Abstract
Purpose
To investigate the clinical features and prognosis associated with endogenous endophthalmitis (EE) in western Gyeongsangnam-do over an 11-year period.
Methods
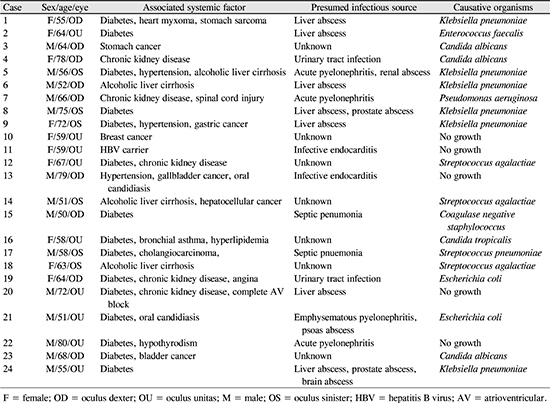
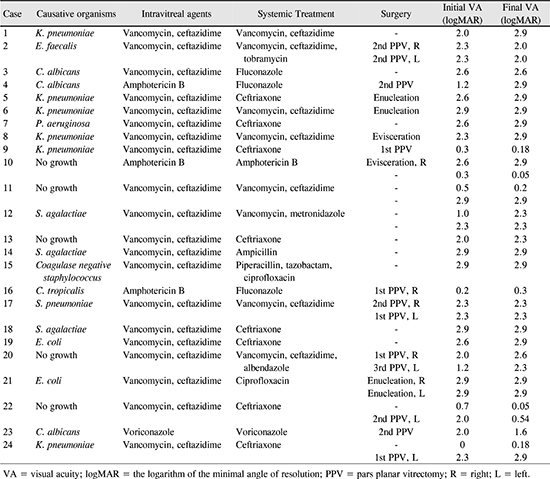
This study was a retrospective review of the medical records of 24 patients (33 eyes) who presented with endogenous endophthalmitis at the Gyeongsang National University Hospital from 2007 to 2017.
Results
The mean age of onset was 63.2 years, and 58.3% of the patients were men. Bilateral involvement was observed in nine patients (37.5%). Liver abscess (30.3%) and urinary tract infection (24.2%) were the most common extraocular sources of infection. Positive culture result was noted in 72.7% of the patients. The most common causative agents were gram-negative organisms (45.8%); the most commonly isolated microorganism was Klebsiella pneumoniae. Vitreous tapping and intravitreal antibiotic injection were performed in all patients; pars plana vitrectomy with intravitreal injection of antibiotics was performed in 12 eyes (36.4%). Enucleation and evisceration were performed in six eyes (18.2%). Initial visual acuity worse than hand motion was associated with a significantly worse visual outcome (p = 0.001).
Figures and Tables
 | Figure 1Identifiable associated systemic factors of patients with endogenous endophthalmitis. Diabetes is the leading systemic factor following cancer, chronic kidney disease and liver cirrhosis. |
 | Figure 2Identifiable presumed infection source of patients with endogenous endophthalmitis. Note that liver abscess is the leading cause of presumed infection source. |
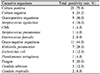
Table 2
Microbial isolates from blood, aqueous and vitreous samples of patients with endogenous endophthalmitis (n = 33)
References
1. Lee S, Um T, Joe SG, et al. Changes in the clinical features and prognostic factors of endogenous endophthalmitis: fifteen years of clinical experience in Korea. Retina. 2012; 32:977–984.
2. Relhan N, Forster RK, Flynn HW Jr. Endophthalmitis: then and now. Am J Ophthalmol. 2018; 187:xx–xxvii.

3. Schiedler V, Scott IU, Flynn HW Jr, et al. Culture-proven endogenous endophthalmitis: clinical features and visual acuity outcomes. Am J Ophthalmol. 2004; 137:725–731.

4. Leibovitch I, Lai T, Raymond G, et al. Endogenous endophthalmitis: a 13-year review at a tertiary hospital in South Australia. Scand J Infect Dis. 2005; 37:184–189.

5. Cho H, Shin YU, Siegel NH, et al. Endogenous endophthalmitis in the American and Korean Population: an 8-year retrospective study. Ocul Immunol Inflamm. 2018; 26:496–503.

