I. Introduction
The rise in traffic accidents combined with the increasing speed of modern vehicles has led to an increase in the number and complexity of midfacial injuries. The management of such complicated panfacial cases requires meticulous planning and skill, as the maintenance of aesthetics is a major concern in this region. Five basic principles of craniomaxillofacial fracture management are: 1) precise anatomic diagnosis, 2) direct fracture exposure, 3) reduction and rigid internal fixation, 4) primary bone grafting, and 5) periosteal and soft tissue suspension with repair
1. Hence, an approach that fulfills these principles with minimal or no skin scarring and which presents a low risk to the vital structures is ideal. Thus, maxillofacial surgeons must have expertise in various approaches to the midface and craniofacial regions. Although midfacial degloving (MFD) is most commonly used by otorhinolaryngologists, it is useful in many maxillofacial surgical procedures, as the entire midface is accessible by way of a single flap. This method of rhinoplastic release of the nasal soft tissues in combination with bilateral anterior maxillary exposure provides wide surgical access to the midface without a visible facial scar and can be combined with coronal, brow, temporal, and palatal incisions for more complicated surgeries
2. Due to positive outcomes of past studies, we decided to consider MFD as an approach for maxillofacial injuries. The aim of the present study was to evaluate the versatility and feasibility of the MFD approach in patients with maxillofacial trauma, posttraumatic deformity, and requiring reconstruction of facial deformity. We also attempted to evaluate the advantages and complications associated with this approach.
II. Materials and Methods
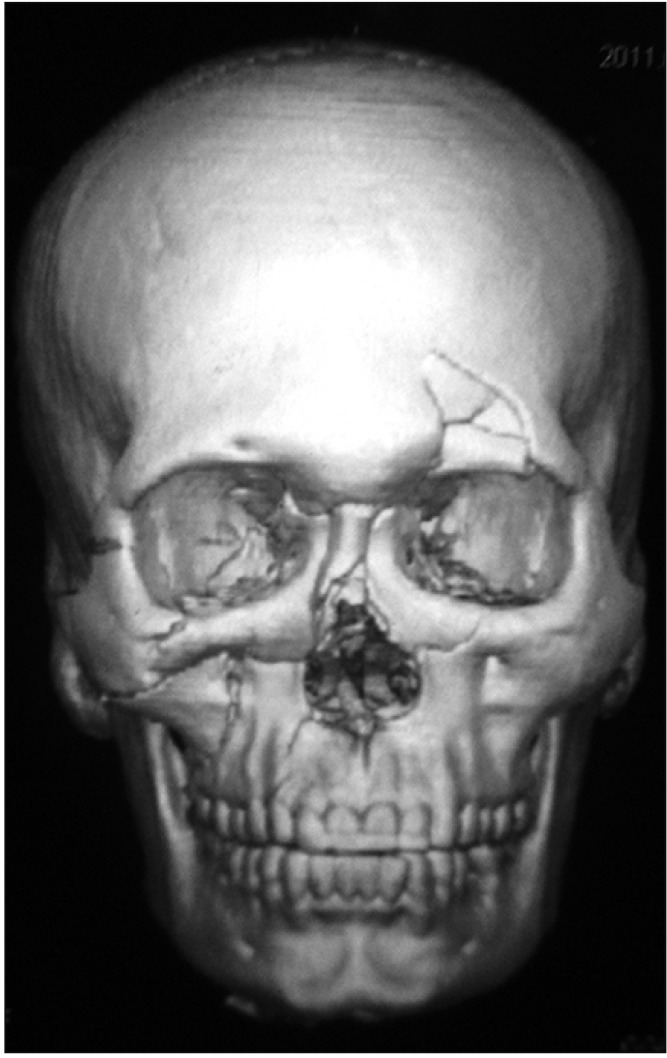
In this study, five male patients aged from 21 to 55 years old were operated on using the MFD approach under general anesthesia in the Department of Oral and Maxillofacial Surgery, Tamilnadu Government Dental College and Hospital (Chennai, India) from January 2011 to January 2012. All patients had naso-orbito-ethmoidal complex and midface fractures. Patients' complete medical and dental history, previous history of trauma or surgery in the midface region, and pre-existing nasal stenosis was recorded. Local examinations were done to elicit midfacial sensory deficits. None of the patients had orbital complications like restriction of eye movements, diplopia, enophthalmos, or epiphora. The written informed consent was obtained after explaining the procedure and its complications to the patients before surgery. This study was approved by the Institutional Ethical Committee of Tamilnadu Government Dental College and Hospital (No. 0430/DE/2010).
