This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Safety pin ingestion is common in some regions of the world and may lead to severe morbidity and mortality. The aim of this study was to present some practical suggestions for ingested safety pins using an accompanying algorithm, presented for the first time in the literature to the best of our knowledge.
Methods
Twenty children with ingested safety pins during a 4-year period were retrospectively included in the study.
Results
Median age of patients was 9.5 months (interquartile range, 6.3–14 months), and 70% were girls. On endoscopic examination, safety pins were observed in the stomach (25%), duodenal bulb (20%), upper esophagus (15%), middle esophagus (10%), and second part of the duodenum (10%) but were not observed in 20% of the cases. Safety pins were removed using endoscopy in 15 cases (75%). In four cases (20%), no safety pin was observed on endoscopic examination. In one case (5%) involving a 6-month-old infant, the safety pin could not be removed although it was observed using endoscopy. No surgical intervention was needed for any patient. No complications such as perforation or deaths developed, except for erosions, due to the foreign body removal procedure.
Conclusion
Safety pins are easily removed endoscopically. The best option is to remove the safety pin using endoscopy while it is still in the esophagus and stomach. For this reason, endoscopic procedures should be performed as soon as possible in children who have ingested safety pins.
Keywords: Safety pin, Endoscopic, Foreign body, Algorithms
INTRODUCTION
Foreign body ingestion in children is a common public health problem worldwide. In the United States of America, foreign body ingestions cause approximately 1,500 deaths per year [
1]. Of the 23,087 cases of foreign body ingestion reported by the American Association of Poison Control Centers in 2015, 64% involve children aged ≤5 years [
2]. Although >80% of the gastrointestinal foreign bodies can be spontaneously excreted, some lead to severe morbidity and mortality [
3].
Safety pin ingestion has been reported in 1% of children with foreign body ingestions, but it is more common in some regions of the world [
4]. In our country, ingested safety pins constitute 7.8–38.6% of all ingested foreign bodies in children [
56]. The high frequency of safety pin ingestion is somehow our country's cultural phenomenon. Safety pins are mostly used to attach blue beads and other amulets believed to protect the baby against the evil eye or to attach gold jewellery gifts. Babies may usually pull and open these attachments and then swallow the open safety pin.
In the present study, children who had ingested safety pins and underwent endoscopic procedures were evaluated. The aim was to present some practical approaches for ingested safety pins. An algorithmic proposal of endoscopic removal for ingested safety pins was presented for the first time in the literature to the best of our knowledge.
MATERIALS AND METHODS
Patients
Data of 120 children who underwent flexible endoscopic intervention because of ingested foreign bodies during a 4-year period were collected retrospectively. Twenty of them who had ingested safety pins were included. Informed consent was obtained from the parents of all children prior to endoscopy. Principles outlined in the Declaration of Helsinki were followed.
Endoscopic procedure
All patients underwent neck, chest, and/or abdominal radiographies to detect the localization of the foreign body. The nil per os (NPO) status for 6–8 hours was provided prior to the procedure. Sedation was ensured with intravenous midazolam and propofol. Safety was ensured by endotracheal intubation.
Esophagogastroduodenoscopic procedures were performed using 5.9- and 9.4-mm-diameter flexible gastroscopes (Fujinon, 2500, Tokyo, Japan), and the foreign body was removed using rat tooth and alligator jaw grasping forceps. Immediately after the foreign body was removed, re-evaluation of the gastrointestinal mucosa in terms of complications was performed using endoscopy. Ingested safety pins that could not be removed or observed using endoscopy were followed up with radiography until spontaneous clearance was achieved.
RESULTS
The median age of patients was 9.5 months (interquartile range, 6.3–14 months), and 70% were girls.
