Abstract
Alcohol use disorder is a kind of chronic illness that is difficult to treat. The disorder often recurs easily and patients visit the outpatient clinic while intoxicated. Therefore, is often too difficult to treat all people of concern, i.e., the caregiver, patient, and doctor, due to the frequent helpless and hopeless relapse. If the patient has severe withdrawal symptoms or poor physical condition, it is very difficult to maintain treatment at an outpatient clinic. On the other hand, many patients abstain or reduce drinking and go on to live a sober life by outpatient-based management. In addition, psychosocial treatment techniques and efficient medications are available at the level of a psychiatric outpatient clinic. Under the scope and limitations of outpatient-based approaches, patients with alcohol use disorder can develop a new life called ‘recovery’ with the help of psychiatrists, by the way of motivating changes, correcting cognitive errors, establishing effective coping skills, utilizing external resources actively, and facilitating healthy roles with their families.
Figures and Tables
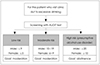
Fig. 1
Differentiation of the levels of risk by the AUDIT score. AUDIT: alcohol use disorder identification test. Adapted from Ministry of Health and Welfare.10)
References
1. Health Insurance Review & Assessment Service. The most frequent mental disorders by age groups. updated 2018 Dec 13. cited 2019 Jul 21. Available from: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020041000100&brdScnBltNo=4&brdBltNo=9731.
2. National Center for Mental Health, Health Insurance Review & Assessment Service, Korea Institute for Health and Social Affairs. National Mental Health Statistics_pilot study. Seoul: National Center for Mental Health;2018.
3. The Ministry of Health and Welfare. The survey of mental disorders in Korea. Sejong: The Ministry of Health and Welfare;2017.
4. Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER. Treating tobacco use and dependence: clinical practice guideline. Rockville, MD: US Dept of Health and Human Services, Public Health Service;2000.
5. Anderson P, O'Donnell A, Kaner E. Managing alcohol use disorder in primary health care. Curr Psychiatry Rep. 2017; 19:79.

6. Kim HS, Oh DY. Study for characteristics of alcohol dependence patients using DrInC scale. J Korean Acad Addict Psychiatry. 2000; 4:108–122.
7. Korea Health Promotion Institute. Health promotion statistics year book. Seoul: Korea Health Promotion Institute;2017.
8. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test: guidelines for use in primary care. Geneva: World Health Organization;2001.
9. Willenbring ML, Massey SH, Gardner MB. Helping patients who drink too much: an evidence-based guide for primary care clinicians. Am Fam Physician. 2009; 80:44–50.
10. Ministry of Health and Welfare. Guideline development of prevention and brief intervention for 4 major addiction problems. Seoul: The Catholic University of Korea Industry-Academic Cooperation Foundation;2013.
11. Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007; 31:1208–1217.

12. Sobell LC, Sobell MB. Timeline follow-back. In : Litten RZ, Allen JP, editors. Measuring alcohol consumption. . Totowa, NJ: Humana Press;1992. p. 41–72.
13. Kim JS, Park BK, Kim GJ, Oh MK, Lee CS, Yu NJ, et al. Assessing the insight status using HAIS (Hanil Alcohol Insight Scale), a new devised scale for qualitative and quantitative evaluation of insight in alcohol dependents. J Korean Acad Addict Psychiatry. 1998; 2:126–133.
14. Marshall EJ, Humphreys K, Ball DM. Physical complications of excessive drinking. In : Marshall EJ, Humphreys K, Ball DM, editors. The treatment of drinking problems: a guide to the helping professions. 5th ed. Cambridge: Cambridge University Press;2010. p. 50–72.
15. Korean Academy of Addiction Psychiatry. Alcohol use disorder. Addiction treatment guidelines series. Seoul: Korean Academy of Addiction Psychiatry;2011.
16. Emmelkamp PMG, Ellen V. Evidence-based treatment for alcohol and drug abuse. New York, NY: Routledge;2006.
17. Bujarski S, O'Malley SS, Lunny K, Ray LA. The effects of drinking goal on treatment outcome for alcoholism. J Consult Clin Psychol. 2013; 81:13–22.

