Abstract
Purpose
To evaluate effectiveness of percutaneous transluminal angioplasty (PTA) for transposed brachiobasilic arteriovenous fistula (tBBAVF), and to analyze the factors influencing patency after PTA.
Materials and Methods
In 101 patients who underwent operation for tBBAVF from January 2006 to February 2008, we identified 42 patients undergoing PTA. We conducted a retrospective analysis of sequential PTAs in these patients from 2006 to 2017.
Results
A total of 100 PTAs were performed. The technical success rate was 93% and the clinical success was 100%. Only ruptures occurred in 12% as minor complications. Primary patency rate was 61%, 29%, 7%, and secondary patency was 91%, 82%, 59% at 6, 12, and 24 months, respectively. Primary patency rate was lower in tBBAVF with rupture (p = 0.024). Secondary patency rate was significantly lower in the diabetes (p = 0.002).
The transposed brachiobasilic arteriovenous fistula (tBBAVF) is the third AVF recommended for cases in which AVF creation is difficult in the wrist (radial-cephalic) or elbow (brachial-cephalic), according to the 2001 NKF-DOQI Clinical Practice Guidelines for Vascular Access (1). The tBBAVF was first introduced by Dagher et al. in 1976 (2). The creation of tBBAVF entails transposition of basilic vein. This process can kink or devascularize the venous segment, increasing the risk of stenosis and thrombosis compared with the brachiocephalic fistula where the vein is left in situ (3). On the other hand, it is more likely to mature and facilitates rapid outcomes since it uses superficially tunneled large basilic vein (3). Further, tBBAVF has a lower risk of thrombosis and infection compared with grafts (34). Based on its unique process and hemodynamic differences, it was hypothesized that the patency or the factors influencing patency may be distinct from that of the other native AVFs.
Percutaneous transluminal angioplasty (PTA) is an important procedure to treat stenosis of dysfunctional AVF (567), and is simple, safe, effective and widely used (89). The 2006 NKF-DOQI Clinical Practice Guidelines found that the factors affecting PTA longevity were not clearly identified and probably influenced by multiple factors including surgical techniques (10).
Turmel-Rodrigues et al. (5) and Neuen et al. (11) showed that upper arm AVFs were associated with shorter postintervention primary patency. However, these studies did not report tBBAVF from upper arm AVF separately. While many studies have reported patency and factors influencing outcome of PTA in AVF (5678111213), these studies may be limited by their exclusion or small numbers of tBBAVF.
The purposes of our study are to evaluate the patency of PTA for dysfunctional stenosis of tBBAVF and to analyze the influencing factors of patency.
Institutional Review Board approval was obtained for this study (IRB No. 2017-10-017-001) and the requirement for informed consent was waived.
In total, 101 patients underwent creation of tBBAVF at our hospital between January 2006 and February 2008. Of these patients, we identified 42 patients who underwent PTA. Characteristics of the study population are listed (Table 1).
We conducted a retrospective analysis of sequential PTAs in patients from January 2006 to March 2017. The study group included patients who had previous vascular access in the ipsilateral as well as the contralateral upper extremity. Comorbid conditions, the status of dialysis at the time of AVF placement, and history of central dialysis catheters were recorded.
No routine surveillance was performed for tBBAVF. We performed fistulography only when symptomatic fistula stenosis such as high pressure of the AVF, prolonged bleeding or inadequate volume flow was suspected.
All procedures were performed by two experienced interventional radiologists. Diagnostic fistulography was performed by inserting a 21-gauge (G) needle (Becton Dickinson, Sandy, UT, USA) into juxta-anastomosis of tBBAVF. Under conditions of decreased arterial inflow, we evaluated the stenosis of anastomotic site through reflux of contrast material via manual compression of proximal portion of puncture site. PTA was performed when stenosis was greater than 70% or was situation of clinical dysfunction. The same basic technique was used for all PTAs. In non-occluded AVF cases, after the puncture site anesthesia with 2% lidocaine hydrochloride, an 18-G needle was inserted into the tBBAVF near the anastomosis and a 0.035-inch guidewire was directed toward the stenotic site. After placement of a 7 french (F) vascular introducer sheath (Terumo, Corp., Tokyo, Japan or Cook Medical, Bloomington, IN, USA), the roadmap image was obtained. A balloon catheter was passed over the guide wire until the most proximal site of stenosis. Balloons with 5–14 mm diameter were used for stenosis (Blue Max/XXL/Cutting balloon, Boston Scientific, Natick, MA, USA or Conquest/Atlas, BARD, Covington, GA, USA). The contrast-filled balloon was inflated to 5 to 30 atmospheres of pressure and held for 1 to 2 min using an Encore 26 manual inflation device (Boston Scientific). We evaluated for residual stenosis, immediately after PTA using the roadmap image. Residual stenosis exceeding 30% was treated with 1–2 mm larger cutting balloon or a high-pressure balloon. Additional stent deployment was performed in case of residual stenosis greater than 50% or complications such as venous rupture. After the procedure, the puncture site was sutured, using a modified purse-string suture technique (14).
