Abstract
Purpose
To evaluate the efficiency of a surgical method using original breaks to drain subretinal fluid without using retinotomy and perfluorocarbon liquid for patients with rhegmatogenous retinal detachment (RRD).
Methods
A retrospective chart review comparing 41 eyes of 41 patients who received vitrectomy, and used original breaks to drain subretinal fluid without using perfluorocarbon liquid, and 40 eyes of 40 patients who received vitrectomy using perfluorocarbon liquid for simple RRD between February 2014 and December 2017 was conducted. All patients were followed for a minimum of 6 months after surgery.
Results
The primary anatomical success percentages were 97.6% and 97.5% for groups that did not and did use perfluorocarbon liquid, respectively. Retinal detachment recurred in one eye from both groups. The final success percentage was 100%. The preoperative mean logMAR best-corrected visual acuity (BCVA) of 0.87 ± 0.80 improved to 0.30 ± 0.30 at postoperative 6 months for the group that did not use perfluorocarbon liquid, while it improved from 0.86 ± 0.71 to 0.42 ± 0.52 for the group that did use perfluorocarbon liquid. Both groups showed significant BCVA improvement (p < 0.01). There was no significant difference in the incidence of complications caused by the use of perfluorocarbon liquid.
Figures and Tables
 | Figure 1Summary of vitrectomy without perfluorocarbon liquid. (A) Before fluid air exchange, advanced DSP backflush soft tip is on retinal tear. (B) After fluid air exchange and subretinal fluid drainage through original retinal break, there is remained subretinal fluid at posterior pole. (C) Before endolaser photocoagulation around retinal tear with scleral indentation. (D) After endolaser photocoauglation around retinal tear. |
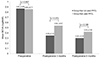 | Figure 2Changes in best corrected visual acuity (BCVA). In group that not used perfluorocarbon liquid (PFCL), preoperative mean logarithm of minimal angle of resolution (logMAR) BCVA was 0.87 ± 0.80. Postoperative mean logMAR BCVA was improved to 0.35 ± 0.31 at 3 months after operation (*p < 0.01) and 0.30 ± 0.30 at 6 months after operation (*p 0.01). In group that used PFCL, preoperative mean logMAR BCVA was 0.86 ± 0.71. Postoperative mean logMAR BCVA was improved to 0.54 ± 0.57 at 3 months after operation (*p = 0.05) and 0.42 ± 0.52 (*p 0.01) at 6 months. There was no significant difference in BCVA between two groups (†p > 0.05). Values are presented as mean ± standard deviation unless otherwise indicated. *The one-way analysis of variance; †independent t-test. |
Notes
References
1. Park SJ, Choi NK, Park KH, Woo SJ. Five year nationwide incidence of rhegmatogenous retinal detachment requiring surgery in Korea. PLoS One. 2013; 8:e80174.

2. Kuhn F, Aylward B. Rhegmatogenous retinal detachment: a reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014; 51:15–31.

3. Choi SW, Kim KS, Kim YC. Clinical characteristics of rhegmatogenous retinal detachment in patients under 40 years of age. J Korean Ophthalmol Soc. 2014; 55:1808–1813.

4. Heimann H, Bartz-Schmidt KU, Bornfeld N, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007; 114:2142–2154.
5. Haimann MH, Burton TC, Brown CK. Epidemiology of retinal detachment. Arch Ophthalmol. 1982; 100:289–292.

6. Assi AC, Charteris DG, Pearson RV, Gregor ZJ. Pneumatic retinopexy in the treatment of primary rhegmatogenous retinal detachment. Eye (Lond). 1999; 13:725–728.

7. Minihan M, Tanner V, Williamson TH. Primary rhegmatogenous retinal detachment: 20 years of change. Br J Ophthalmol. 2001; 85:546–548.

8. Escoffery RF, Olk RJ, Grand MG, Boniuk I. Vitrectomy without scleral buckling for primary rhegmatogenous retinal detachment. Am J Ophthalmol. 1985; 99:275–281.