18. Namgung K. You can treat the patients with alcohol dependence. . Seoul: Chungnyun Euisa;2001.
19. Project MATCH: rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993; 17:1130–1145.
20. Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York, NY: Guilford Press;1991.
21. DiClemente CC, Hughes SO. Stages of change profiles in outpatient alcoholism treatment. J Subst Abuse. 1990; 2:217–235.

22. Oh SH, Han CW, Seo JS, Joe KH, Lee HK, Yoon HG, et al. Korean addiction treatment, guidelines (III): psychosocial treatment of alcohol use disorder. J Korean Neuropsychiatr Assoc. 2014; 53:221–227.

23. National Institute for Health and Clinical Excellence. Alcohol use disorders: the NICE Guideline on the diagnosis, assessment and management of harmful drinking and alcohol dependence (national clinical practice guideline). London: The Royal College of Psychiatrists Publications;2011.
24. National Alcohol Strategy. The treatment of alcohol problems: a review of the evidence. Canberra: Department of Health and Ageing & National Alcohol Strategy;2003.
25. Practice guideline for the treatment of patients with substance use disorders: alcohol, cocaine, opioids. American Psychiatric Association. Am J Psychiatry. 1995; 152:1–59.
26. Beck AT, Wright FD, Newman CF, Lies BS. Cognitive therapy of substance abuse. New York, NY: Guilford Press;1993.
27. Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006; 295:2003–2017.

28. Nowinski J, Baker S, Carroll KM. Twelve step facilitation therapy manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, MD: US Department of Health and Human Services;1992.
29. American Psychiatric Association. The American Psychiatric Association practice guideline for the pharmacological treatment of patients with alcohol use disorder. Washington, DC: American Psychiatric Association Publishing;2018.
30. Drummond C. Alcohol-use disorder. updated 2018 Jun. cited 2019 Jul 3. Available from: https://bestpractice.bmj.com/topics/en-us/198.
31. Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014; 311:1889–1900.

32. Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013; 108:275–293.

33. Rösner S, Leucht S, Lehert P, Soyka M. Acamprosate supports abstinence, naltrexone prevents excessive drinking: evidence from a metaanalysis with unreported outcomes. J Psychopharmacol. 2008; 22:11–23.

34. Ragia G, Manolopoulos VG. Pharmacogenomics of alcohol addiction: personalizing pharmacologic treatment of alcohol dependence. Hospital Pharmacology. 2014; 1:147–167.

35. Jeong JY, Yoon HJ, Kim SR, Lee KS. Comparisons of naltrexone and acamprosate's medication compliance for 12 months in patients with alcohol dependence. J Korean Acad Addict Psychiatry. 2011; 15:58–64.
36. Thase ME, Salloum IM, Cornelius JD. Comorbid alcoholism and depression: treatment issues. J Clin Psychiatry. 2001; 62 Suppl 20:32–41.
37. Kang CJ, Kim SG, Namkoong K, Cho DH, Lee BO, Choi IG, et al. Non-relapse rate in a 24 week follow-up clinical study with Korean male alcohol-dependent patients. J Korean Neuropsychiatr Assoc. 2006; 45:42–48.
38. Miller M, Gorski TT, Miller DK. Learning to live again: a guide for recovery from chemical dependency (updated and revised). Independence, MO: Herald Pub House;1992.
39. Douaihy A, Daley DC, Marlatt GA, Donovan DM. Relapse prevention: clinical models and intervention strategies. In : Ries RK, Fiellin DA, Miller SC, Saitz R, editors. The ASAM principles of addiction medicine. China: Wolters Kluwer Health;2014. p. 991–1007.
40. Yoon MS. Addiction and family. In : Joe KH, Kwon DH, Kim DJ, Kim JM, Kim HO, Roh SW, editors. Comprehensive textbook of addiction. Seoul: Hakji Press;2011. p. 259–305.
41. Dasarang Addiction Research Institute. Recovery class for the alcoholics and their family. Seoul: Hana Medical Book;2007. p. 61–76.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download