This article has been
cited by other articles in ScienceCentral.
Abstract
Background and Objectives
This study aimed to confirm the effects of traditional holidays on the incidence and outcomes of out-of-hospital cardiac arrest (OHCA) in South Korea.
Methods
We studied 95,066 OHCAs of cardiac cause from a nationwide, prospective study from the Korea OHCA Registry from January 2012 to December 2016. We compared the incidence of OHCA, in-hospital mortality, and neurologic outcomes between traditional holidays, Seollal (Lunar New Year's Day) and Chuseok (Korean Thanksgiving Day), and other day types (weekday, weekend, and public holiday).
Results
OHCA occurred more frequently on traditional holidays than on the other days. The median OHCA incidence were 51.0 (interquartile range [IQR], 44.0–58.0), 53.0 (IQR, 46.0–60.5), 52.5 (IQR, 45.3–59.8), and 60.0 (IQR, 52.0–69.0) cases/day on weekday, weekend, public holiday, and traditional holiday, respectively (p<0.001). The OHCA occurred more often at home rather than in public place, lesser bystander cardiopulmonary resuscitation (CPR) was performed, and the rate of cessation of CPR within 20 minutes without recovery of spontaneous circulation was higher on traditional holiday. After multivariable adjustment, traditional holiday was associated with higher in-hospital mortality (adjusted hazard ratio [HR], 1.339; 95% confidence interval [CI], 1.058–1.704; p=0.016) but better neurologic outcomes (adjusted HR, 0.503; 95% CI, 0.281–0.894; p=0.020) than weekdays.
Conclusions
The incidence of OHCAs was associated with day types in a year. It occurred more frequently on traditional holidays than on other day types. It was associated with higher in-hospital mortality and favorable neurologic outcomes than weekday.
Keywords: Epidemiology, Out-of-hospital cardiac arrest, Mortality, Heart arrest
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) is a major healthcare burden globally and is associated with very high mortality and morbidity.
1)2) OHCA occurs in >30,000 individuals in South Korea, but the survival rate is 3.0% with a favorable neurologic recovery rate of 0.9%, which is lower than that of the global rate.
2)3)4) Successful resuscitation requires implementing a complete “chain of survival,” and identifying the characteristics of OHCA is important to find the missing link in the chain.
3)
Prior studies have suggested temporal variability in OHCA, and a few have suggested circaseptan variability in occurrence and outcomes.
5)6)7) However, these studies are limited in other nations and do not consider any differences in the OHCA incidence between the holiday and weekend. Because the variability between day type (weekday, weekend, public holiday, traditional holiday) is cultural, further understanding of the day type variability of OHCA occurrence and outcomes in South Korea is important to develop preventative strategies and optimize resource planning for prehospital and in-hospital response to cardiac arrest, with the aim of improving patient survival.
8)9)10)
Every year, during the traditional holidays, Seollal (Lunar New Year's Day, January 1 in the lunar calendar) and Chuseok (Korean Thanksgiving Day, August 15 in the lunar calendar), Koreans abruptly change their patterns of life.
11) These large scale behavioral change and emotional stress can affect cardiac mortality.
12) Some patients might inappropriately delay seeking necessary medical treatment until after the holidays.
8)13) In this study, we evaluated the difference between traditional holiday and other day types in the incidence and outcomes of OHCA. We also explored the potential mechanisms that may explain this difference.
METHODS
Study population
The Korea OHCA Registry (KOHCAR) is a nationwide, prospective observational registry of OHCA from 712 hospitals throughout South Korea. All OHCA events that occurred in Korea in contact with the emergency medical service (EMS) were included in KOHCAR. KOHCAR enrolled 96.50% of all OHCA individuals in South Korea. The full details of the KOHCAR aims and protocols have been published elsewhere.
14) The Korea Centers of Disease Control and Prevention (CDC) approved the use of all data. The data obtained from KOHCAR included the following: the date of OHCA, demographic information of the victims, place of OHCA, event witness, bystander cardiopulmonary resuscitation (CPR), etiology of OHCA, initial electrocardiography rhythm, experience of return of spontaneous circulation (ROSC) before emergency department (ED) visit, time from ED visit to ROSC, survival to discharge, and cerebral performance category (CPC) at time of discharge using the Utstein Style.