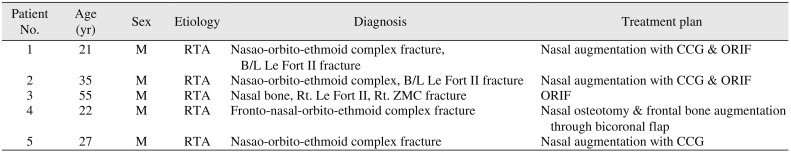
Three patients (patient Nos. 1-3) were treated with open reduction and internal fixation and two patients (patient Nos. 4 and 5) were treated for secondary corrections using the MFD approach. Costal cartilage was used for nasal augmentation in three patients (patient Nos. 1, 2, and 5). Nasal osteotomy was performed and an additional bicoronal incision was used in one patient (patient No. 4) for frontal bone augmentation. (
Table 1) Postoperative clinical evaluation was performed for the assessment of fracture reduction, aesthetics, function, and complications. The follow-up period ranged from three to six months with review on the first, seventh, and 15th days and during the first, third, and sixth months postoperatively, respectively. Pre- and postoperative photographs were taken for comparison of clinical findings. Occipitomental skull radiographs were obtained at one month postoperatively for the assessment of fracture reduction and stability. Neurosensory deficits were reviewed by clinical examination (cold, light touch, and two-point discrimination).
We followed the technique illustrated by Har-El
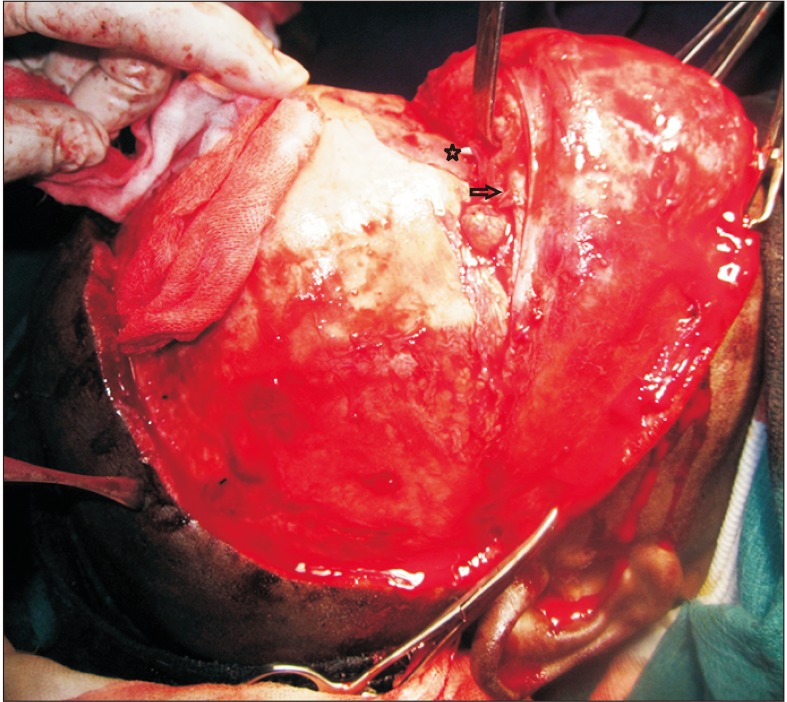
3. After securing the endotracheal tube, lidocaine with 1:100,000 adrenaline was infiltrated into the maxillary labial vestibule and into the nasal cavity as done for rhinoplasty procedures. A sublabial incision was made from the first molar, extending to the contralateral first molar followed by mucoperioasteal flap elevation until the pyriform aperture and infraorbital rim were exposed, which was done carefully to protect the infraorbital nerve. An intranasal incision was started with a complete transfixion incision, then bilateral intercartilaginous incisions (between the upper and lower lateral cartilages of the nose) were extended to meet the transfixion incision superiorly and caudally to complete circumvestibular incision of the nose. Soft tissues of the nasal dorsum, anterior maxillary sinus wall, and glabella up to the frontal bone were elevated through the intercartilagenous incisions. Intraoral and intranasal incisions were connected through the nasal sill incision.(
