Abstract
Pseudoaneurysm formation in the profunda femoris artery (PFA) is a rare complication of femur shaft fractures or, more usually, a consequence of operative repair. Over the past few years, percutaneous transcatheter arterial embolization (TAE) has increasingly been considered the most effective treatment for pseudoaneurysms of the PFA. We report two cases with pseudoaneurysms of the PFA that were caused by femur shaft fractures and were successfully treated using TAE with n-butyl cyanoacrylate (NBCA). When a pseudoaneurysm of the PFA occurs due to a femur shaft fracture, early recognition and prompt radiologic intervention may prevent severe vascular injury without the need for additional surgery. The advent of TAE using NBCA enables minimally invasive treatment to be undertaken and it is effective for managing pseudoaneurysms of the PFA.
Pseudoaneurysms are rarely formed in the profunda femoris artery (PFA). These pseudoaneurysms are caused by penetrating and blunt trauma to the thigh and orthopedic procedures of the proximal femur (1). The symptomatic injury usually manifests as a hemorrhage; however, it is likely that many injuries are subclinical and remain undetected. Angiography and computed tomography angiography (CTA) can confirm the presence of the PFA pseudoaneurysm, and transcatheter arterial embolization (TAE) is now regarded as the treatment of choice for this condition (23). This report describes two cases with pseudoaneurysms of the PFA caused by femoral fractures. Both cases were successfully treated using TAE with n-butyl cyanoacrylate (NBCA).
A 26-year-old male patient presented to our hospital, following a car accident, with multiple traumas that included a comminuted fracture of the proximal femoral shaft. Computer tomography (CT) revealed active bleeding from the right colic artery, arising from the superior mesenteric artery. The patient underwent a right hemicolectomy and a right colic artery ligation on admission. Postoperatively, the blood pressure and pulse rate were stable; however, on the fifth postoperative day, the hemoglobin level reduced from 11.3 mg/dL to 4.6 mg/dL, necessitating a massive packed red blood cell transfusion. A tense, tender swelling had developed in the left thigh, and the wound was oozing. A vascular injury was suspected to have been caused by the femoral shaft fracture. An urgent CTA was performed, which revealed a 1.2-cm pseudoaneurysm arising from a branch of the left PFA (Fig. 1A). We proceeded to conduct angiography for a more detailed evaluation and to determine whether the patient required endovascular treatment. The left PFA was catheterized via the right femoral artery, and the angiography revealed a pseudoaneurysm that arose from the bifurcation of the second deep perforating branch of the PFA (Fig. 1B). The feeding branch was superselectively catheterized using a 2.0-French microcatheter system (Progreat®, Terumo, Tokyo, Japan) coaxially and was embolized using gelfoam (Spongostan®, Johnson & Johnson, Gauteng, South Africa). However, the first attempt was unsuccessful because the gelfoam pieces passed freely into the distal arteries. Subsequently, we resorted to NBCA (B. Braun Medical AG, Sempach, Switzerland) as the embolic agent. A 1:3 mixture of NBCA and iodized oil (Lipiodol, Terumo, Tokyo, Japan) was injected, followed by a contrast medium injection that demonstrated the disappearance of the pseudoaneurysm (Fig. 1C). Five days after the embolization, the patient underwent a closed reduction and internal fixation of the left femoral shaft fracture. The patient recovered well and was discharged 8 weeks after the embolization. No complications were noted at the 15-month follow-up assessment.
A 71-year-old male patient presented to our hospital with multiple traumas after a fall. The thigh CT scan revealed a comminuted fracture of the femur with displacement. A physical examination of the patient showed that the right thigh was swollen, and the vitals became unstable with systolic blood pressure dropping to 70 mm of Hg and hemoglobin level at 8.9 g/dL; therefore, a vascular injury caused by a femoral shaft fracture was strongly suspected. Hence, the patient was referred directly for emergent angiography without any imaging evaluations, such as the CTA. The right PFA was catheterized via the left femoral artery, and selective angiography demonstrated pseudoaneurysm (1.4 × 1.0 cm) that arose from the third deep perforating branch of the PFA (Fig. 2A). The feeding branch was superselectively catheterized using a 2.2-French microcatheter system (Progreat®) coaxially, but the pseudoaneurysm was too deep to enable advancement of the coils. Thus, the embolization was performed using a 1:2 mixture of NBCA and iodized oil. A subsequent angiography showed the successful exclusion of the pseudoaneurysm (Fig. 2B). On the first day after the embolization, the patient underwent an open reduction and internal fixation of the right femoral shaft fracture. There was no evidence of recurrent bleeding or procedure-related complications at the 6-month follow-up assessment.
Pseudoaneurysms of the PFA are uncommon and account for approximately 2% of peripheral arterial wounds (4). Since the PFA lies deep within the thigh and is protected from external trauma by the vastus medialis muscle, it is most vulnerable to injury in the sub-trochanteric area (1). Arterial injury can occur because of drills, screws, bone spike, displaced implants, and even retraction of surrounding tissue (5). Most of the arterial injuries are associated with iatrogenic injuries, such as operative repairs that cause pseudoaneurysm of the PFA more frequently compared with fracture, and damage to the PFA by femoral fracture has rarely been reported (6). In these cases, the pseudoaneurysm was detected before the surgical fixation of the femoral shaft fracture, and hence, the pseudoaneurysm of the PFA was presumed to have been caused by direct traumatic injury such as pressure of a sharp bone fragment.