The present study population included a total of 139,741 OHCA events that occurred in patients ≥18 years old enrolled in KOHCAR with recorded ED visit date and time between January 1, 2012, and December 31, 2016. As shown in
Figure 1, we excluded patients with OHCA of noncardiac cause (e.g., trauma, intoxication, primary respiratory arrest, or other noncardiac medical causes, n=43,581), and we excluded patients with missing value of cause (n=94). The final study subjects for the present analysis consisted of 95,066 OHCA events of cardiac causes. The Institutional Review Boards of Sejong General Hospital (2018-0557) and Korean CDC (2018-28) approved this study protocol and granted waivers of the informed consent based on the general impracticability and minimal harm. Patients' information was anonymized and de-identified before being provided. The study was conducted in accordance with the Declaration of Helsinki and its relevant guidelines and regulations.
Figure 1
Study flowchart.
OHCA = out-of-hospital cardiac arrest; ROSC = return of spontaneous circulation.

Data definitions
The date of the OHCA was defined as the date the OHCA was witnessed. When the OHCA was not witnessed, we used last normal time as OHCA date, and if neither was confirmed, the ED visit time was used as the OHCA date.
We divided the days during the study periods by day type (weekday, weekend, public holiday, and traditional holiday). Traditional holidays were defined as Seollal (Lunar New Year's Day, January 1 in the lunar calendar) holiday and Chuseok (Korean Thanksgiving Day, August 15 in the lunar calendar) holiday (
Supplementary Table 1). A weekend linked with Seollal or Chuseok holiday was defined as traditional holiday. Public holiday was defined as
Supplementary Table 1. A weekend linked with public holiday was defined as public holiday. The weekend was defined as Saturday and Sunday that are not associated with a holiday. The weekday was defined as Monday through Friday, which is not associated with a holiday.
Outcomes
The difference by day type in the incidence of OHCA was evaluated. Among the patients who were admitted to the hospital after ROSC, we evaluated the day type variability in the in-hospital mortality. Among the patients who survived to hospital discharge, the day type variability in the poor neurologic outcomes (defined as CPC 3, 4, or 5) was also evaluated. A CPC score of 3 denotes severe cerebral disability, 4 coma or vegetative state, and 5 dead.
Statistical analysis
As shown in
Tables 1 and
2, descriptive statistics are summarized as mean with 95% confidence interval (CI) and median with interquartile ranges (IQRs) for the continuous variables. Moreover, categorical variables were summarized as counts with percentages. After we examined the OHCA incidence in the study population using Shapiro-Wilk normality test and Kolmogorov-Smirnov normality test, we confirmed that the data were not normal distribution of the residuals (p<0.001 and p<0.001). Because of this, the day type variability of OHCA incidence was shown graphically and was compared using the Kruskal-Wallis rank sum test. Additionally, we compared the two groups using the Welch two-sample t-test. Furthermore, since the traditional holiday happens in the autumn and winter, we confirmed the variability in OHCA incidence according to day type among the cohort of autumn and winter. Moreover, we evaluated the variability in OHCA incidence according to day type in each male and female.
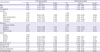
Table 1
Baseline characteristics