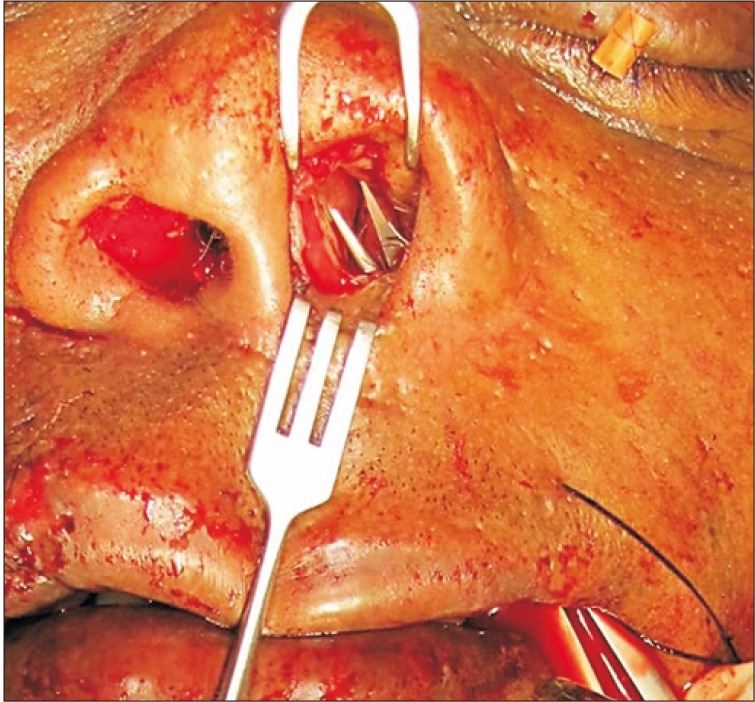
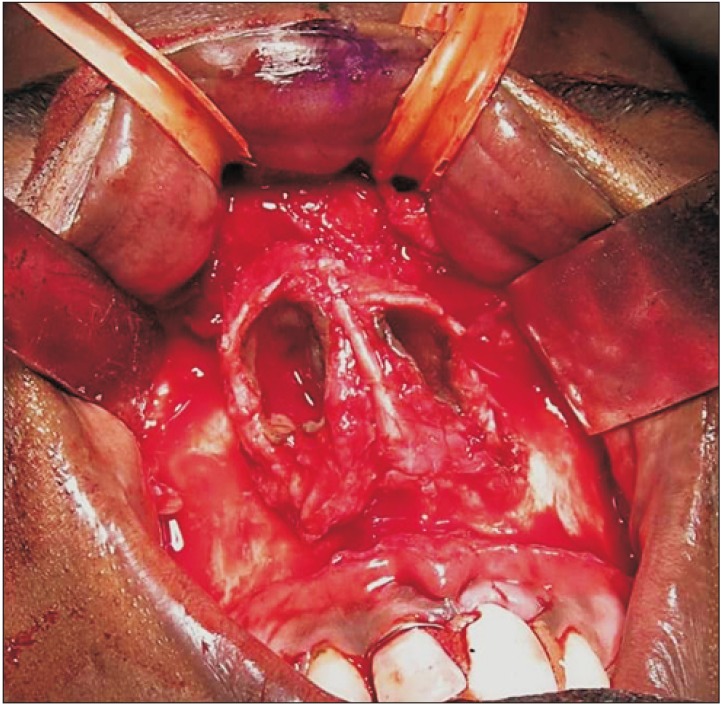
Fig. 1) As degloving continued, the midfacial skin was separated from the maxilla and the nasal pyramid. The flap included the lower lateral cartilages and columella with its medial crura. The bony nasal pyramid with the upper lateral cartilages was now fully exposed in the midface. Two rubber drains were placed through the nostrils and around the lip for retraction (
Fig. 2) and one of the drains was released every 15 to 20 minutes. Fractures were identified, reduced, and fixed with miniplates and screws. Grafting and osteotomy were performed wherever indicated. Intranasal and sublabial incisions were closed with 4-0 and 3-0 resorbable sutures, respectively. Intranasal packing and a nasal splint were placed. In patient No. 4, a bicoronal flap was elevated in addition to performing MFD. The bicoronal flap incision was marked with gentian violet ink at a point 4 cm posterior to the hairline, extending into the preauricular region bilaterally with cross hatches for exact approximation during closure. A standard bicoronal incision was made parallel to hair follicles with a scalpel extending deep until the galea in between the temporal lines. The incision below the temporal lines was deepened until the glistening superficial temporal fascia and the helix of the ear bilaterally were exposed. A subgaleal dissection was done and the flap was elevated forward up to 3 cm before the frontal bone defect. At this place, a periosteal incision was made and subperiosteal dissection was carried out until the supraorbital rims were seen. Supraorbital neurovascular bundles were identified and released to facilitate further retraction of the flap for extension into the nasoorbito-ethmoidal region, where it was connected to the MFD flap.(
Fig. 3) Nasal osteotomy and augmentation of the frontal bone defect was carried out easily with ample exposure provided by both flaps. Flaps were closed layer-wise with 3-0 Vicryl (Johnson & Johnson, New Brunswick, NJ, USA) and 3-0 Ethilon (Johnson & Johnson) sutures after placement of a suction drain to reduce postoperative edema.