6. Song JH, Chung IY, Park JM. A case of bilateral endogenous enterococcus faecalis endophthalmitis in liver abscess. J Korean Ophthalmol Soc. 2007; 48:1291–1296.

7. Kim IN, Moon SM, Chi MJ. Endogenous endophthalmitis due to klebsiella ozaenae. J Korean Ophthalmol Soc. 2016; 57:1139–1143.
8. Kim HA, Choi KS. Rapidly progressive endogenous endophthalmitis with subretinal abscess. J Korean Ophthalmol Soc. 2013; 54:1794–1799.

9. Lee MS, Chang MH. A case of bilateral endogenous endophthalmitis in a streptococcus pneumoniae meningitis patient. J Korean Ophthalmol Soc. 2013; 54:370–374.
10. Lee YW, Ha MM, Han SY, Bae JH. A case of endogenous streptococcus mitis endophthalmitis in a patient with staphylococcus aureus sepsis. J Korean Ophthalmol Soc. 2012; 53:1190–1193.
11. Han JM, Kim NJ. Two cases of bilateral endogenous klebsiella pneumoniae endophthalmitis in primary klebsiella pneumoniae liver abscess patients. J Korean Ophthalmol Soc. 2009; 50:1590–1594.

12. Hwang JH, Cho NC. Prognostic factors in patients with endogenous endophthalmitis. J Korean Ophthalmol Soc. 2009; 50:858–863.

13. Silpa-Archa S, Ponwong A, Preble JM, Foster CS. Culture-positive endogenous endophthalmitis: an eleven-year retrospective study in the central region of Thailand. Ocul Immunol Inflamm. 2018; 26:533–542.

14. The IONDT Research Group. The ischemic optic neuropathy decompression trial (IONDT): design and methods. Control Clin Trials. 1998; 19:276–296.
15. Deramo VA, Cox TA, Syed AB, et al. Vision-related quality of life in people with central retinal vein occlusion using the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2003; 121:1297–1302.

16. Faraawi R, Fong IW. Escherichia coli emphysematous endophthalmitis and pyelonephritis. Case report and review of the literature. Am J Med. 1988; 84(3 Pt 2):636–639.
17. Park SB, Searl SS, Aquavella JV, Erdey RA. Endogenous endophthalmitis caused by Escherichia coli. Ann Ophthalmol. 1993; 25:95–99.
18. Sadiq MA, Hassan M, Agarwal A, et al. Endogenous endophthalmitis: diagnosis, management, and prognosis. J Ophthalmic Inflamm Infect. 2015; 5:32.

19. Jackson TL, Eykyn SJ, Graham EM, Stanford MR. Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Surv Ophthalmol. 2003; 48:403–423.

20. Nishida T, Ishida K, Niwa Y, et al. An eleven-year retrospective study of endogenous bacterial endophthalmitis. J Ophthalmol. 2015; 2015:261310.

21. Lim HW, Shin JW, Cho HY, et al. Endogenous endophthalmitis in the Korean population: a six-year retrospective study. Retina. 2014; 34:592–602.
22. Park IH, Jun CH, Wi JW, et al. Prevalence of and risk factors for endogenous endophthalmitis in patients with pyogenic liver abscesses. Korean J Intern Med. 2015; 30:453–459.

23. Hunt JJ, Wang JT, Callegan MC. Contribution of mucoviscosityassociated gene A (magA) to virulence in experimental Klebsiella pneumoniae endophthalmitis. Invest Ophthalmol Vis Sci. 2011; 52:6860–6866.
24. Wiskur BJ, Hunt JJ, Callegan MC. Hypermucoviscosity as a virulence factor in experimental Klebsiella pneumoniae endophthalmitis. Invest Ophthalmol Vis Sci. 2008; 49:4931–4938.
25. Lee SY, Chee SP. Group B Streptococcus endogenous endophthalmitis: case reports and review of the literature. Ophthalmology. 2002; 109:1879–1886.
26. Edwards MS, Baker CJ. Group B streptococcal infections in elderly adults. Clin Infect Dis. 2005; 41:839–847.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download