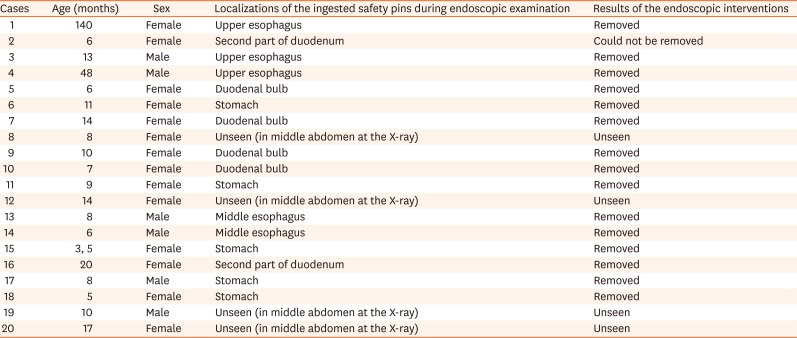
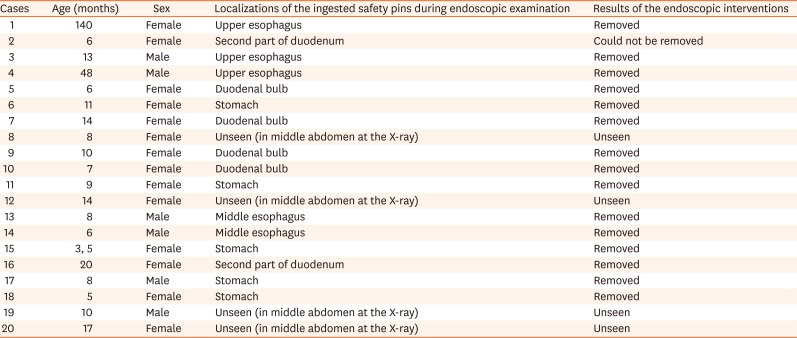
Table 1 presents details regarding age, sex, localizations of the ingested safety pins during endoscopy, and results of the endoscopic interventions. All patients were admitted to the hospital with foreign body ingestion complaints. All foreign body ingestions were accidental. All patients ingested the safety pins themselves, and the reason why the parents brought the infants to the hospital was that the safety pins were lost. All suspicions were verified on X-ray images.
Table 1
The features of the cases with ingested safety pins
|
Cases |
Age (months) |
Sex |
Localizations of the ingested safety pins during endoscopic examination |
Results of the endoscopic interventions |
|
1 |
140 |
Female |
Upper esophagus |
Removed |
|
2 |
6 |
Female |
Second part of duodenum |
Could not be removed |
|
3 |
13 |
Male |
Upper esophagus |
Removed |
|
4 |
48 |
Male |
Upper esophagus |
Removed |
|
5 |
6 |
Female |
Duodenal bulb |
Removed |
|
6 |
11 |
Female |
Stomach |
Removed |
|
7 |
14 |
Female |
Duodenal bulb |
Removed |
|
8 |
8 |
Female |
Unseen (in middle abdomen at the X-ray) |
Unseen |
|
9 |
10 |
Female |
Duodenal bulb |
Removed |
|
10 |
7 |
Female |
Duodenal bulb |
Removed |
|
11 |
9 |
Female |
Stomach |
Removed |
|
12 |
14 |
Female |
Unseen (in middle abdomen at the X-ray) |
Unseen |
|
13 |
8 |
Male |
Middle esophagus |
Removed |
|
14 |
6 |
Male |
Middle esophagus |
Removed |
|
15 |
3, 5 |
Female |
Stomach |
Removed |
|
16 |
20 |
Female |
Second part of duodenum |
Removed |
|
17 |
8 |
Male |
Stomach |
Removed |
|
18 |
5 |
Female |
Stomach |
Removed |
|
19 |
10 |
Male |
Unseen (in middle abdomen at the X-ray) |
Unseen |
|
20 |
17 |
Female |
Unseen (in middle abdomen at the X-ray) |
Unseen |
Endoscopic procedure results
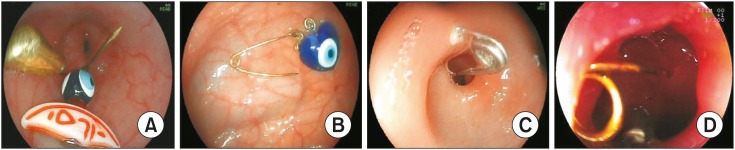
Localizations of safety pins when first observed during endoscopy are presented in
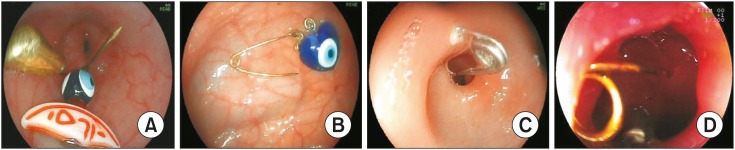
Table 1. Examples of endoscopic images of ingested safety pins are shown in
Fig. 1. On endoscopic examination, safety pins were observed in the stomach (25%), duodenal bulb (20%), upper esophagus (15%), middle esophagus (10%), and second part of the duodenum (10%), but these were not observed in 20% of the cases.