|
Predictor variables |
Weekday (1,243 days, n=63,688) |
Weekend (491 days, n=26,186) |
Public holiday (50 days, n=2,605) |
Traditional holiday (43 days, n=2,587) |
p value |
|
All |
51.2 |
53.3 |
52.1 |
60.2 |
|
|
Age (years) |
|
|
|
|
0.104 |
|
18–39 |
2.0 (3.9) |
2.1 (3.9) |
2.3 (4.5) |
2.3 (3.8) |
|
40–49 |
3.8 (7.5) |
4.2 (7.8) |
3.6 (6.9) |
4.0 (6.6) |
|
50–59 |
7.4 (14.5) |
8.1 (15.1) |
7.9 (15.2) |
8.1 (13.5) |
|
60–69 |
8.3 (16.3) |
8.5 (16.0) |
7.7 (14.9) |
9.8 (16.2) |
|
70–79 |
14.5 (28.2) |
14.6 (27.4) |
15.1 (29.0) |
18.1 (30.0) |
|
80–89 |
11.9 (23.2) |
12.4 (23.3) |
11.8 (22.7) |
13.2 (22.0) |
|
≥90 |
3.3 (6.5) |
3.5 (6.5) |
3.6 (6.9) |
4.7 (7.8) |
|
Mean (SD) |
69.67 (15.33) |
69.48 (15.51) |
69.62 (15.57) |
70.16 (15.28) |
|
Median (IQR) |
73 (59–81) |
73 (58–81) |
73 (58–81) |
73 (60–81) |
|
Sex |
|
|
|
|
0.550 |
|
Female |
19.2 (37.5) |
19.8 (37.2) |
20.0 (38.3) |
22.9 (38.0) |
|
Male |
32.0 (62.5) |
33.5 (62.8) |
32.1 (61.7) |
37.3 (62.0) |
|
Metropolis |
|
|
|
|
0.161 |
|
Metropolitan |
20.8 (40.6) |
21.3 (39.9) |
20.5 (39.3) |
23.7 (39.4) |
|
Nonmetropolitan |
30.5 (59.4) |
32.0 (60.1) |
31.6 (60.7) |
36.4 (60.6) |
|
Place of arrest |
|
|
|
|
<0.001 |
|
Home |
29.7 (57.9) |
30.6 (57.4) |
30.1 (57.7) |
37.0 (61.6) |
|
Other private places |
5.6 (11.0) |
6.0 (11.3) |
6.0 (11.6) |
5.5 (9.2) |
|
Public place |
6.7 (13.0) |
6.5 (12.2) |
6.0 (8.3) |
5.0 (8.3) |
|
Ambulance |
2.5 (4.8) |
2.6 (4.9) |
2.5 (4.7) |
3.3 (5.6) |
|
Others |
6.8 (13.2) |
7.6 (14.2) |
7.5 (14.4) |
9.2 (15.3) |
|
Time of arrest |
|
|
|
|
<0.001 |
|
Daytime (7 AM–3 PM) |
22.3 (43.5) |
22.8 (42.8) |
23.3 (44.8) |
26.8 (44.6) |
|
Evening (3 PM–11 PM) |
17.8 (34.8) |
19.4 (36.4) |
18.3 (35.1) |
20.9 (34.8) |
|
Night (11 PM–7 AM) |
11.1 (21.7) |
11.1 (20.8) |
10.5 (20.1) |
12.4 (20.6) |
|
Season of arrest |
|
|
|
|
<0.001 |
|
Spring (Mar–May) |
16,274/315 |
6,880/127 |
965/18 |
- |
|
51.7 (25.6) |
54.2 (26.3) |
53.6 (37.0) |
|
Summer (Jun–Aug) |
13,894/318 |
5,947/130 |
573/12 |
- |
|
43.7 (21.8) |
45.7 (22.7) |
47.8 (22.0) |
|
Autumn (Sep–Nov) |
15,599/306 |
6,233/118 |
431/9 |
1,137/22 |
|
51.0 (24.5) |
52.8 (23.8) |
47.9 (16.5) |
51.7 (44.0) |
|
Winter (Dec–Feb) |
17,921/304 |
7,126/116 |
636/11 |
1,450/21 |
|
59.0 (28.1) |
61.4 (27.2) |
57.8 (24.4) |
69.0 (56.0) |
|
Witnessed arrest |
22.6 (44.0) |
24.6 (46.1) |
24.3 (46.6) |
26.8 (44.5) |
<0.001 |
|
Type of bystander |
|
|
|
|
<0.001 |
|
Healthcare provider |
3.8 (7.5) |
3.8 (7.1) |
3.4 (6.6) |
4.3 (7.2) |
|
Family |
27.6 (53.8) |
29.2 (54.7) |
28.8 (55.2) |
35.0 (58.1) |
|
Colleague or friend |
5.8 (11.3) |
5.9 (11.0) |
5.7 (11.0) |
4.6 (7.7) |
|
Others |
13.1 (25.8) |
13.9 (26.1) |
13.1 (25.2) |
15.6 (25.8) |
|
Unknown |
0.9 (1.6) |
0.7 (1.2) |
1.0 (2.0) |
0.7 (1.2) |
|
Bystander CPR |
7.1 (13.9) |
7.9 (14.9) |
7.9 (15.2) |
8.5 (14.1) |
<0.001 |
|
Low flow time |
|
|
|
|
0.650 |
|
Mean (SD) |
48.53 (13.43) |
48.68 (13.41) |
48.73 (13.52) |
48.05 (13.80) |
|
Median (IQR) |
54 (39–60) |
54 (40–60) |
54 (41–60) |
54 (38–60) |
|
Primary ECG |
|
|
|
|
0.574 |
|
VF |
2.9 (5.7) |
3.1 (5.8) |
2.7 (5.3) |
3.4 (5.6) |
|
Pulseless VT |
0.4 (0.7) |
0.4 (0.7) |
0.5 (1.0) |
0.3 (0.5) |
|
PEA |
10.8 (21.0) |
11.1 (20.8) |
10.6 (19.8) |
12.7 (21.0) |
|
Asystole |
37.2 (72.6) |
38.8 (72.7) |
38.5 (73.9) |
43.8 (72.8) |
|
Prehospital ROSC |
2.7 (5.3) |
3.2 (6.0) |
2.7 (5.3) |
3.2 (5.3) |
<0.001 |
|
Cessation of in-hospital resuscitation within 20 minutes without ROSC |
25.7 (50.1) |
27.3 (51.2) |
26.4 (50.7) |
31.2 (51.8) |
0.009 |
|
Performed CAG |
1.5 (2.9) |
1.6 (3.0) |
1.2 (2.3) |
