This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Few studies have reported non-acute long-term morbidity rates in children with intestinal malrotation. The aim of this study was to investigate the rate of constipation in children undergoing Ladd's procedure for isolated intestinal malrotation.
Methods
This retrospective study included children aged <15 years who underwent Ladd’s procedure for intestinal malrotation between 2001 and 2016. Demographics, presence of volvulus perioperatively, need for bowel resection, short term (<30 days) and long-term complications, including mortality were recorded. Constipation was defined as treatment with laxatives at 1-year follow-up.
Results
Of the 43 children included in the study, 49% were boys. The median age at surgery was 28 days (0–5, 293 days). Volvulus occurred in 26 children (60.5%), and bowel resection was required in 4 children (9.3%). Short-term complications categorized as grades II–V according to the Clavien-Dindo classification occurred in 13 children (30.2%). Of these, 5 children (11.6%) required re-operation. Constipation was observed in 9 children (23.7%) at the 1-year follow-up. No difference was observed in the rate of perioperative volvulus between children with and without constipation (44% vs. 65%, p=0.45). Excluding re-operations performed within 30 days after surgery, 3 children (6%) underwent surgery for intestinal obstruction during the study period.
Conclusion
Many children undergoing Ladd's procedure require bowel management even at long-term follow-up, probably secondary to constipation. It is important to thoroughly evaluate bowel function at the time of follow-up to verify or exclude constipation, and if treatment of constipation is unsuccessful, these children require evaluation for dysmotility disorders and/or intestinal neuronal dysplasia.
Keywords: Intestinal malrotation, Outcome, Bowel management
INTRODUCTION
Intestinal malrotation is a relatively common congenital malformation, although the exact incidence remains unknown. However, symptomatic malrotation occurs only in approximately 1/6,000 children [
1]. Several reports have highlighted the high postoperative surgical morbidity associated with this condition, including small bowel obstruction and revolvulus; however, limited information is available regarding persistent non-acute symptoms. Previous studies suggest that many children show persistent symptoms even after correction of malrotation and that this may be associated with an inherent dysmotility disorder, often causing non-mechanical bowel obstruction symptoms [
234]. The aim of this study was to investigate the need for any kind of bowel management at long-term 1-year follow-up following surgery for isolated intestinal malrotation.
MATERIALS AND METHODS
This study was approved by the Regional Ethics Board of the Lund University, Lund, Sweden (DNR. 2010/49).
Settings and children
This study was performed at a tertiary pediatric surgery center that caters to approximately 1.8 million individuals. Children <15 years of age who underwent Ladd's procedure for isolated intestinal malrotation between 2001 through 2016 were included in the study. This center usually performs only an open Ladd's procedure. Children with a concomitant gastrointestinal malformation that was identified perioperatively, or children with malrotation as a component of gastroschisis, omphalocele, or congenital occult contralateral hernia were excluded from the study.
Study design
This retrospective study included children aged <15 years. We only included children with isolated intestinal malrotation defined by the International Classification of Diseases, 10th Revision codes Q43.3 and K56.2. Demographic parameters, other concomitant congenital malformations and syndromes, history of premature birth (gestational age <37 weeks), age at surgery, presence of volvulus perioperatively, need for bowel resection, and short-term (<30 days) and long-term complications, including mortality, were recorded. Short-term complications included infections confirmed by a positive culture result, wound rupture, intestinal obstruction, anastomotic insufficiency, other complications requiring re-operation, and mortality and were graded according to the Clavien-Dindo classification [
5]. Grade I complications were excluded because a retrospective chart review would be an inaccurate method of obtaining reliable data. Long-term complications included the need for any kind of bowel management (administration of laxatives, enema, and/or medications) at 1-year follow-up, short bowel syndrome, intestinal obstruction, and mortality.
Statistical analyses
Data was analyzed using the IBM SPSS software ver. 24 (SPSS Inc., Chicago, IL, USA). Categorical data were analyzed using Fisher's exact test (between 2 groups) or chi-square test (among more than 2 groups). Significance was set to a p-value of <0.05.