PFA injuries may be overlooked because of delay in their presentation, and an accurate diagnosis is difficult because this artery is located deep within the thigh. Clinical signs including a tense thigh swelling, hip pain caused by direct pressure, or persistent or recurrent anemia caused by the continuing hemorrhage should suggest pseudoaneurysm formation (1).
Several techniques can be used to diagnose pseudoaneurysm, including gray-scale and duplex Doppler ultrasound, CT, magnetic resonance imaging, and angiography. CTA enables three-dimensional reformatting of the vasculature of the lower extremity and is a quick and non-invasive method with high levels of sensitivity (90–95%) and specificity (98–100%) for detecting arterial injury after trauma (7). Angiography is the best technique for detecting vascular pathologies, especially in bleeding cases, because it provides valuable information about the site and the size of the pseudoaneurysm, the feeding vessels, and the patency and adequacy of the distal flow. In our first case, where the patient was hemodynamically stable but showed reduced hemoglobin levels, a pseudoaneurysm of the PFA was identified using CTA on the fifth day after admission. The second patient was directly referred for emergent angiography, because he was hemodynamically unstable on admission. Therefore, if a patient with a comminuted femoral fracture is hemodynamically unstable or presents high clinical suspicion of active bleeding, careful examinations including CTA or angiography of the injured area should be performed.
Three options exist for the management of a pseudoaneurysm. Ultrasound-guided thrombin injections have been used to successfully treat femoral artery aneurysms since 1986, and this technique was first used to treat a pseudoaneurysm of the PFA in 1987 (8). This approach is safe and effective with success rates of up to 93%; however, it is not suitable for all cases because the presence of a large hematoma complicates the identification of the feeding vessel using ultrasound, and cannulating a deep-seated or small aneurysm is technically challenging (8). The surgical management of a pseudoaneurysm involves a sizable incision and exposure of the artery through the hematoma. This is the treatment of choice when a rupture, limb ischemia, compressive neuropathy, distal embolization, skin necrosis, and an infection are present, but the incidence of postoperative complications can be as high as 20% with the mortality rate up to 3% (9). The third option for the management of a pseudoaneurysm is percutaneous TAE, which is increasingly considered to be the most effective treatment for a PFA pseudoaneurysm (2). Hence, an endovascular approach seems to be a significant and effective alternative to surgical treatment, because it is minimally invasive and is associated with a short and relatively painless recovery period.
TAE of a pseudoaneurysm can be achieved using embolic agents that include coils, polyvinyl alcohol, NBCA, autologous clots, and gelfoam (10). The PFA has a collateral supply; therefore, the regions that are proximal and distal to the pseudoaneurysm must be embolized to exclude the pseudoaneurysm from the circulation completely by preventing backflow from the collateral circulation. NBCA has the advantage of being rapidly delivered to the site of the bleeding. Other potential advantages of NBCA include its capacity to obliterate small distal vessels that can be reached by a microcatheter, and its effective occlusion of bleeding sites that have complex anatomical structures. Although the danger of damaging a limb's circulation should be considered, preservation of the collateral branches maintains adequate supply to the muscle groups that PFA supplies (10). In both our cases, NBCA was used as the embolic agent because the gelfoam piece passed freely into the distal arteries in the first patient, and the pseudoaneurysm that formed in the second patient was too deep to enable coils to be advanced. There was no evidence of procedure-related complications during the follow-up periods after the embolization. NBCA can be considered a safe and effective embolic agent, particularly for pseudoaneurysms that arise below the second branch of the PFA.
When a patient presents with a pseudoaneurysm of the PFA accompanied by femoral shaft fracture, early recognition and prompt radiologic interventions help to ensure that the vessel injuries caused by the fracture can be treated without the need for additional surgery. The advent of TAE with NBCA has facilitated minimally invasive treatment and effective management of PFA pseudoaneurysms.
Figures and Tables
 | Fig. 1A 26-year-old male admitted for a left femur fracture (Case 1).
A. An axial computed tomography scan obtained five days after admission shows a pseudoaneurysm (arrow) within the left adductor magnus muscle.
B. Angiography via the left femoral artery demonstrates a pseudoaneurysm (arrowhead) arising from the bifurcation of the second deep perforating branch of the profunda femoris artery.
C. An angiography after injection of a 1:3 mixture of n-butyl cyanoacrylate and iodized oil demonstrates the occluded feeding artery and the pseudoaneurysm.
|
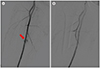 | Fig. 2A 71-year-old man admitted for a right femur fracture (Case 2).
A. Selective angiography demonstrates a feeding artery and the pseudoaneurysm (arrow) that arises from the third deep perforating branch of the profunda femoris artery.
B. Embolization with a 1:2 mixture of n-butyl cyanoacrylate and iodized oil was performed, and a subsequent angiography shows the successful exclusion of the pseudoaneurysm.
|
References
1. Hanna GB, Holdsworth RJ, McCollum PT. Profunda femoris artery pseudoaneurysm following orthopaedic procedures. Injury. 1994; 25:477–479.

