Duration of ECMO (day) [median (range)] |
- |
11.5 (1–45) |
- |
- |
|
|
Wait time (day) |
87.6±93.5 |
46.5±59.2*,†
|
104.4±98.2*
|
132.2±118.4†
|
0.009 |
|
Donor characteristics |
|
|
|
|
|
|
Age (yr) |
39.7±13.0 |
39.6±12.4 |
38.9±13.3 |
44.0±13.7 |
0.569 |
|
Male |
52 (61.2) |
19 (65.5) |
27 (57.4) |
6 (66.7) |
0.734 |
|
Smoking |
35 (41.2) |
10 (34.5) |
22 (46.8) |
3 (33.3) |
0.501 |
|
P/F ratio |
468.8±98.8 |
443.2±129.3 |
487.9±69.2 |
451.0±107.5 |
0.136 |

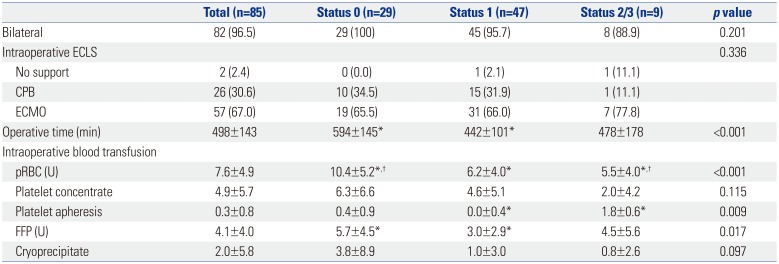
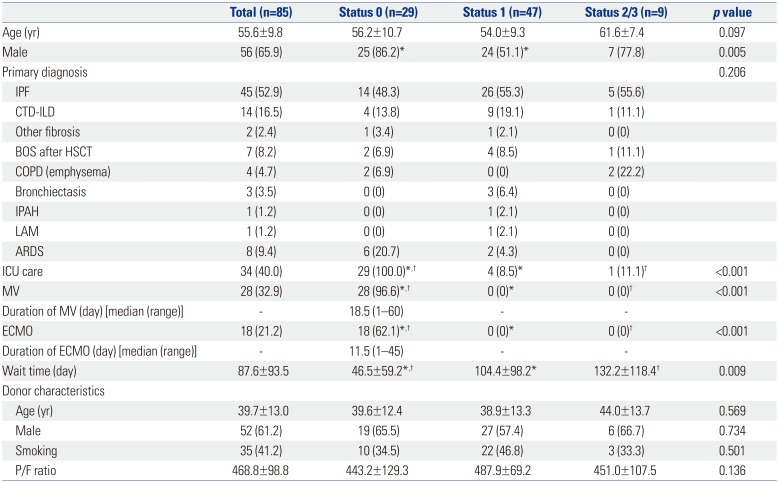
Most patients received bilateral LTx. There was no difference in intraoperative ECLS based on urgency status. Operation times were significantly longer (
p<0.001), and red blood cells and fresh frozen plasma were more frequently transfused intraoperatively in Status 0 patients than in Status 1 patients (
p<0.001 and
p=0.014, respectively) (
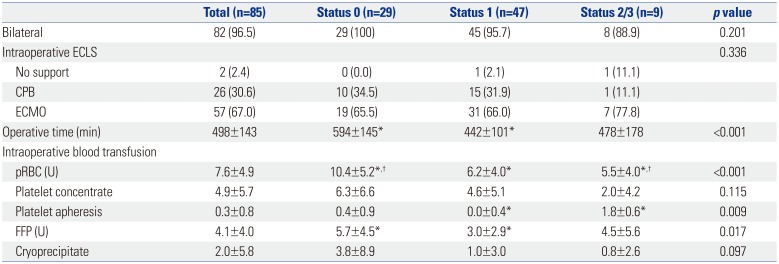
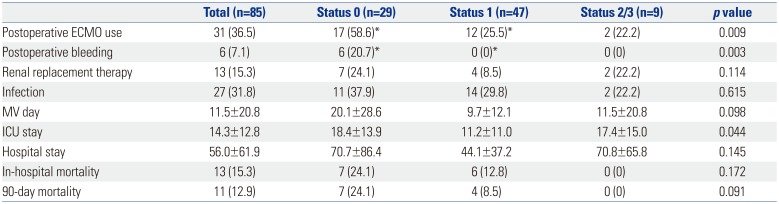
Table 3). Seventeen (58.6%) Status 0 patients required postoperative ECMO, which was significantly higher than the number of Status 1 patients requiring ECMO (
p=0.020). Six status 0 (20.7%) patients suffered from postoperative bleeding, and there was no postoperative bleeding among other urgency statuses. Although there was no statistical significance, Status 0 patients seemed to have longer periods of mechanical support, longer ICU and hospital stay, and poorer short-term survival (
Table 4,
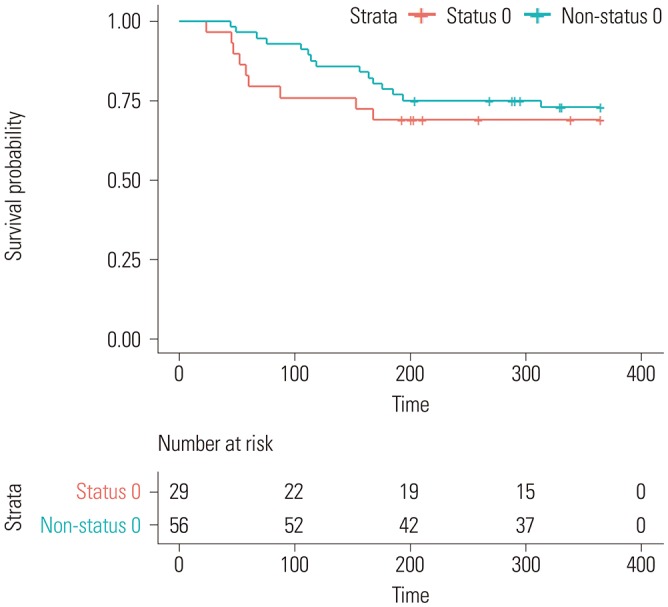
Fig. 1) compared to patients in other urgency statuses.