9. Chang S, Lincoff H, Zimmerman NJ, Fuchs W. Giant retinal tears. Surgical techniques and results using perfluorocarbon liquids. Arch Ophthalmol. 1989; 107:761–766.
10. Verstraeten T, Williams GA, Chang S, et al. Lens-sparing vitrectomy with perfluorocarbon liquid for the primary treatment of giant retinal tears. Ophthalmology. 1995; 102:17–20.

11. McDonald HR, Lewis H, Aaberg TM, Abrams GW. Complications of endodrainage retinotomies created during vitreous surgery for complicated retinal detachment. Ophthalmology. 1989; 96:358–363.

12. Berglin L, Ren J, Algvere PV. Retinal detachment and degeneration in response to subretinal perfluorodecalin in rabbit eyes. Graefes Arch Clin Exp Ophthalmol. 1993; 231:233–237.

13. Cauchi P, Azuara-Blanco A, McKenzie J. Corneal toxicity and inflammation secondary to retained perfluorodecalin. Am J Ophthalmol. 2005; 140:322–323.

14. Tewari A, Eliott D, Singh CN, et al. Changes in retinal sensitivity from retained subretinal perfluorocarbon liquid. Retina. 2009; 29:248–250.

16. Gartry DS, Chignell AH, Franks WA, Wong D. Pars plana vitrectomy for the treatment of rhegmatogenous retinal detachment uncomplicated by advanced proliferative vitreoretinopathy. Br J Ophthalmol. 1993; 77:199–203.

17. Campo RV, Sipperley JO, Sneed SR, et al. Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology. 1999; 106:1811–1815.

18. Woon WH, Burdon MA, Green WT, Chignell AH. Comparison of pars plana vitrectomy and scleral buckling for uncomplicated rhegmatogenous retinal detachment. Curr Opin Ophthalmol. 1995; 6:76–79.
19. Newman DK, Burton RL. Primary vitrectomy for pseudophakic and aphakic retinal detachments. Eye (Lond). 1999; 13:635–639.

20. Bartz-Schmidt KU, Kirchhof B, Heimann K. Primary vitrectomy for pseudophakic retinal detachment. Br J Ophthalmol. 1996; 80:346–349.

22. Fine HF, Iranmanesh R, Iturralde D, Spaide RF. Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology. 2007; 114:1197–1200.

23. Sonoda Y, Yamakiri K, Sonoda S, et al. Endoscopy-guided subretinal fluid drainage in vitrectomy for retinal detachment. Ophthalmologica. 2006; 220:83–86.

24. Martínez-Castillo VJ, García-Arumí J, Boixadera A. Pars plana vitrectomy alone for the management of pseudophakic rhegmatogenous retinal detachment with only inferior breaks. Ophthalmology. 2016; 123:1563–1569.

25. Lee SJ, Kwon HJ, Park KY, et al. Prognostic factors of anatomical success in microincisional vitrectomy for rhegmatogenous retinal detachment. J Korean Ophthalmol Soc. 2016; 57:1613–1618.

26. Lv Z, Li Y, Wu Y, Qu Y. Surgical complications of primary rhegmatogenous retinal detachment: a meta-analysis. PLoS one. 2015; 10:e0116493.

27. Yamaguchi M, Ataka S, Shiraki K. Subretinal fluid drainage via original retinal breaks for rhegmatogenous retinal detachment. Can J Ophthalmol. 2014; 49:256–260.

28. Yokoyama S, Kojima T, Mori T, et al. Clinical outcomes of endoscope-assisted vitrectomy for treatment of rhegmatogenous retinal detachment. Clin Ophthalmol. 2017; 11:2003–2010.

29. Quintyn JC, Brasseur G. Subretinal fluid in primary rhegmatogenous retinal detachment: physiopathology and composition. Surv Ophthalmol. 2004; 49:96–108.

30. Chen X, Zhang Y, Yan Y, et al. Complete subretinal fluid drainage is not necessary during vitrectomy surgery for macula-off rhegmatogenous retinal detachment with peripheral breaks: a prospective, nonrandomized comparative interventional study. Retina. 2017; 37:487–493.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download