Fig. 1
Examples of endoscopic images of ingested safety pins. (A) A safety pin with an attached blue bead and amulet in the esophagus. (B) A blue bead separated from a safety pin in the stomach. (C) A safety pin with its pin part penetrated totally in the antral mucosa and head part that had entered the duodenal bulb through the pylorus. (D) A safety pin that had penetrated the mucosa of the duodenal bulb.
Safety pins were removed using endoscopy in 15 cases (75%). In four cases (20%), no safety pin was observed on endoscopic examination. In one case (5%) involving a 6-month-old infant, the safety pin could not be removed although it was observed using endoscopy. The safety pin was in the duodenum, with its body part localized distally; therefore, it could not be held from its body part, and the procedure was terminated. Spontaneous clearance was achieved 2 days later. Thus, all cases wherein safety pins were not observed or removed using endoscopy involved spontaneous clearance.
No surgical intervention was needed for any patient. No complications such as perforations or deaths developed, except for erosions, due to the foreign body removal procedure.
DISCUSSION
Eighteen of the 20 cases of safety pin ingestion involved patients aged <2 years, and the youngest patient was 3.5 months old. The largest safety pin removed in our case series was approximately 6-cm long. The North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) suggests the removal of sharp foreign bodies (i) immediately if they are in the esophagus, (ii) immediately if they are in the stomach and intestines and are symptomatic, (iii) within 24 hours if they are in the stomach and intestines and are asymptomatic via endoscopy first, and (iv) by surgical intervention if endoscopy is not successful and no spontaneous clearance is achieved 3 days after ingestion [
7]. The European Society of Gastrointestinal Endoscopy (ESGE) and European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) recommend that if sharp-pointed objects are located in the esophagus, stomach, or proximal duodenum, the removal procedure must be performed within <2 hours, even in asymptomatic children [
8]. As suggested by the NASPGHAN and ESGE/ESPGHAN, safety pins, as well as other sharp-pointed objects, should be removed as soon as possible.
Sarihan et al. [
9] reported that they performed right esophagoscopy in 15 children who had ingested safety pins; nine safety pins were removed, five passed out with spontaneous clearance, and one open safety pin lodged at the duodenum required laparotomy. Kalayci et al. [
10] reported seven cases of ingested open safety pins. They reported that all safety pins, including four lodged in the esophagus, two in the stomach, and one in the duodenum, were successfully removed.
In a series of 49 cases reported by pediatric surgeons [
11], 5 of the 18 safety pins in the esophagus could not be removed using endoscopy; eighteen safety pins in the stomach were left for spontaneous passage, and 7 of these 18 safety pins required surgical intervention; five safety pins below the stomach were spontaneously excreted; and surgical intervention was required for 7 safety pins in the intestines and the last one in the colon. Both in the present study and in other studies, safety pins passing through the duodenum could be excreted spontaneously. However, Gün et al. [
11] reported that they had operated on a patient with a safety pin in the colon. In the present study, all cases wherein safety pins were not observed or removed using endoscopy involved spontaneous clearance.
Rupture of the carotid artery [
12], hemopericardium and cardiac tamponade [
13], duodenocolic fistulas [
14], and incarcerated umbilical hernia [
15] have also been reported as serious complications. For this reason, endoscopic removal of an ingested safety pin should be immediately arranged following an NPO status. In the current case series, safety pins in the esophagus and stomach were removed easily, while in one case, wherein the safety pin was lodged in the second part of the duodenum, it could not be removed easily. Thus, the best option is to remove the safety pin using endoscopy while it is still in the esophagus and stomach.