1.5 (2.6) |
0.100 |
|
ECMO |
0.4 (0.8) |
0.3 (0.5) |
0.3 (0.5) |
0.3 (0.6) |
0.014 |
|
TTM |
1.4 (2.7) |
1.4 (2.6) |
1.3 (2.4) |
1.5 (2.4) |
0.334 |
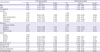
Table 2
Analysis of outcomes by day type

|
Outcomes |
Weekday (1,243 days, n=63,688) |
Weekend (491 days, n=26,186) |
Public holiday (50 days, n=2,605) |
Traditional holiday (43 days, n=2,587) |
p value |
|
All |
51.2 |
53.3 |
52.1 |
60.2 |
|
|
ROSC after initial resuscitation |
11.3 (22.1) |
11.5 (21.5) |
11.5 (22.0) |
13.1 (21.7) |
0.324 |
|
Admission to hospital |
8.7 (16.9) |
9.2 (17.2) |
9.0 (17.3) |
10.2 (17.0) |
0.656 |
|
Length of stay among patients admitted to the hospital (day) |
11.97 (21.32) |
11.84 (20.22) |
11.23 (17.56) |
10.85 (17.89) |
0.753 |
|
In-hospital mortality among patients admitted to the hospital |
5.6/8.7 (65.2) |
5.8/9.2 (63.6) |
6.1/9.0 (67.6) |
7.1/10.2 (69.7) |
0.021 |
|
Poor neurologic outcomes among hospital survivors |
1.3/3.0 (42.6) |
1.3/3.3 (39.5) |
1.5/2.9 (50.7) |
1.1/3.1 (35.3) |
0.008 |
Additionally, we evaluated the temporal variability of OHCA incidence. We evaluated the OHCA incidence during pre-holiday (3 days before, 2 days before, 1 day before), holiday (1st holiday, 2nd holiday, 3rd holiday, 4th holiday), and post-holiday (1 day after, 2 days after, 3 days after). Since the traditional holiday happens in the lunar calendar, we compared the OHCA incidence of traditional holiday with that of the same solar calendar date with traditional holiday during the study period. In this analysis, the same solar date of weekday, weekend, and public holiday was used. The results were shown graphically, and the differences of OHCA incidence between the traditional holiday and same solar date of other years were compared using the χ2 goodness-of-fit test. Furthermore, we confirmed the circadian variability in OHCA incidence and compared traditional holiday and weekday using the χ2 goodness-of-fit test.
Additionally, we confirmed the effect of the duration of traditional holidays by comparing OHCA incidence of traditional holidays to that of other nonworking days (public holiday and weekend). In this comparison, we used a 3-day weekend period with a public holiday on Monday or Friday. We determined the OHCA incidence on the 1st, 2nd, and 3rd days of the traditional holiday and other nonworking days and compared the differences using the χ2 goodness-of-fit test.
Logistic regression modeling was used to examine the association between the day type and in-hospital mortality after adjusting for the following variables: patients' age, sex, OHCA in metropolitan areas (population over 1,000,000 persons), place of OHCA (home, public place, ambulance, and others), season of OHCA, witness status (witnessed versus unwitnessed arrest), bystander CPR (performed or not), low flow time, first monitored cardiac rhythm (shockable versus non-shockable), and prehospital ROSC (ROSC before ED visit). Non-shockable first cardiac rhythm included asystole, pulseless electrical activity, and unknown non-shockable rhythm. Continuous covariates were tested for linearity, and nonlinear adjustment covariates were transformed with spline functions or truncated, as appropriate. Rate of missingness was <1% for all covariates; patients with any missing covariate (n=387, 0.4%) were excluded, and imputation was not performed. The analysis population for logistic regression modeling of in-hospital mortality was 16,172 patients who were admitted to the hospital after ROSC. Results are presented as hazard ratios (HRs) with 95% CIs.