III. Results
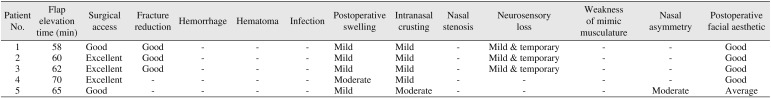
During this study, the MFD approach was satisfactory and the access provided was excellent for performing the planned procedures of reduction, fixation, and augmentation with the additional benefit of bilateral comparison in a single flap. MFD alone was sufficient in four patients, whereas, in one patient (patient No. 4), bicoronal incision was also used to address the depressed frontal bone fracture. Even in combination with a bicoronal flap, no evidence of ischemia (pallor or cyanosis) was noted and both flaps healed uneventfully. Esthetically satisfying results were achieved in all patients (
Fig. 4,
5) except in one patient (patient No. 5) in whom the costochondral graft became displaced. Hemorrhage, hematoma, or infection were not encountered in any of our patients. Mild to moderate crusting at the nasal incision site was complained of by all patients, which was managed by saline irrigations and resolved in an average of four weeks without much discomfort. Postoperative swelling at the nasal and midface regions was noticed, which resolved in an average of six weeks. Average time spent for flap elevation and exposure of the fracture site was 63 minutes. Mild weakness of the infraorbital nerve was present in the form of upper lip parasthesia in three patients (patient Nos. 1-3), in which manipulation of the fractures and miniplate fixations required flap retraction. However, this was transient and was completely resolved in an average of three weeks with oral steroids and vitamin B supplements. No permanent motor or sensory deficits were present in any patient. In this series, all patients complained of tightness in the nose which resembled vestibular narrowing for an average of eight weeks postoperatively, but all such symptoms resolved on their own without any treatment. There were no complaints of any complete nasal circumvestibular stenosis or any kind of difficulty and/or obstruction in the nasal airway.(
Table 2)
IV. Discussion
The MFD approach was first introduced by Casson et al.
4 in 1974 and popularized later by Maniglia
5, who published indications and the MFD technique in 1986. The excellent bilateral exposure of the midface with no functional disability and a low complication rate are the main advantages of this approach
6. In our study, we reduced and fixed midfacial fractures to their anatomical positions using the MFD approach. (
Fig. 6,
7) Access to the surgical site was excellent in all patients for performing the planned procedures.
MFD is also useful for nasal corrections in depressed and short noses, as extensive undermining of the paranasal region is necessary to obtain enough space for nasal augmentation
7. The nasal dorsum can be easily raised using bone grafting and the graft size can be shaved, controlled, and stabilized by a miniplate or screws
78. We performed nasal dorsum augmentation with costal cartilage in three patients (patient Nos. 1, 2, and 5). Costal cartilage was used because of its ease of manipulation, smooth surface, and flexibility. A cantilever costal cartilage graft was fixed with miniscrews in two patients (patient Nos. 2 and 5), whereas an L-shaped graft was used in one patient (patient No. 1). Aesthetically good results were achieved by sufficient nasal projection and raised dorsum of the nose (
Fig. 3,
4) in two patients, whereas, in one patient (patient No. 5), the graft was displaced due to fixation failure.