Occluded AVFs (n = 8) were either abandoned (n = 5) or recanalized using percutaneous mechanical thrombectomy (n = 3). We used the crossed-catheter technique (151617). The fistula was initially cannulated with a 21-G micropuncture set (Cook Medical). We advanced the 7 F Desilets-Hoffman sheath (Cook Medical) to the venous limb along a hydrophilic guidewire for aspiration thrombectomy. The thrombus was manually aspirated with Desilets-Hoffman sheath. A 7–8 mm × 4 cm balloon catheter was advanced into the drain vein and 3000 IU of heparin was administered. After completing the treatment of the venous limb, we performed aspiration thrombectomy of the arterial limb similarly. When wall-adherent thrombi such as the arterial plug remained in the anastomosis, we used a 5 F Fogarty thrombectomy balloon catheter (Baxter, Santa Ana, CA, USA) to pull the plug back into the midarterial limb of the AVF. An angioplasty balloon was used to break the plug. Immediately after the procedure, whole AVF angiography from the feeding artery to the superior vena cava was performed to treat residual stenosis or adherent thrombosis as needed.
We defined patency, technical and clinical success and categorized major and minor complication in accordance with Society of Interventional Radiology reporting standards (18).
Postintervention primary patency was defined as the interval from the time of the first endovascular intervention until rethrombotic occlusion, sequential intervention designed to maintain patency or reestablish patency, or the time of the last measurement of patency. The postintervention secondary patency was defined as the interval from the initial intervention until access abandonment, new surgical dialysis access or the longest recent follow-up period.
The technical success of PTA was defined as residual stenosis less than 30%. Clinical success was defined as resumption of normal dialysis after at least one session of treatment of a thrombosed access, reduction of recirculation to below threshold values after treatment of a stenosis, or continuous palpable thrill (no pulse) extending from the anastomosis.
Any procedural complications were also reviewed.
Each PTA was analyzed primarily for stenosis. Each stenosis was characterized by anatomic location, percentage, length of stenosis and number of stenotic sites. We categorized the stenotic sites anatomically into five groups: 1) central vein, 2) axillary vein, 3) mid portion of basilic vein, 4) juxta-anastomosis (within 3 cm of the arterial anastomosis), and 5) others.
We evaluated the effectiveness of PTA by calculating the postintervention primary and secondary patency rates using Kaplan-Meier survival analysis. The log-rank test was used to compare patency rates.
We used a multivariate Cox proportional hazards model to determine the risk factors for loss of primary or secondary patency according to angiographic findings, clinical variables and AVF age. Results are presented as hazard ratios with corresponding 95% confidence intervals. Statistical significance was assumed at two-sided p < 0.05. Analyses were carried out using SPSS 14.0 (SPSS Inc., Chicago, IL, USA).
A total of 100 PTAs was performed in 42 patients as follows: one PTA in 15 patients (35.7%), two PTAs in 9 patients (21.4%), three PTAs in 5 patients (11.9%), and four or more PTAs in 13 patients (30.9%).
The total number of stenotic sites was 142: one site in 63 PTAs (63.0%), two sites in 33 PTAs (33.0%), three or more sites in 4 PTAs (4.0%). The most common site of stenosis was the mid portion of the basilic vein (Fig. 1).
The technical success rate of PTA was 93% (Fig. 2). Technical failure was reported in 7 procedures (Fig. 3). However, all of them resulted in clinical success and underwent one or more dialysis sessions. The residual stenotic sites with more than 30% stenosis were innominate vein in 3 cases, mid portion of basilic vein in 2, axillary vein and juxta-anastomosis in a case each.
8 stents were inserted in 100 PTAs. Indications of stent deployment were residual stenosis due to elastic recoil in 6 cases, angioplasty-induced rupture of central vein in one case, and both residual stenosis and rupture at mid portion of basilica vein in one case. Mechanical thrombectomy was done in three cases.
There was no major complication after PTA. The only minor complication after PTA was ruptures. Twelve angioplasty-induced ruptures occurred in 12 procedures (12%). Seven ruptures occurred in the mid portion of basilic vein (58.3%), 4 in axillary vein (33.3%) and 1 in central vein (8.3%). Ten ruptures (83.3%) were treated successfully with endovascular balloon tamponade. A case of central venous rupture induced by angioplasty underwent stenting. Another case involving both angioplasty-induced rupture and residual stenosis of about 60% underwent covered stent insertion. No patient had local infection due to PTA in our study.
The mean follow-up was 56.6 months in 42 patients (range, 2.6 to 123.8 months) and 18 patients were lost to follow-up during the study.