Additionally, we used logistic modeling to confirm the association between the day type variability and poor neurologic outcomes. For this evaluation, we adjusted the same variables in the previous evaluation of in-hospital mortality. The analysis population for logistic regression modeling of poor neurologic outcome was 5,673 patients who survived to hospital discharge after OHCA events. Results are presented as HRs with 95% CIs. All analyses of this study were performed using the R software version 3.4.3 (R Development Core Team, Vienna, Austria). All p values <0.05 were considered as statistically significant.
RESULTS
Characteristics of the study population
Of the 95,066 OHCA events that comprised the present study population, the median (25th, 75th percentile) patient age was 73 (59, 81) years, 59,441 events (62.5%) occurred in male patients, 38,327 events (40.3%) occurred in the metropolis, 55,007 events (57.9%) occurred at home, 42,482 events (44.7%) were witnessed, bystander of 51,538 events (54.2%) were family, and bystander CPR was performed in 13,487 events (14.2%). The median (25th, 75th percentile) of low flow time (time from resuscitation start to end) was 54 (40, 60) minutes. In-hospital mortality was 64.9% among the 16,172 patients who were admitted to the hospital. Poor neurologic outcome was 41.8% among the 5,673 hospital survivors.
Table 1 shows the significant differences between day type in place of arrest, time of arrest, season of arrest, witnessed arrest, type of bystander, performed bystander CPR, prehospital ROSC, cessation of in-hospital resuscitation within 20 minutes without ROSC, and performed extracorporeal membrane oxygenation (ECMO). Moreover,
Table 2 shows the significant differences between day type in in-hospital mortality among patients admitted to the hospital and poor neurologic outcomes among hospital survivors. However, there was no significant difference between day types in ROSC after initial resuscitation, admission to hospital, and length of stay among patients admitted to the hospital.
OHCA incidence variability by day type
For study periods, there were 1,243 weekdays, 491 weekends, 50 public holidays, and 43 traditional holidays. As shown in
Figure 2A, the median OHCA incidences were 51.0 (IQR, 44.0–58.0), 53.0 (IQR, 46.0–60.5), 52.5 (IQR, 45.3–59.8), and 60.0 (IQR, 52.0–69.0) on weekday, weekend, public holiday, and traditional holiday, respectively, and there is a significant difference between day type groups using the Kruskal-Wallis rank sum test (p<0.001). The OHCA incidence of traditional holiday was significantly more likely to occur than that of weekday (p<0.001), weekend (p=0.001), and public holiday (p<0.001) using the Welch two-sample t-test.
Figure 2
OHCA incidence by day type.
OHCA = out-of-hospital cardiac arrest.

As shown in
Figure 2B, among the cohort of autumn and winter, the OHCA occurred more frequently on traditional holiday (60 [52, 69]) than on weekday (55 [48, 62], p=0.012) and public holiday (54.5 [47.5, 61], p=0.017). There is no significant difference between traditional holiday and weekend (57 [50, 63], p=0.14). Additionally, as shown in
Supplementary Figure 1, there was no significant difference in the OHCA incidence between male and female.
Temporal variability of OHCA incidence
As shown in
Figure 3A, we found an increase in the incidence of OHCA through holiday, and the highest incidence of OHCA occurred on the last day of the holiday. Furthermore, there was a significant difference between holidays and same solar date of other years (p<0.001). As shown in
Figure 3B, OHCA occurred more frequently during daytime and in the evening, with a large peak in occurrence from 7 to 10 AM and a smaller secondary peak from 5 to 7 PM. The OHCA incidence in the holiday was similar in weekday from 6 to 8 AM. However, at other times, OHCA occurred more frequently on traditional holiday than on weekday. There was a significant difference between traditional holiday and weekday (p<0.001).
Figure 3
Temporal variation of OHCA.
OHCA = out-of-hospital cardiac arrest.

We additionally compared the incidence of OHCA on traditional holiday and longer duration holiday (≥3 days) which consisted of weekend and public holiday on Monday or Friday, and found the incidence of traditional holiday OHCA was significantly higher than that of longer duration holiday (
Supplementary Figure 2, p<0.001).