The most common complications and sequelae of the MFD technique are excessive intranasal crusting postoperatively and prolonged infraorbital nerve hypoesthesia
27910. In our study, all patients complained about intranasal crusting for an average of four weeks postoperatively, which resolved on its own after saline irrigations without much discomfort.
Lenarz and Keiner
10 identified transient paresthesia of the infraorbital nerve in five of 40 patients, while Price et al.
2 encountered temporary paresthesia in all of 48 patients in whom the MFD approach was used for tumor resection. In our study, three out of five patients (patient Nos. 1-3) who were operated on by open reduction and internal fixation of midface fractures experienced temporary infraorbital nerve paresthesia. This is mostly because of flap retraction and the manipulation of fracture fragments in the midface region. The finding resolved in an average of three weeks with vitamin B supplementation and low-dose oral steroids. The occurrence can be reduced by a careful positioning of retractors and avoidance of direct contact with or excessive stretching of the nerve. None of our patients suffered from permanent or prolonged paresthesia of the infraorbital nerve.
Baumann and Ewers
7 considered extensive subperiosteal stripping of the face especially in the zygoma region as a disadvantage of MFD, though they did not encounter any aesthetic sagging of tissues in all 14 of their patients in spite of extensive subperiosteal stripping. Our study showed neither postoperative tissue sagging nor weakness of the facial muscles in any patient.
Hyperplastic collagen deposition may occur underneath the flap over the nose and maxilla, resulting in sneer deformity. This becomes evident at six weeks postoperatively and slowly resolves. Six to 12 weeks postoperatively is a phase of active collagen deposition, in which vestibular narrowing resembling early stenosis is a common symptom. This should uniformly resolve without treatment
2. In our study, all patients complained of tightness in the nose which resembled vestibular narrowing for an average of eight weeks postoperatively and all symptoms resolved on their own without any treatment. Sneer deformity was not noticed in any patient.
Stenosis of the nose is often discussed as a disadvantage of the MFD approach. Partial stenosis of the nasal vestibule was found by Romo et al.
11 in five out of 24 cases after treating nasal septal perforation with the MFD approach. Additionally, Lenarz and Keiner
10 identified circular stenosis of the nose in one out of 40 patients, and Price et al.
2 found complete stenosis of the nose in two out of 48 patients treated by MFD for tumor resection. This complication can be avoided if the intranasal incisions are sutured exactly. In our study, no nasal stenosis or any kind of difficulty with breathing due to narrowing of the nasal airway were encountered. This may be attributed to careful attention to meticulous approximation and suturing intraoperatively.
We combined a bicoronal incision with the MFD approach for the augmentation of depressed frontal bone fracture by alloplastic graft in one patient (patient No. 4). No complication occurred due to combination of these two flaps, as the degloving flap is well-perfused with branches of the facial artery and other collateral vessels. No complications such as hemorrhage, hematoma, infection, neurosensory deficit, excessive scarring, alopecia, or temporal hollowing were noted with bicoronal flap. Mild edema was present postoperatively, which subsided within one week.
According to Cultrara et al.
12, the disadvantage of MFD is the need for familiarity with the surgical technique, which may be more complicated than facial and/or scalp incisions. To evaluate the ease of access through this approach, we calculated the time required for complete degloving of the midface. The timing ranged from 58 to 70 minutes with an average of 63 minutes, which is more than the time required for the bicoronal approach or other approaches used for maxillofacial surgeries. Despite the intricacies of the procedure, we found it to be a very versatile and useful option. Oral and maxillofacial surgeons must familiarize themselves with this approach in order to apply it in various midfacial surgeries wherever indicated.
V. Conclusion
Like any other surgical procedure, the MFD approach has pros and cons, but, if used in appropriate patients correctly, the advantages are more numerous than the few complications that are manageable and avoidable with minimal morbidity. Though our sample size was small in this study, the approach was found to be successful. Our observations and results are comparable to those of various studies in the past. This technique-sensitive approach cannot be used for every case, but it must be incorporated in the repertoire of every oral and maxillofacial surgeon.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download