The postintervention primary patency for PTA in tBBAVF was 61%, 29%, and 7% at 6, 12, and 24 months, respectively. The median period of postintervention primary patency was 6.5 months (Fig. 4). The postintervention secondary patency for PTA was 91%, 82%, and 59% at 6, 12, and 24 months, respectively. The median period of postintervention secondary patency was 43.1 months (Fig. 4).
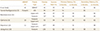
Predictors of postintervention patency for tBBAVF were analyzed using univariate and multivariate analysis and the results are summarized in Tables 2, 3, and 4.
The primary patency rate was only significantly lower in angioplasty-induced rupture (p = 0.024) (Table 3, Fig. 5). Other variables such as age above 75 years, sex, history of central venous catheterization, previous upper extremity access, multiple stenotic sites, location of stenosis, stenotic length greater than 2 cm and balloon type were not associated with any difference in postintervention primary or secondary patency (Tables 2, 3, and 4). The postintervention secondary patency rate was significantly lower only in the diabetes (p = 0.04) (Table 4, Fig. 6).
The tBBAVF is the third option of AVF when the radial-cephalic AVF or the brachial-cephalic AVF is unavailable (1). It entails a unique procedure of transposition of basilic vein and hemodynamic differences compared with other native AVFs (3). Hemodynamically significant stenosis inducing dysfunctional vascular access is a frequent complication warranting PTA to maintain patency.
In our study, about two-thirds of PTAs had single stenosis, which was similar to other reports (6713). The majority of previous studies reported that juxta-anastomosis site was the common stenotic site (5671319). However, most of the studies failed to analyze according to the type of native AVFs. Furthermore, the criteria for stenotic site classification varied among the reports. Rajan et al. (7) analyzed the stenotic site according to the type of native AVF and the frequency of stenotic sites varied according to the type of fistula. Stenosis was most prevalent within 3 cm of the arteriovenous anastomosis in 74 (64%) out of 116 dysfunctional radiocephalic fistulas and at the cephalic arch in 22 (30%) out of 74 dysfunctional brachiocephalic fistulas in their study (7). However, no studies reported exclusive analysis of the frequency of stenosis in tBBAVF. In our study, the most common stenotic site of tBBAVF involved the mid portion of basilic vein (31.7%) and the second most common stenotic site was axillary vein (26.8%) (Fig. 1). Mid-portion of the basilic vein is the site where the dialysis needle is punctured. The site of kinking of venous segment during the transposition of basilic vein is axillary vein (3).
Heye et al. (13) and Trerotola et al. (20) mentioned that the technical success varied according to the access type. In the study by Heye et al. (13), the technical success rate of tBBAVF was 87.5% and the success rate of radiocephalic AVF was 94.3%. In our study, the proportion of technical success of tBBAVF was 93% comparable to that of radiocephalic AVF.
Several studies have reported shorter postintervention patency of upper arm AVF compared with that of forearm AVF (57). Neuen et al. (11) mentioned that increased hemodynamic shear stresses, possibly due to higher flow rates and pressures in larger upper arm blood vessels, explained this observation. However, in our study, the patency rate of tBBAVF after angioplasty was as high as that of forearm AVF in other studies except for the study of Jeong et al., which had a higher rate of primary patency (Table 6) (568131921). There were no studies investigating the patency rates of a large number of tBBAVFs and further studies are needed.
Although many studies have investigated the factors that influence the postintervention patency of AVF, there are no conspicuous factors showing coherence (567811121319222324). The 2006 NKF-DOQI Clinical Practice Guidelines for Vascular Access suggest that the factors affecting PTA longevity have not been clearly elucidated and are probably influenced by a multitude of factors including surgical techniques (10). In addition, tBBAVF has a unique process of transposition of the venous segment, and we assumed that the hemodynamic differences of tBBAVF may have different factors affecting the patency, when compared with other types of vascular access.
Turmel-Rodrigues et al. (8) suggested that a minor overdilatation is preferable and carried low risk, since we now have the means of controlling any type of rupture percutaneously. A few studies reported successful covered stent deployment to salvage AVF complicated by venous rupture (2526). However, these were not reviewed according to the different types of AVF, especially tBBAVF. In our study, the primary postintervention patency rate of tBBAVF was significantly lower in angioplasty-induced rupture despite successful treatment with balloon tamponade or stent deployment (p = 0.024) (Table 3). The reason for this lower primary patency in angioplasty-induced rupture is unclear, however, tBBAVF may be vulnerable to rupture due to devascularization of the venous segment during transposition. In this study, the angioplasty-induced rupture occurred in 12% of tBBAVF, which was mainly in the mid portion of basilic vein, similar to the result of Turmel-Rodrigues et al. (5)