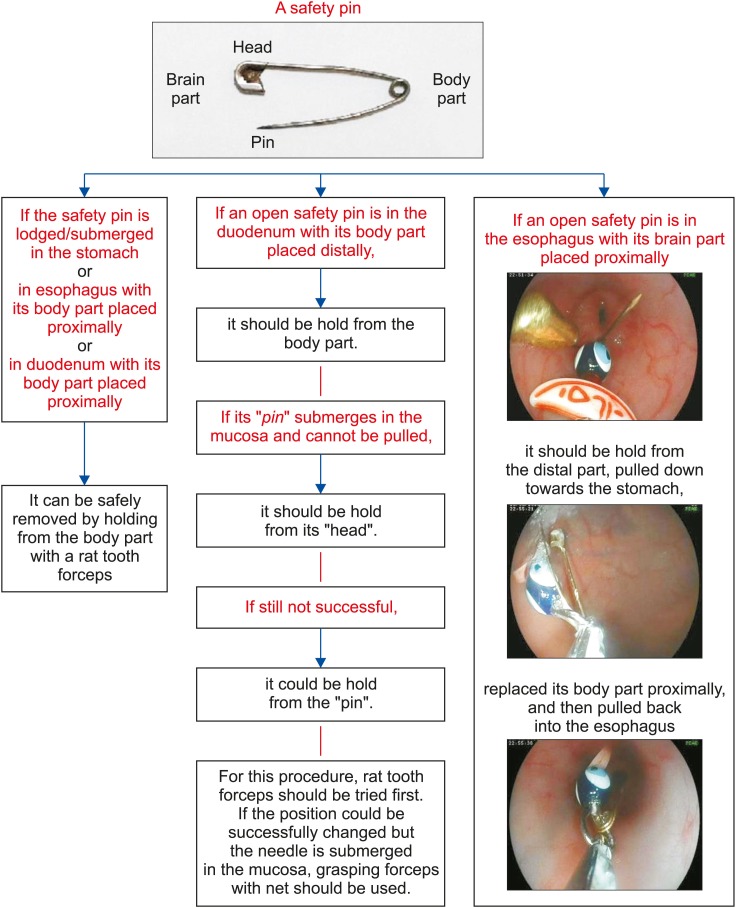
An algorithmic proposal for the technique of endoscopic removal for ingested safety pins is presented in
Fig. 2. This algorithm presents some suggestions on how to remove safety pins with different localizations.
Fig. 2
An algorithmic proposal for the technique of endoscopic removal for ingested safety pins.
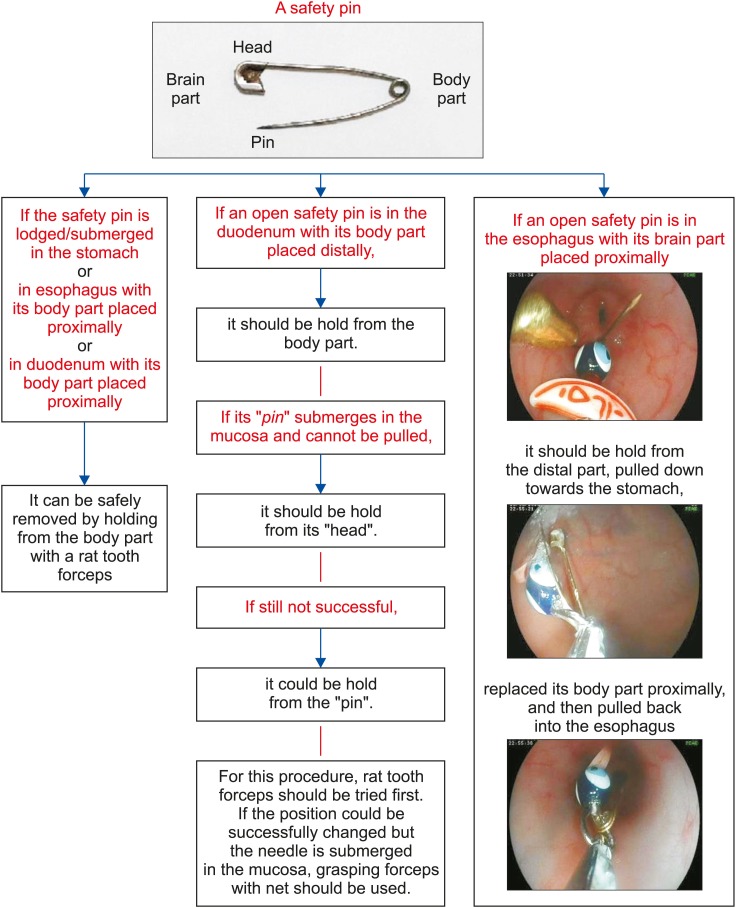
In conclusion, safety pins are easily removed endoscopically. For this reason, endoscopic procedures should be performed as soon as possible in children who have ingested safety pins. To the best of our knowledge, an algorithmic proposal of endoscopic removal for ingested safety pins has not been presented in the literature. A limitation of the study is that this was a single-center study. Therefore, there is a need for multicenter studies to evaluate these presented proposals.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download