Day type variability in OHCA outcomes
In-hospital mortality among admitted patients was highest for OHCA that occurred on traditional holiday (
Table 2). There was a significant difference in in-hospital mortality according to day types (p=0.021). After multivariable adjustment, compared with traditional holiday OHCAs, weekday OHCAs (adjusted HR, 0.747; 95% CI, 0.587–0.945; p=0.016) and weekend OHCAs (adjusted HR, 0.741; 95% CI, 0.579–0.943; p=0.016) but not public holiday OHCAs (adjusted HR, 0.810; 95% CI, 0.585–1.121; p=0.204) were associated with lower in-hospital mortality (
Table 3).
Table 3
Factors that are associated with in-hospital death among admitted OHCA patients
|
Characteristics |
Univariate analysis |
Multivariate analysis |
|
HR |
95% CI |
p value |
HR |
95% CI |
p value |
|
Age |
1.031 |
1.028–1.033 |
<0.001 |
1.020 |
1.018–1.023 |
<0.001 |
|
Male |
0.593 |
0.550–0.638 |
<0.001 |
0.773 |
0.710–0.842 |
<0.001 |
|
Metropolitan |
0.658 |
0.616–0.702 |
<0.001 |
0.641 |
0.595–0.691 |
<0.001 |
|
Location |
|
|
|
|
|
|
|
Others |
1.000 |
|
|
1.000 |
|
|
|
Home |
1.041 |
0.943–1.148 |
0.425 |
0.860 |
0.767–0.963 |
0.009 |
|
Other private places |
1.399 |
1.204–1.627 |
<0.001 |
0.850 |
0.716–1.010 |
0.064 |
|
Public place |
0.519 |
0.467–0.578 |
<0.001 |
0.607 |
0.537–0.686 |
<0.001 |
|
Ambulance |
0.709 |
0.624–0.805 |
<0.001 |
0.756 |
0.650–0.879 |
<0.001 |
|
Day type |
|
|
|
|
|
|
|
Traditional holiday |
1.000 |
|
|
1.000 |
|
|
|
Weekday |
0.813 |
0.659–0.998 |
0.051 |
0.747 |
0.587–0.945 |
0.016 |
|
Weekend |
0.759 |
0.612–0.936 |
0.011 |
0.741 |
0.579–0.943 |
0.016 |
|
Public holiday |
0.908 |
0.684–1.205 |
0.505 |
0.810 |
0.585–1.121 |
0.204 |
|
Season |
|
|
|
|
|
|
|
Spring |
1.000 |
|
|
1.000 |
|
|
|
Summer |
0.894 |
0.814–0.980 |
0.017 |
0.946 |
0.851–1.052 |
0.309 |
|
Autumn |
0.916 |
0.836–1.004 |
0.061 |
0.928 |
0.835–1.031 |
0.167 |
|
Winter |
0.958 |
0.875–1.049 |
0.353 |
0.870 |
0.784–0.966 |
0.009 |
|
Witnessed arrest |
0.463 |
0.429–0.500 |
<0.001 |
0.612 |
0.560–0.668 |
<0.001 |
|
Bystander CPR |
0.440 |
0.409–0.473 |
<0.001 |
0.700 |
0.643–0.762 |
<0.001 |
|
Low flow time |
1.028 |
1.024–1.032 |
<0.001 |
1.033 |
1.028–1.037 |
<0.001 |
|
Initial shockable ECG |
0.383 |
0.321–0.455 |
<0.001 |
0.286 |
0.236–0.346 |
<0.001 |
|
Prehospital ROSC |
0.159 |
0.147–0.171 |
<0.001 |
0.174 |
0.161–0.189 |
<0.001 |
Among the cohort of survivors to hospital discharge, there was a significant difference in poor neurologic outcomes between day types (p=0.008). As shown in
Table 2, the survivors of OHCA on traditional holiday had better neurologic outcomes than the other day types. After multivariable adjustment, compared with traditional holiday OHCAs, weekday OHCAs (adjusted HR, 1.989; 95% CI, 1.119–3.554; p=0.020) but not weekend OHCAs (adjusted HR, 1.395; 95% CI, 0.914–2.154; p=0.127) and public holiday OHCAs (adjusted HR, 1.349; 95% CI, 0.875–2.101; p=0.179) were associated with poor neurologic outcomes (
Supplementary Table 2). Among the 387 patients with any missing covariate for multivariable adjustment, the in-hospital mortality rate was 64.9% and the poor neurologic outcome rate was 38.5%. These results were similar to the other patients' in-hospital mortality rate (64.9%) and poor neurologic outcome rate (41.8%).