Beathard (22) investigated the success of angioplasty at different stenotic sites and found that angioplasty of subclavian vein stenosis resulted in poor long-term success. Our study also showed similar results indicating that the presence of central vein stenosis almost significantly lower in the postintervention primary patency than in other stenotic sites (p = 0.053) (Fig. 7).
While several studies have reported that patency of PTA is related to stenotic length (61219), no relationship between stenotic length of tBBAVF and patency was identified in our study (p = 0.98). The majority of subjects in previous studies were radiocephalic AVFs, which may be responsible for the differences between studies.
The central dialysis catheters were found to be vulnerable to infection and thrombus, and subsequent stenosis interfered with the creation of a future arteriovenous access (823). However, a history of upper extremity vascular access as well as central dialysis catheter insertion was not associated with postintervention patency in our study (Table 2).
Other studies reported that clinical variables except diabetes did not affect the postintervention primary or secondary patency (6111213). In our study, diabetes was the only factor that lowered postintervention secondary patency (p = 0.04) (Fig. 6). The result suggesting that diabetes lowers the patency of PTA is similar to the study of Clark et al. (6) and Heye et al. (13).
As shown in many studies, a younger AVF age was associated with poor postintervention patency (561113), probably due to immature AVF as reported by Manninen et al (27). These may be supported by our results that more common stenosis was noted at the axillary vein in the younger tBBAVF than in the older tBBAVF (46.1% vs. 11.8%). The axillary vein is vulnerable to maturation due to transposed segment of tBBAVF. However, previous studies had a limitation in that the majority of native AVFs were forearm AVF and the number of upper arm AVF as well as tBBAVF was small. The relationship between tBBAVF age and postintervention patency in our study was contrary to the results of most previous studies (561113). In our study, no statistically significant loss of postintervention primary or secondary patency was observed in young AVF stratified into groups younger than and older than 6 months or 1 year. We assumed that postintervention patency of tBBAVF was less affected by AVF age because maturation of tBBAVF was nearly a month faster than other native AVFs (3).
The major limitation of this study was its retrospective design, limitation to a single institution without a control group. However, compared with other studies to date, we analyzed the largest number of PTAs of tBBAVFs. We did not analyze the effect of technical success on postintervention patency due to the small number of technical failures. However, most studies reported no association between technical success and postintervention patency (61328).
In conclusion, PTA is a safe and effective intervention for dysfunctional stenosis of tBBAVF based on its unique transposition of the venous segment. We suggest that repeated PTAs in tBBAVF are acceptable due to excellent secondary patency and absence of major complication. Loss of postintervention primary patency of tBBAVF is influenced by angioplasty-induced rupture and possibly central vein stenosis. Diabetes per se has a significant effect on postintervention secondary patency. Patients with tBBAVF with these additional risk factors may need frequent surveillance to prolong AVF longevity.
Figures and Tables
 | Fig. 2A 64-year-old man with technically successful percutaneous transluminal angioplasty.
A. Preprocedural fistulogram shows severe juxta-anastomotic stenosis in transposed brachiobasilic arteriovenous fistula. Stenotic site (arrow).
B. A 6 mm × 80 mm balloon was used to treat this lesion.
C. Stenosis was completely resolved after angioplasty without complication. Stenotic site (arrow).
|
 | Fig. 3A 63-year-old woman who underwent a technically failed but clinically successful percutaneous transluminal angioplasty.
A. Preprocedural angiogram shows stenosis in the axillary vein in transposed brachiobasilic arteriovenous fistula. Stenotic site (arrow).
B. A 5 mm × 20 mm cutting balloon was used to treat this lesion.
C. Roadmap image after ballooning shows residual stenosis of about 50%. Stenotic site (arrow).
|
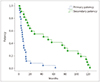 | Fig. 4Kaplan-Meier curves of postintervention primary and secondary patency for transposed brachiobasilic arteriovenous fistula. |
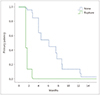 | Fig. 5Postintervention primary patency for transposed brachiobasilic arteriovenous fistula with angioplasty-induced rupture and non-rupture (p = 0.024). |
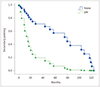 | Fig. 6Postintervention secondary patency for transposed brachiobasilic arteriovenous fistula with diabetes (p = 0.04). DM = diabetes mellitus. |
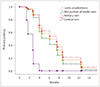 | Fig. 7Postintervention primary patency according to location of stenotic site. Central vein stenosis showed borderline significant lower postintervention primary patency when compared with other stenotic sites in patients with a single stenotic site in transposed brachiobasilic arteriovenous fistula (hazard ratio, 15.267; 95% confidence interval, 0.962 to 242.389; p = 0.053). |
Table 5
HRs for Reduced Postintervention Primary Patency with Location of Stenotic Site Based on Cox Selectivity