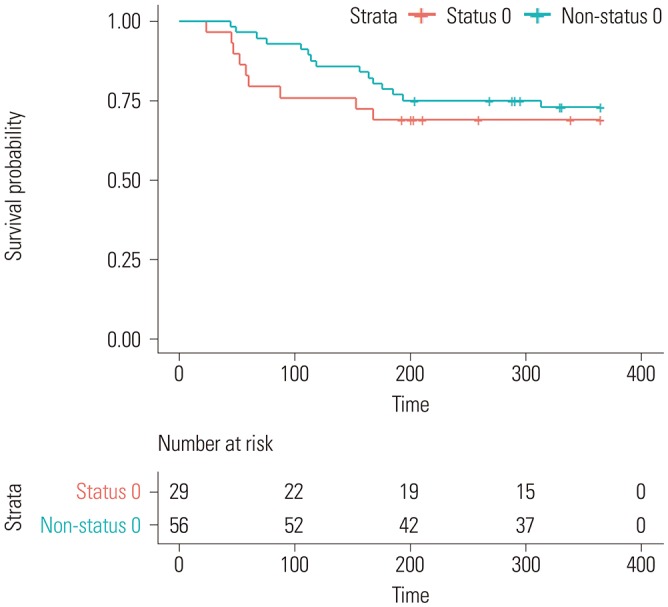 | Fig. 1Survival curves of Status 0 and non-Status 0 patients.
|
Table 3
Operative Characteristics
|
Total (n=85) |
Status 0 (n=29) |
Status 1 (n=47) |
Status 2/3 (n=9) |
p value |
|
Bilateral |
82 (96.5) |
29 (100) |
45 (95.7) |
8 (88.9) |
0.201 |
|
Intraoperative ECLS |
|
|
|
|
0.336 |
|
No support |
2 (2.4) |
0 (0.0) |
1 (2.1) |
1 (11.1) |
|
|
CPB |
26 (30.6) |
10 (34.5) |
15 (31.9) |
1 (11.1) |
|
|
ECMO |
57 (67.0) |
19 (65.5) |
31 (66.0) |
7 (77.8) |
|
|
Operative time (min) |
498±143 |
594±145*
|
442±101*
|
478±178 |
<0.001 |
|
Intraoperative blood transfusion |
|
|
|
|
|
|
pRBC (U) |
7.6±4.9 |
10.4±5.2*,†
|
6.2±4.0*
|
5.5±4.0*,†
|
<0.001 |
|
Platelet concentrate |
4.9±5.7 |
6.3±6.6 |
4.6±5.1 |
2.0±4.2 |
0.115 |
|
Platelet apheresis |
0.3±0.8 |
0.4±0.9 |
0.0±0.4*
|
1.8±0.6*
|
0.009 |
|
FFP (U) |
4.1±4.0 |
5.7±4.5*
|
3.0±2.9*
|
4.5±5.6 |
0.017 |
|
Cryoprecipitate |
2.0±5.8 |
3.8±8.9 |
1.0±3.0 |
0.8±2.6 |
0.097 |

Table 4
Post-Operative Outcomes
|
Total (n=85) |
Status 0 (n=29) |
Status 1 (n=47) |
Status 2/3 (n=9) |
p value |
|
Postoperative ECMO use |
31 (36.5) |
17 (58.6)*
|
12 (25.5)*
|
2 (22.2) |
0.009 |
|
Postoperative bleeding |
6 (7.1) |
6 (20.7)*
|
0 (0)*
|
0 (0) |
0.003 |
|
Renal replacement therapy |
13 (15.3) |
7 (24.1) |
4 (8.5) |
2 (22.2) |
0.114 |
|
Infection |
27 (31.8) |
11 (37.9) |
14 (29.8) |
2 (22.2) |
0.615 |
|
MV day |
11.5±20.8 |
20.1±28.6 |
9.7±12.1 |
11.5±20.8 |
0.098 |
|
ICU stay |
14.3±12.8 |
18.4±13.9 |
11.2±11.0 |
17.4±15.0 |
0.044 |
|
Hospital stay |
56.0±61.9 |
70.7±86.4 |
44.1±37.2 |
70.8±65.8 |
0.145 |
|
In-hospital mortality |
13 (15.3) |
7 (24.1) |
6 (12.8) |
0 (0) |
0.172 |
|
90-day mortality |
11 (12.9) |
7 (24.1) |
4 (8.5) |
0 (0) |
0.091 |

Go to :

DISCUSSION
In this study, we found that the urgency status for LTx in Korea is defined in practice by limited clinical parameters, such as mechanical ventilation and/or ECMO use, functional status, and PaO2. Additionally, most of the candidates who received LTx were either Status 0 or Status 1 patients. Status 0 was associated with longer operative times, higher intraoperative blood transfusion volumes, higher postoperative ECMO use, postoperative bleeding, and longer postoperative ICU stay. Status 0 patients seemed to have poorer postoperative survival.
