RESULTS
KSPGHAN has 400 registered pediatricians online, among which 80 are PG and 320 are GP. Among the 400 pediatricians, 141 pediatricians (35.3%) responded to the survey. Among 141 pediatricians, 55 (68.8%) of the 80 PG and 86 (26.9%) of the 320 GP responded to the survey.
Fig. 1 shows the domestic area where the pediatricians who responded to the questionnaire were located.
Fig. 1
The geographical areas from which the pediatricians responded.

Among the 141 pediatricians who answered the survey, 39.0% (n=55) were PG and 72.7% of these PG (n=40) worked at a tertiary hospital. Approximately 60% of GP (n=52) worked at a primary hospital (
p<0.05). We observed that 94.6% of PG (n=52) and 46.5% of GP (n=40) worked at hospitals where hospitalization facilities were available (
p<0.05). The duration of working as pediatricians was similar in both groups (
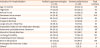
Table 1). Most pediatricians had been working in this specialty for over 10 years.
Table 1
Respondents specialty and duration as pediatrician

|
Duration of working |
Pediatric gastroenterologist (n=55) |
General pediatrician (n=86) |
|
<1 y |
0 (0.0) |
3 (3.5) |
|
1–4 y |
1 (1.8) |
8 (9.3) |
|
5–9 y |
12 (21.8) |
22 (25.6) |
|
>10 y |
42 (76.4) |
53 (61.6) |
|
Total |
55 (39.0) |
86 (61.0) |
The PG and GP groups did not differ with respect to assessment of the symptoms and signs of AGE (p>0.05). Both PG and GP considered diarrhea (n=119) or vomiting (n=107) to be the primary symptom of AGE. A few pediatricians diagnosed AGE in children without vomiting and diarrhea.
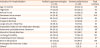
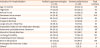
The most common indication for hospitalization was severe dehydration (n=139, 98.8%), followed by persistent vomiting and lethargy/irritability (
Table 2). Nearly all pediatricians treated moderate-to-severe dehydration with IV fluids (PG n=54, 98.2%; GP n=74, 92.9%). ORT therapy or no hydration was used in children with mild dehydration by both PG and GP.
Table 2
Symptoms diagnosed as acute gastroenteritis
|
Indication for hospitalization |
Pediatric gastroenterologist (n=55) |
General pediatricians (n=86) |
Total numbers |
|
Age <2 months |
31 (38.0) |
38 (44.2) |
69 |
|
High fever |
17 (30.9) |
26 (30.2) |
43 |
|
Refusal to eat |
34 (61.8) |
54 (62.8) |
88 |
|
Decreased urine output |
41 (74.6) |
68 (79.1) |
109 |
|
Frequent vomiting |
30 (54.5) |
54 (62.8) |
84 |
|
Frequent diarrhea |
5 (9.1) |
16 (18.6) |
21 |
|
Large amount of diarrhea |
10 (18.2) |
15 (17.4) |
25 |
|
Impossible intake of oral rehydration therapy |
53 (96.4) |
83 (96.5) |
136 |
|
Abdominal pain/abdominal distention |
34 (61.8) |
34 (39.5) |
68*
|
|
Mucoid or bloody diarrhea |
32 (58.2) |
50 (58.1) |
82 |
|
Lethargy/irritability |
50 (90.9) |
73 (84.9) |
123 |
|
Underlying chronic disease |
31 (56.4) |
30 (34.9) |
61*
|
|
Severe dehydration |
55 (100.0) |
84 (97.7) |
139 |
|
Prolonged diarrhea over 3 days |
1 (1.8) |
8 (9.3) |
9 |
|
Others†
|
5 (9.1) |
2 (2.3) |
0 |
Antiemetics were prescribed for >50% of the children with AGE by 87.3% (n=48) of PG and 96.6% (n=85) of GP (p>0.05). Domperidone was the most common drug used to treat vomiting by 57.4% (n=31) of PG and 57.1% (n=51) of GP. Ondansetron was more commonly prescribed by PG (n=12, 22.2%) than by GP (n=6, 7.0%). Trimebutine was more commonly prescribed by GP (n=62, 73.3%) than by PG (n=28, 27.3%) (p<0.05).