References
1. III. NKF-K/DOQI clinical practice guidelines for vascular access: update 2000. Am J Kidney Dis. 2001; 37:S137–S181.
2. Dagher F, Gelber R, Ramos E, Sadler J. The use of basilic vein and brachial artery as an A-V fistula for long term hemodialysis. J Surg Res. 1976; 20:373–376.

3. Oliver MJ, McCann RL, Indridason OS, Butterly DW, Schwab SJ. Comparison of transposed brachiobasilic fistulas to upper arm grafts and brachiocephalic fistulas. Kidney Int. 2001; 60:1532–1539.

4. Weale AR, Bevis P, Neary WD, Lear PA, Mitchell DC. A comparison between transposed brachiobasilic arteriovenous fistulas and prosthetic brachioaxillary access grafts for vascular access for hemodialysis. J Vasc Surg. 2007; 46:997–1004.

5. Turmel-Rodrigues L, Pengloan J, Baudin S, Testou D, Abaza M, Dahdah G, et al. Treatment of stenosis and thrombosis in haemodialysis fistulas and grafts by interventional radiology. Nephrol Dial Transplant. 2000; 15:2029–2036.
6. Clark TW, Hirsch DA, Jindal KJ, Veugelers PJ, LeBlanc J. Outcome and prognostic factors of restenosis after percutaneous treatment of native hemodialysis fistulas. J Vasc Interv Radiol. 2002; 13:51–59.

7. Rajan DK, Bunston S, Misra S, Pinto R, Lok CE. Dysfunctional autogenous hemodialysis fistulas: outcomes after angioplasty--are there clinical predictors of patency? Radiology. 2004; 232:508–515.

8. Turmel-Rodrigues L, Pengloan J, Bourquelot P. Interventional radiology in hemodialysis fistulae and grafts: a multidisciplinary approach. Cardiovasc Intervent Radiol. 2002; 25:3–16.

9. Glass C, Porter J, Singh M, Gillespie D, Young K, Illig K. A large-scale study of the upper arm basilic transposition for hemodialysis. Ann Vasc Surg. 2010; 24:85–91.

10. Gilmore J. KDOQI clinical practice guidelines and clinical practice recommendations—2006 updates. Nephrol Nurs J. 2006; 33:487–488.
11. Neuen BL, Gunnarsson R, Baer RA, Tosenovsky P, Green SJ, Golledge J, et al. Factors associated with patency following angioplasty of hemodialysis fistulae. J Vasc Interv Radiol. 2014; 25:1419–1426.