RESULTS
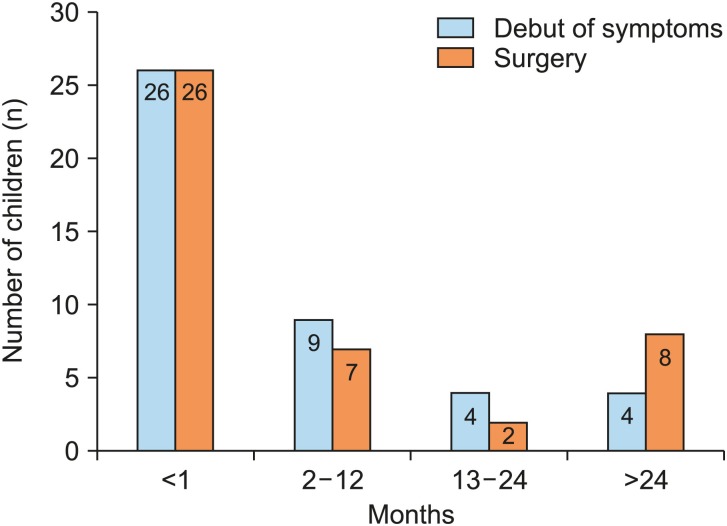
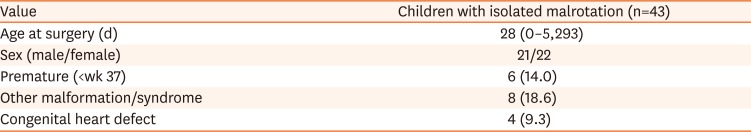
During the study period, 49 children underwent Ladd's procedure for intestinal malrotation, and of these, 6 underwent an operation for a concomitant intestinal malformation; therefore, only 43 children (21 boys and 22 girls) were included. The median age at surgery was 28 days (0–5, 293 days), and 34 children (79.1%) underwent the operation before the age of 1 year (
Fig. 1). Other congenital malformations or syndromes were observed in 8 children (18.6%), and 4 children (9.3%) had a congenital heart defect (
Table 1).
Fig. 1
Age at symptom onset and surgery in 43 children who underwent Ladd's procedure for isolated intestinal malrotation.
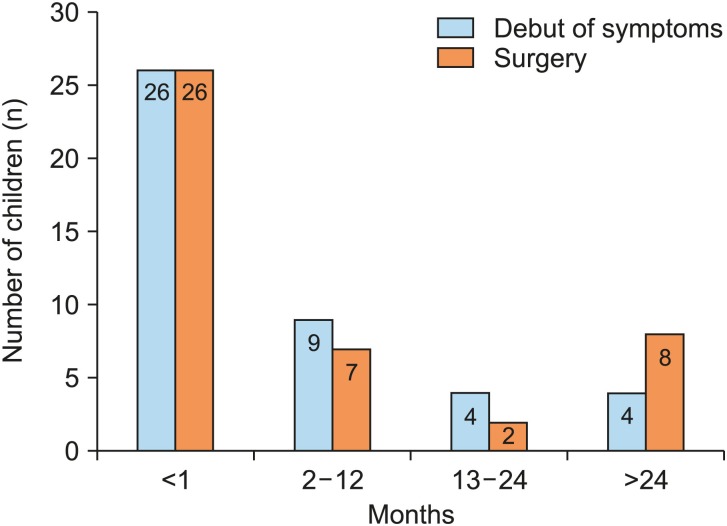
Table 1
Demographics and other malformations in children operated on for intestinal malrotation
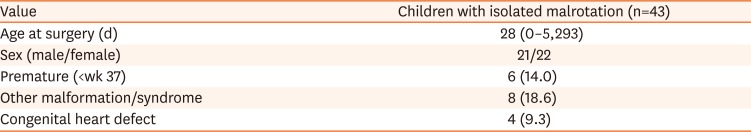
|
Value |
Children with isolated malrotation (n=43) |
|
Age at surgery (d) |
28 (0–5,293) |
|
Sex (male/female) |
21/22 |
|
Premature (<wk 37) |
6 (14.0) |
|
Other malformation/syndrome |
8 (18.6) |
|
Congenital heart defect |
4 (9.3) |
Urgent laparotomy was performed in 26 children (60.5%), subacute surgery (<72 hours) in 9 children (20.9%), and elective surgery for intestinal malrotation in 8 children (18.6%). Volvulus occurred in 26 children (60.5%) without any difference in incidence rates between children undergoing urgent, subacute, or elective surgery (p=0.26). Bowel resection was required in 4 children (9.3%). Histopathological examination of the resected bowel specimen revealed transmural necrosis; therefore, it was impossible to determine the presence of intestinal neuronal dysplasia.
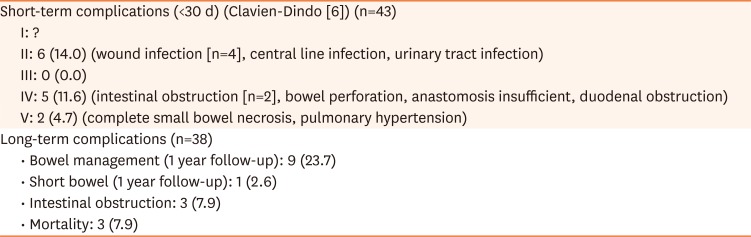
With regard to short-term complications, 13 children (30.2%) showed complications categorized as grades II–V according to the Clavien-Dindo classification. Of these, 5 children (11.6%) required re-operation and 2 died of complete small bowel necrosis and pulmonary hypertension (
Table 2) [
6]. At the 1-year follow-up, data regarding current bowel management were available in only 38 children. Nine children (23.7%) were treated with laxatives and 2 (5.3%) were treated with the intermittent use of enemas. No patient received any other medications for bowel management, and no patient received a specific diet. Constipation was treated by pediatricians (n=7) or pediatric surgeons (n=2). Seven of the 9 children with constipation underwent an operation at the age of <3 months and were, therefore, aged approximately 1 year at the time of follow-up. No child who underwent bowel management required re-operation after the initial Ladd's procedure. No difference was observed in the rates of perioperative volvulus between children who required bowel management (44%) and those who did not require bowel management (65%) (
p=0.45). No child in the study group complained of abdominal pain at the 1-year follow-up, and treatment with laxatives led to the successful resolution of symptoms in all children. Excluding re-operations performed within 30 days after surgery, 3 children (6%) underwent surgery for intestinal obstruction during the study period. At the long-term follow-up, 3 more children died (all 3 deaths were secondary to other underlying diseases).