2. Entwisle JJ, De Nunzio M, Hinwood D. Case report: transcatheter embolization of pseudoaneurysm of the profunda femoris artery complicating fracture of the femoral neck. Clin Radiol. 2001; 56:424–427.
3. Waldherr C, Kickuth R, Ludwig K, Do DD, Triller J. Superselective embolization of deep femoral artery branch pseudoaneurysm with a coaxial microcatheter system. Vasa. 2006; 35:45–49.

4. Loubeau JM, Bahnson HT. Traumatic false aneurysm and arteriovenous fistula of the profunda femoris artery: surgical management and review of the literature. Surgery. 1977; 81:222–227.
5. Chong KC, Yap EC, Lam KS, Low BY. Profunda femoris artery pseudoaneurysm presenting with triad of thigh swelling, bleeding and anaemia. Ann Acad Med Singapore. 2004; 33:267–269.
6. Naouli H, Jiber H, Bouarhroum A. False aneurysm of perforating branch of the deep femoral artery-report of two cases. Int J Surg Case Rep. 2015; 14:36–39.

7. Miller-Thomas MM, West OC, Cohen AM. Diagnosing traumatic arterial injury in the extremities with CT angiography: pearls and pitfalls. Radiographics. 2005; 25:Suppl 1. S133–S142.

8. Walker TG, Geller SC, Brewster DC. Transcatheter occlusion of a profunda femoral artery pseudoaneurysm using thrombin. AJR Am J Roentgenol. 1987; 149:185–186.

9. Sedwitz MM, Hye RJ, Stabile BE. The changing epidemiology of pseudoaneurysm. Therapeutic implications. Arch Surg. 1988; 123:473–447.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download