Antacids were prescribed in children with abdominal pain and vomiting by 5.6% (n=3) of PG and 8.1% (n=7) of GP. Proton-pump inhibitors were prescribed for abdominal pain and vomiting by 7.3% (n=4) of PG and 4.6% (n=4) of GP.
Probiotics were the most common antidiarrheal agents prescribed by 89.1% (n=49) of PG and 100% (n=86) of GP (p<0.05). Saccharomyces boulardii and Lactobacillus rhamnosus GG were the most common probiotics prescribed for diarrhea by PG (n=48, 87.8% and n=35, 63.6%, respectively) and GP (n=69, 80.2% and n=40, 46.5%, respectively). Other commercially available probiotics prescribed by GP included Medilac DSⓇ (Hammi, Seoul, Korea), Bacilpedi powderⓇ (Sama Pharm Co., Ltd., Wonju, Korea), LacterolⓇ (Dong-Wha Pharm Co., Ltd., Seoul, Korea), AntibioⓇ (Han Wha Pharma Co., Ltd., Seoul, Korea). Smectite was more commonly prescribed by GP (n=47, 64.4%) than by PG (n=8, 14.6%) (p<0.05). Racecadotril was prescribed by 27.3% (n=15) of PG and 19.6% (n=16) of PG. Loperamide was prescribed by 5.5% (n=3) of PG and 18.4% (n=16) of GP (p<0.05). Zinc was prescribed by 31.5% (n=17) of PG and 23.5% (n=19) of GP.
With respect to the frequency of having prescribed antibiotics to children with AGE during the month preceding presentation, 22.2% (n=12) of PG and 12.8% (n=11) of GP confirmed prescribing these drugs. Most PG (n=42, 77.8%) and GP (n=74, 87.2%) revealed that they did not prescribe antibiotics to treat AGE. The most common indication for antibiotic prescriptions was blood in diarrheal stool [73.5% (n=36) of PG, 76.3% (n=57) of GP], followed by high fever [51.0% (n=28) of PG, 63.2% (n=54) of PG]. Antibiotics were prescribed in children with abdominal tenderness by 41.8% (n=23) of PG and 24.4% (n=21) of GP (p<0.05).
Dietary changes were more commonly recommended by GP (n=51, 59.3%) than by PG (n=15, 27.3%) (p<0.05, 95% confidence interval). We observed that 80.0% (n=44) of PG and 66.7% (n=57) of GP did not recommend a nil per os (NPO) status in the child. NPO was recommended (based on the case) by 20.0% (n=11) of PG and 27.9% (n=24) of GP (p>0.05).
With respect to recommendations for the resumption of feeding with milk or fruits, 43.6% (n=24) of PG and 63.9% (n=55) of GP advised an antidiarrheal diet such as lactose-free milk. GP were more likely to recommend the consumption of pectin-containing fruits such as bananas or persimmons (n=36, 41.9%) and the restriction of milk-containing foods (n=49, 56.9%) and fruits in quantity. Restriction of milk and consumption of pectin-containing fruits was recommended by 16.4% (n=9) and 12.7% (n=7) of PG, respectively (p<0.05).
With respect to the duration required for the improvement of AGE, 52.9% (n=74) of the pediatricians surveyed answered that the duration was within 3 days. All GP answered that AGE improved symptomatically within 7 days.
Diagnostic workup to evaluate the etiological agents associated with AGE was performed by 83.6% (n=46) of PG and 88.4% (n=76) of GP when the child was hospitalized. Assessment of the virus in the stool using polymerase chain reaction and stool cultures was more commonly performed by PG than by GP. Both PG and GP showed similar rates of the performance of the rotavirus antigen test (9.1%, n=5 vs. 4.7%, n=4, respectively) and the fecal occult blood test (12.7%, n=7 vs. 13.9%, n=12, respectively).
The rate of complications associated with AGE in children treated by PG (n=36, 65.4%) was higher than that in children treated by GP (n=23, 26.7%) (p<0.05). Hemolytic uremic syndrome, sepsis, hypovolemic shock, renal failure, glomerulonephritis, seizures, methemoglobinemia, intussusception, acute appendicitis, and urticaria were the complications observed in these children.