Allocation systems differ between countries. They are based on the urgency, waiting time, benefits, or a combination of these criteria in most countries.
67 If waiting time is used, there must be no disagreement. However, it is difficult to decide which patient is more urgent or who will benefit more from lung transplantation. The Korean allocation system was designed to allocate donor lungs based on urgency. The urgency criteria were created empirically by experts. The criteria were not based on data, and the data have not been validated. Notably, there was a lack of data to determine whether the urgency status in Korea reflects the true urgency or waitlist mortality.
In this study, most urgency status cases, except for Status 0, were determined by functional status and PaO
2. The criteria of PFT and right heart catheterization were barely used. For example, in this system, patients with IPF and acute exacerbation dependent on high-flow nasal O
2 therapy had no priority over stable patients with chronic obstructive pulmonary disease and hypoxia being treated with long-term oxygen therapy. These patients with acute exacerbation of IPF had a higher chance of deteriorating to Status 0 or dying before they received LTx. This finding corresponded with a previous study of LAS simulation at a Korean LTx center. Status 1 patients had a wide range of LAS from 25 to 88.
7
Before the introduction of LAS in the United States, waiting time was used for allocation. Due to the high waitlist mortality, especially for IPF patients, the need for a new allocation system was raised. The LAS system, as a new allocation system, was designed to allocate donor lungs based on measures of medical urgency while avoiding futile transplants. The study reviewed 3103 cases of LTx that were recorded in the U.S. Register Organ Procurement & Transplantation Network.
56 The statistical model for waitlist mortality (medical urgency) and post-transplant survival (benefit) were developed based on clinical data. LAS has been revised by clinical data. In LAS system, predicted waitlist urgency and posttransplant survival are calculated using various clinical parameters such as age, height, weight, lung diagnosis, functional status, diabetes, need for assisted ventilation, O
2 requirement, PFT, right heart catheterization, partial pressure of carbon dioxide (PCO
2), serum creatinine levels, and serum bilirubin levels.
10 After introduction of LAS, reduction of waitlist mortality was observed.
6 The process of establishing LAS system might serve as an educational example for the Korean allocation system. To revise this system, we must review our clinical data to evaluate waitlist mortality according to urgency status, and evaluate parameters that are related to waitlist mortality.
Based on data from the United Network for Organ Sharing, among a total of 15934 LTx performed between 1987 and 2008, only 586 patients (3.7%) were on mechanical ventilation and 51 patients (0.3%) were on ECMO.
11 Recently, ECMO was reported to be used in up to 13% of all LTx in high-volume centers in the United States.
1213 However, in this study, 34.1% of patients were Status 0 and dependent on mechanical ventilation or ECMO preoperatively (32.9% on mechanical ventilation and 21.2% on ECMO). Status 0 patients had more intra- and postoperative complications and seemed to have poorer postoperative survival compared to other groups (
p=0.342). In a previous single-center study, Status 0 was significantly associated with poorer posttransplant survival than Status 1 (
p<0.001).
7 Currently, Status 0 has the highest priority for a donor lung, but it might have worse prognosis after transplantation than other urgency status designations. This study has revealed the need for an attempt to reduce lung transplantation in Status 0 patients.
This study had several limitations. First, this was a relatively small retrospective study with a short follow-up period. However, this was the first and only multi-institutional study that attempted to evaluate the Korean lung allocation system using nationwide LTx cohorts in Korea. As KOTRY study continues to enroll LTx patients and accumulate more data, KOTRY should help to better elucidate the problems faced in lung donor allocation and to revise the allocation system in the future. Second, this study cohort did not include patients who died while on the waitlist. Therefore, we could not find related parameters to predict waitlist mortality (i.e., urgency). Cooperation between lung transplantation centers is needed to find parameters related to waitlist mortality and to revise urgency criteria to better reflect true urgency.
In conclusion, the Korean urgency classification for LTx is determined using very limited parameters, and may not be a true reflection of urgency. Despite having the highest priority for donor lungs, Status 0 patients seem to have poor outcomes compared to other urgency status patients. Further multi-center and nationwide studies are needed to revise the lung allocation system to reflect true urgency and to provide the best benefit of lung transplantation.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download