Table 2
Short- and long-term postoperative complications in children operated on for isolated intestinal malrotation
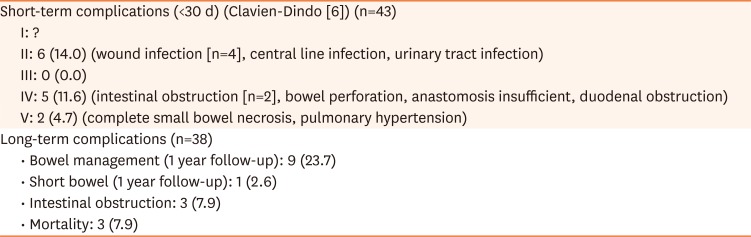
|
Short-term complications (<30 d) (Clavien-Dindo [6]) (n=43) |
|
I: ? |
|
II: 6 (14.0) (wound infection [n=4], central line infection, urinary tract infection) |
|
III: 0 (0.0) |
|
IV: 5 (11.6) (intestinal obstruction [n=2], bowel perforation, anastomosis insufficient, duodenal obstruction) |
|
V: 2 (4.7) (complete small bowel necrosis, pulmonary hypertension) |
|
Long-term complications (n=38) |
|
• Bowel management (1 year follow-up): 9 (23.7) |
|
• Short bowel (1 year follow-up): 1 (2.6) |
|
• Intestinal obstruction: 3 (7.9) |
|
• Mortality: 3 (7.9) |
DISCUSSION
We observed that nearly 25% of the children included in this small-sized, retrospective single-center study had received some kind of bowel management at the time of long-term follow-up after undergoing surgery for isolated intestinal malrotation. The rate of perioperative volvulus did not appear to affect the need for bowel management at the time of follow-up.
To our knowledge, no study has specifically investigated the need for bowel management at the long-term follow-up after isolated intestinal malrotation, although 3 previous studies have reported the rates of constipation after surgery for intestinal malrotation [
478] of 2–31%. However, the study with the highest constipation rate included adults [
8], whereas that with the lowest rate did not report the specific time interval for follow-up [
7]. In healthy children, the rate of constipation shows a wide range (5–22%), with most studies including children aged ≥4 years [
910111213]. A previous study that specifically focused on non-mechanical obstructive (dysmotility) symptoms in healthy children reported a rate of 14% associated with obstructive symptoms (difficulty with evacuation of soft stools) [
13]. The present study only investigated the rate of bowel management, which indirectly indicates the constipation rate and could also indicate the occurrence of non-mechanical obstructive bowel symptoms in these children. Although all children were successfully treated with laxatives, the rate of laxative use (24%) (as a component of bowel management) observed in the present study indicates impaired bowel function in a significant percentage of children undergoing Ladd's procedure. This is particularly true considering that our study only included children with isolated intestinal malrotation and that a significant percentage of children who required bowel management were 1-year-old. No patient in our study showed long-term postoperative abdominal pain, in contrast to the findings of previous studies [
8]. Thus, constipation and/or non-mechanical obstructive (dysmotility) symptoms may contribute to pain after Ladd's procedure. Impaired bowel function after surgery for intestinal malrotation could be attributed to the following factors (among several others): intestinal adhesions after laparotomy could manifest as constipation, and as previously described [
23], an intrinsic motility disturbance, or intestinal neuronal dysplasia (which may coexist with malrotation) [
14], could cause this complication. This latter condition was not suspected in our cohort, we could not confirm this finding based on the histopathological examination of resected bowel specimens.
Previous studies have reported that the rate of adhesive small bowel obstruction after Ladd's procedure was 6–24%, with varying duration of follow-up [
46151617]. Our results showed a rate of 8%, which is low compared to that reported in previous studies. No child in our study developed recurrent midgut volvulus; however, previous studies have reported rates of 0.5–7% [
417].
The limitations of this study include its retrospective design and the small sample size. The conditions necessitating bowel management could not be confirmed owing to the retrospective nature of the study. Therefore, we could not differentiate between non-mechanical (dysmotility) obstructive symptoms and constipation. However, all children were successfully treated with laxatives and/or enema, indicating that symptoms in all children could be attributed to constipation and not to dysmotility disorders.
In conclusion, many children undergoing Ladd's procedure for isolated intestinal malrotation require bowel management even at the long-term follow-up, probably secondary to a high constipation rate. It is important to completely evaluate the bowel function at follow-up to verify or exclude constipation, and if treatment with laxatives is unsuccessful, these children require evaluation for dysmotility disorders and/or intestinal neuronal dysplasia.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download