Introduction
Currarino syndrome is a congenital disorder characterized by the clinical triad of anorectal malformations, sacral agenesis, and a presacral mass such as an anterior meningocele [
1]. Chronic constipation is the most common symptom of this disorder, secondary to extrinsic compression of the presacral mass or anorectal malformations [
12]. In most cases, this condition is diagnosed in childhood, and rarely, in adulthood [
3]. We report a case of a 29-year-old woman who visited our gynecology department for evaluation of a pelvic mass who was diagnosed with Currarino syndrome. We have additionally reviewed the relevant literature.
Case report
A 29-year-old woman was referred to our hospital for evaluation of a pelvic mass that was identified during a gynecological examination at a local hospital in October 2017. She had visited the local clinic for a routine gynecological checkup before marriage. She denied any relevant family or medical history; however, she reported a history of chronic constipation since birth. Her menstrual cycle had been regular, i.e., every 30–35 days, since menarche at the age of 18 years. She often had mild dysmenorrhea but no pelvic pain. On speculum examination, the cervix showed a smooth surface but was deviated to the upper right. Her anus was relatively small (measuring approximately 1 cm in diameter), and the perineum was relatively long at approximately 5 cm.
Ultrasonography revealed a septate uterus with bilaterally normal ovaries. An approximately 10-cm solid calcified mass was observed in the left posterior portion of the uterus. This pelvic mass was suspected to be a subserosal myoma or non-gynecological mass. Pelvic magnetic resonance imaging (MRI) was performed to further evaluate the pelvic mass, which was identified as a fecal mass on MRI. The partial septate uterus showed right anterior displacement secondary to a massively distended rectum (
Fig. 1A). Rectal and anal sphincter stenoses were observed. A septated cystic mass measuring approximately 4.7×3.3×2.5 cm in size was observed in the right presacral area, and it was continuous with the dilated thecal sac through a right sacral defect, which was consistent with an anterior meningocele (
Fig. 1B). The sigmoid colon was dilated to 7–8 cm in diameter and extended to the anterior aspect of the liver and right subphrenic space (
Supplementary Fig. 1A). The right kidney of the patient was small in size (7×3.4×3 cm), and showed calyceal blunting and dilatation (
Supplementary Fig. 1B). The left kidney showed compensatory hypertrophy (12×7×6 cm). Plain radiography revealed a right-sided sacral bone defect; however, the right S1 was intact (scimitar sacrum;
Fig. 2). Abdominal radiographs showed a massively distended sigmoid colon filled with feces. Sacral dysgenesis was observed below the level of the right S2 and around the left S4, along with erosive changes.
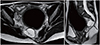
Fig. 1
Pelvic magnetic resonance image shows (A) a partial septate uterus (1.7 cm of the muscular septum) with right anterior displacement secondary to a massively distended rectum. (B) Right-sided anterior sacral meningocele (arrow) is observed.
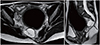
Fig. 2
Abdominal radiograph shows sacral hypogenesis (scimitar sacrum) and a massively distended sigmoid colon filled with feces.

Physical examination and imaging studies suggested Currarino syndrome characterized by a presacral mass, anorectal malformations, and sacral agenesis. The patient was transferred to a tertiary hospital for further evaluation and treatment.
Discussion
Currarino syndrome is a rare autosomal dominant hereditary disorder [
4]. Since the Currarino triad was first described by Currarino in 1981, approximately 300 cases have been reported [
345]. However, the exact incidence of this condition is unknown owing to its multiple phenotypes and clinical presentations [
5]. Recent studies have reported an association between Currarino syndrome (primarily sacral agenesis) and the
HLXB9 gene located on chromosome 7q36 [
4]. Reportedly, an
HLXB9 gene mutation was identified in approximately 90% of familial cases and 30% of sporadic cases [
6]. The female-to-male ratio was reported to be 3:1 among non-familial and 1:1 among familial cases [
47]. The higher incidence rate in women is attributable to the greater number of hospital visits made by women for gynecological and/or urological symptoms [
4].
Patients usually present with various symptoms, including meningitis, perianal abscess, abdominal distention, bowel obstruction, chronic constipation, and/or urinary tract infection [
12345]. Chronic constipation is the most common symptom [
1]. Our patient reported a history of chronic constipation since childhood. Constipation is attributable to anal malformations and compression caused by the presacral mass [
78]. Most patients are diagnosed in childhood; this condition is rarely observed in adults [
3]. A previous report described a 30-year-old woman who was diagnosed with Currarino syndrome after gynecological evaluation for recurrent abortion [
7]. She reported a several-year history of low back pain and chronic constipation since birth. She had undergone surgery for anal atresia at 6 months of age. Gynecological workup revealed a bicornuate uterus and sacral bone defect. Pelvic MRI revealed an extremely large anterior sacral meningocele, and she was referred to the Department of Neurosurgery. Another case report described a 22-year-old woman with chronic constipation who visited a neurosurgical clinic [
2] and was diagnosed with Currarino syndrome on the basis of pelvic radiographs and MRI, which showed partial sacral agenesis, meningocele, and a bicornuate uterus. She reported a history of constipation since birth and had undergone anorectoplasty for congenital anal atresia at 3 years of age. Previous reports have described patients with anal malformations such as anal stenosis, which were diagnosed and treated during childhood [
2]. Although not diagnosed as having Currarino syndrome at the time of presentation (in childhood), these patients were diagnosed in adulthood when they presented with other associated symptoms [
247]. Therefore, the diagnosis of anal malformations during childhood warrants additional evaluation to exclude Currarino syndrome.
Patients with Currarino syndrome show a highly variable clinical presentation. In women, gynecological malformations, including a bicornuate or septate uterus and a rectovaginal fistula, have been reported in 19% of cases [
4]. These uterine structural abnormalities can cause infertility, recurrent miscarriage, and premature births [
7]. Therefore, women diagnosed with Currarino syndrome should undergo gynecological evaluation to identify the structural abnormality.
Physical examination and imaging studies, including radiography, ultrasonography, computed tomography, and MRI, are useful diagnostic tools. Pelvic MRI is useful to distinguish between a presacral mass and the surrounding structures. The presacral mass is primarily an anterior meningocele, although teratomas, hamartomas, and neurogenic cysts, among other such lesions, may occur. In addition, MRI is useful to identify other deformities related to the spinal canal [
17]. The treatment of Currarino syndrome depends on its presentation. Anorectal malformations require an anorectoplasty; however, conservative management could be attempted if symptoms are not severe [
78]. An anterior meningocele requires urgent surgical treatment to avoid the risk of meningitis [
57]. Notably, an enlarging presacral mass may cause acute symptoms such as bowel obstruction secondary to a mass effect and, therefore, requires prompt treatment [
3].
In summary, a 29-year-old woman visited our gynecology department with a suspicious pelvic mass. Her anus was relatively small, and she reported a history of chronic constipation since birth. Gynecologists should be aware of the possibility of Currarino syndrome in patients who seek treatment for a presacral mass. Women presenting for a gynecological examination require a thorough examination to rule out Currarino syndrome if their physical examination shows anorectal malformations, presacral mass, or similar suspicious symptoms.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download