DISCUSSION
In this large, population-based, multisite study of 95,066 OHCA events, we confirmed that OHCA occurred more frequently on traditional holiday than on weekday, weekend, and public holiday. Additionally, traditional holiday was related with higher in-hospital mortality than weekdays and weekend, and with lower poor neurologic outcomes than weekdays.
We found a higher incidence of OHCA on traditional holidays than on other types of days. Furthermore, we found that the OHCA incidence increased during holiday. These results are similar to those of a previous study that reported increased OHCA incidence during the Christmas and New Year holiday season in the United States.
8) Decreased accessibility of the hospital during the holiday season might be a reason for the increased incidence of OHCA during holidays.
13)15) The duration of a traditional holiday is longer than that of weekend and public holidays, and this might be one of the reasons for the highest OHCA incidence during traditional holidays.
The OHCA incidence of Korean traditional holidays was also higher than that of other nonworking days with the same duration. Accordingly, the high OHCA incidence of traditional holidays may be not only due to the duration of the nonworking days but also due to the specific characteristics of traditional holidays. Previous studies have reported a higher incidence of OHCA on weekends and holiday.
5)8)9)16)17) Although the reasons remain speculative, changes in behavior around nonworking days, including alcohol intake, sleep/wake cycle, and physical activity, may partly explain this observation.
12)13)
Among the cohort of autumn and winter, OHCA significantly and frequently occurred on traditional holiday than on weekday and public holiday. Moreover, OHCAs more frequently occurred on traditional holiday than on the same solar date of other years. These results confirmed that the highest OHCA incidence occurred more frequently during traditional holiday due to not only seasonal effect but also the effect of traditional holiday. We also found that there is no significant difference in OHCA incidence trend between men and women.
In our study, there was a discrepancy between high in-hospital mortality outcome and low poor neurologic outcomes on traditional holiday. In other words, the traditional holiday had a low survival to discharge rate, but a favorable neurologic rate of traditional holiday is high. There was a clue that cessation of in-hospital resuscitation within 20 minutes without ROSC is significantly more frequent on traditional holiday than that in weekday. Additionally, interventions (e.g., coronary angiography, ECMO, targeted temperature management) are less performed on traditional holiday than that in weekday. In big data analysis, we cannot define the definite causality between clinical outcomes and traditional holidays because we could not review the medical records of each case. Despite these limitations, our interpretation is that, due to the lack of medical resources on traditional holidays compared to that on weekdays, OHCA patients who were expected to have poor neurologic outcome might not require attempted aggressive resuscitation and interventions on traditional holidays. Therefore, poor neurologic prognosis patients might die on traditional holidays, and survival-to-discharge rate might be low on traditional holidays than that on weekdays. As poor outcome patients may have already died, the proportion of patients with poor prognosis may be reduced on traditional holidays. Because of this reason, the favorable neurologic outcomes may increase on traditional holidays than that on weekdays.
The findings of the present study have important implications from the perspective of preventive strategies and policy for OHCA care in South Korea. Efforts are required to reduce OHCA incidence during a holiday by studying the characteristics of the traditional holiday and developing strategies of public health and EMS, such as providing sufficient medical resources during traditional holidays. The traditional holiday OHCA occurred more often at home rather than in public place, and lesser bystander CPR was performed. Efforts are needed to reduce in-hospital mortality variability by increasing basic life support of family. Furthermore, the strategies are needed to recognize early and enhance bystander CPR of OHCA patients at home on traditional holiday.
There are several limitations in the present study. First, we used the registry-based observational data; therefore, this study was subjected to unmeasured confounding factors and biases. Additionally, we were not able to account other variables of resuscitation (e.g., quality of chest compression, dose of medication, and hands-off time) and the type of treating hospital (e.g., academic or community). Second, because we used the last normal time or the ED visit time as the OHCA time in the case of unwitnessed OHCAs, actual time of cardiac arrest can be inaccurate and thus has the potential for misclassification bias. Third, it is necessary to confirm the result of the present study in the global OHCA population, because the KOHCAR only consisted of South Korean patients.






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download