DISCUSSION
This survey research investigated the most common practices among the members of the KSPGHAN with respect to the diagnosis and management of AGE in children, particularly focusing on the differences between the practices followed by PG and GP. Pediatricians across the entire country participated in this survey, and most respondents who answered the questionnaire were physicians who had worked as pediatricians for 5–10 years. The duration of clinical practice after achieving pediatric board accreditation was similar between PG and GP. Therefore, the results of this survey can be considered representative of the patterns of AGE diagnosis and management followed by Korean pediatricians. The members of the KSPGHAN include subspecialists, i.e., PG who are accredited by the Society of Korean Pediatrics. This present survey included responses from 55 PG and 87 GP. Most PG were employed at secondary and tertiary hospitals and managed hospitalized children.
Similarities were observed between PG and GP with regard to the guidelines governing the diagnosis, indications for admission, and hydration therapy utilized to treat AGE in children. Both PG and GP considered frequent vomiting and/or diarrhea as the primary clinical presentation of AGE in children.
With regard to the indications for admission, PG preferred hospitalization for children with chronic or underlying diseases. Children with underlying chronic conditions or those undergoing treatment may show a more severe and prolonged course of common diarrheal infections or may be at a greater risk of contracting opportunistic infections [
1]. Therefore, PG tended to recommend hospitalization for children with underlying diseases, since approximately 66% of PG were employed by tertiary hospitals. In Seoul, the 313 children hospitalized with a diagnosis of AGE included several children without diarrhea or vomiting, and the degree of vomiting differed among the 313 children based on age [
7]. Failure of ORT therapy is an important indication for hospitalization in children with AGE [
1]. This survey showed that 90.0% of PG and 97.0% of GP recommended hospitalization in children in whom oral intake was not possible secondary to vomiting. A study performed across 31 hospitals to evaluate the indications for admission in children with AGE showed that 57.5% of hospitalized children did not require hospitalization [
4]. Therefore, it is necessary to investigate whether the indications for hospitalization followed by Korean pediatricians are in accordance with the established guidelines.
Guidelines advocate standardized ORT in children with mild-to-moderate dehydration; however, these guidelines may not always be followed correctly in clinical practice [
10]. ORT has been shown to be as effective as IV rehydration in most children with mild-to-moderate dehydration and is more cost-effective [
511]. A survey performed among emergency physicians showed that only 34% of these physicians initiated ORT for this patient population and that most physicians who chose this approach were pediatric emergency physicians [
6]. The present survey reported that a small number of pediatricians used ORT and that 66% of pediatricians used IV hydration to manage dehydration. These results concurred with an Italian study in which 74.0% (453/612) of children with AGE received IV rehydration [
4]. The aforementioned finding (ORT prescribed by only a small number of pediatricians to manage dehydration) might be attributed to the fact that the questionnaire did not clearly distinguish between ORT and IV hydration.
ORT is the first-line therapy to treat moderate dehydration in children with AGE [
1213]. A systematic review investigating the management of hydration in pediatric AGE reported no difference in the duration of hospitalization between children who received IV hydration and those who received ORT. Phlebitis and paralytic ileus were common adverse effects associated with IV hydration [
14]. Parents and emergency physicians favor IV fluid therapy to treat mild or moderate dehydration when vomiting is the major symptom [
141516]. IV hydration is preferred over ORT to manage dehydration, which might be attributed to the fact that hospital and health care services are easily accessible in Korea. No complication associated with IV hydration was reported in this survey. Further studies are warranted to determine the optimal hydration approach based on the degree of dehydration in children with AGE. Additionally, why Korean pediatricians prefer IV hydration should be investigated in further studies.
This survey showed several significant intergroup differences in the symptomatic management of AGE in children. Clinical guidelines do not routinely advocate the use of antiemetics in children with AGE [
123]. An Italian study reported that only a small number of children were prescribed antiemetics, although 70% of the children presented with vomiting [
4]. In this survey, it was observed that 87.5% of PG and 96.4% of GP prescribed antiemetics in >50% of children with AGE, with domperidone being the most common antiemetic and trimebutine the 2nd most common antiemetic prescribed in this patient population. The ESPGHAN/European Society for Paediatric Infectious Diseases guidelines recommend ondansetron therapy to reduce the risk of persistent vomiting in children with AGE-induced vomiting [
17]. In Europe, domperidone is the preferred antiemetic [
18]. Few studies have reported the use of domperidone, and these have included small sample sizes and shown low methodological quality and inconsistent results [
1920]. Moreover, domperidone is not available in USA. Most Korean pediatricians prescribe domperidone to treat AGE-induced vomiting. Although ondansetron is the drug of choice to treat AGE-induced vomiting [
21], only 7% (n=6) of GP use ondansetron, which might be attributed to the fact that insurance coverage is unavailable for the use of ondansetron to treat AGE-induced vomiting. Further studies are warranted to investigate the indications and adverse effects of domperidone and ondansetron.