12. Maeda K, Furukawa A, Yamasaki M, Murata K. Percutaneous transluminal angioplasty for Brescia-Cimino hemodialysis fistula dysfunction: technical success rate, patency rate and factors that influence the results. Eur J Radiol. 2005; 54:426–430.

13. Heye S, Maleux G, Vaninbroukx J, Claes K, Kuypers D, Oyen R. Factors influencing technical success and outcome of percutaneous balloon angioplasty in de novo native hemodialysis arteriovenous fistulas. Eur J Radiol. 2012; 81:2298–2303.

14. Simons ME, Clark TW, Rajan DK. The woggle technique: a new method of suture closure of hemodialysis arteriovenous grafts and fistulas after percutaneous interventions. J Vasc Interv Radiol. 2001; 12:S30.
15. Cohen MA, Kumpe DA, Durham JD, Zwerdlinger SC. Improved treatment of thrombosed hemodialysis access sites with thrombolysis and angioplasty. Kidney Int. 1994; 46:1375–1380.

16. Goo DE, Kim JH, Park ST, Chang YW, Kwon KH, Choi DL, et al. Usefulness of thromboaspiration with desilets-Hoffman sheath in thrombosed hemodialysis access graft. J Korean Radiol Soc. 2004; 51:45–53.

17. Turmel-Rodrigues L, Pengloan J, Rodrigue H, Brillet G, Lataste A, Pierre D, et al. Treatment of failed native arteriovenous fistulae for hemodialysis by interventional radiology. Kidney Int. 2000; 57:1124–1140.

18. Gray RJ, Sacks D, Martin LG, Trerotola SO;. Reporting standards for percutaneous interventions in dialysis access. J Vasc Interv Radiol. 2003; 14:S433–S442.

19. Jeong SM, Kim JH, Byun SS, Kang JM, Choi ST, Kim JW, et al. Effect of percutaneous transluminal angioplasty on the stenosis of autogenous radiocephalic arteriovenous fistula for hemodialysis. J Korean Soc Radiol. 2016; 74:105–113.

20. Trerotola SO, Kwak A, Clark TW, Mondschein JI, Patel AA, Soulen MC, et al. Prospective study of balloon inflation pressures and other technical aspects of hemodialysis access angioplasty. J Vasc Interv Radiol. 2005; 16:1613–1618.

21. Manninen HI, Kaukanen ET, Ikäheimo R, Karhapää P, Lahtinen T, Matsi P, et al. Brachial arterial access: endovascular treatment of failing Brescia-Cimino hemodialysis fistulas—initial success and long-term results. Radiology. 2001; 218:711–718.

22. Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992; 42:1390–1397.

23. Hodges TC, Fillinger MF, Zwolak RM, Walsh DB, Bech F, Cronenwett JL. Longitudinal comparison of dialysis access methods: risk factors for failure. J Vasc Surg. 1997; 26:1009–1019.
24. Quinn SF, Schuman ES, Demlow TA, Standage BA, Ragsdale JW, Green GS, et al. Percutaneous transluminal angioplasty versus endovascular stent placement in the treatment of venous stenoses in patients undergoing hemodialysis: intermediate results. J Vasc Interv Radiol. 1995; 6:851–855.

25. Funaki B, Szymski GX, Leef JA, Rosenblum JD, Burke R, Hackworth CA. Wallstent deployment to salvage dialysis graft thrombolysis complicated by venous rupture: early and intermediate results. AJR Am J Roentgenol. 1997; 169:1435–1437.

26. Dale JD, Dolmatch BL, Duch JM, Winder R, Davidson IJ. Expanded polytetrafluoroethylene-covered stent treatment of angioplasty-related extravasation during hemodialysis access intervention: technical and 180-day patency. J Vasc Interv Radiol. 2010; 21:322–326.

27. Manninen HI, Kaukanen E, Mäkinen K, Karhapää P. Endovascular salvage of nonmaturing autogenous hemodialysis fistulas: comparison with endovascular therapy of failing mature fistulas. J Vasc Interv Radiol. 2008; 19:870–876.

28. Forauer AR, Hoffer EK, Homa K. Dialysis access venous stenoses: treatment with balloon angioplasty—1-versus 3-minute inflation times. Radiology. 2008; 249:375–381.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download