Probiotics are commonly prescribed by both PG and GP to shorten the duration of diarrhea. Probiotics are a first-line therapy for AGE along with rehydration [
22]. However, the beneficial effects of probiotics are strain-related; therefore, pooling data on different strains is inappropriate [
23]. The present survey showed that 89.1% of PG and 100% of GP prescribed probiotics and that
Saccharomyces boulardii and
Lactobacillus rhamnosus GG were the most common probiotics prescribed. Other commercially available antidiarrheal agents prescribed were smectite, racecadotril, loperamide, and zinc. Smectite was more commonly prescribed by GP and racecadotril by PG.
Although the BRAT diet comprising bananas, rice, applesauce, and toast is no longer promoted because of its low energy density and lack of protein or fat content, these food items can be added to the diet that is gradually reintroduced in these children (to add bulk to the diarrheal stool) [
24]. Inappropriate dietary changes in children hospitalized with AGE were associated with age, the number of diarrhea episodes, and episodes of vomiting [
4]. Dietary changes and milk (lactose) withdrawal are usually discouraged by all clinical practice guidelines. Lactose-free formula might be indicated in inpatient settings and in children with diarrhea continuing for >7 days. [
25]. In the present survey, dietary changes were recommended by 27.3% of PG and 58.9% of GP. The rate of dietary changes observed in the present survey was higher than that reported by Italian physicians (27.6%) [
4].
Antibiotics are not routinely recommended to treat pediatric AGE [
1]. Most clinical practice guidelines recommend a pathogen-based approach, and antibiotics are considered only in specific situations such as in very young infants (aged <3 months), children with underlying chronic conditions or immunodeficiency, and community-dwelling children to reduce the risk of spreading the infection [
25]. In this survey, the questionnaire inquired regarding the frequency of and indications for antibiotic prescription. It was observed that 75% of the pediatricians prescribed antibiotics only in children with diarrhea/blood and high fever. Prospective studies are warranted to assess the management of AGE in Korean children by categorizing this patient population into inpatient and outpatient groups to gain a better understanding of the treatment patterns for AGE and establish specific guidelines.
In the present survey, >50% of the respondents answered that tests to identify the etiological agents associated with AGE were performed only in hospitalized children. Microbiological tests including rotavirus antigen, virus and bacterial polymerase chain reaction, and stool cultures were more commonly advised by PG than by GP; however, this difference was not statistically significant. In fact, tests to identify etiological agents of AGE were only performed in hospitalized children. In a study reported in Italy, the occurrence of >5 diarrheal stools was the only factor associated with microbiological investigations and antibiotics were prescribed more commonly in children with blood in the diarrheal stool [
4]. Prospective studies are warranted to determine the primary causes of AGE in Korean children.
With respect to the multiple-choice questions regarding the interval required for symptomatic improvement of AGE, 60% of PG and 54.7% of GP reported improvement within a few days, indicating that >50% of all cases improved within a few days. Cause analysis is warranted among GP who conclude that the use of a greater number of drugs or dietary changes is required for the improvement of diarrhea. With respect to the complications associated with AGE, 69.1% of PG and 26.7% of GP reported AGE-induced complications. The complications reported in both groups were similar, and most physicians reported hemolytic uremic syndrome as a complication.
Limitations of the present study are as follows: 1. This was a survey-based study, and the accuracy of responses to the questionnaire depends upon the respondent's memory. Thus, inaccuracies in results cannot be excluded. 2. Only 35.3% of the members of the KSPGHAN responded to this survey. 3. The management of AGE differs on the basis of age and cause; however, this study did not assess the management of AGE in terms of the children's ages and causes of AGE in the study population.
In conclusion, this survey assessed the management of pediatric AGE and showed that the indications for admission and rehydration were similar between GP and PG, with IV hydration being the primary rehydration strategy adopted by most pediatricians for this patient population. Symptomatic treatment including antiemetic and antidiarrheal therapy was more commonly prescribed by GP than by PG in Korea than in other countries.