Abstract
Patients with masticatory muscle tendon-aponeurosis hyperplasia (MMTAH) experience limited mouth opening due to restricted muscle extension. Hyperplastic aponeurosis and tendons lead to the restriction of muscle extension. The criteria for the diagnosis of MMTAH are limited mouth opening that progresses very slowly from adolescence, intraoral palpation reveals a hard cord-like structure along the overhang of the anterior border of the masseter muscle on maximum mouth opening, and a square mandible. Conservative treatment, including pharmacotherapy, occlusal splint and physical therapy are ineffective. The standard therapy is surgical treatment, such as anterior partial aponeurectomy of the masseter muscle and coronoidectomy. The long-term results are very satisfying.
Limited mouth opening may be caused by various diseases, such as temporomandibular disorders, fracture of the condylar process, neurological disorders, rheumatoid arthritis, inflammatory disease, tumors and hyperplasia of the coronoid process12. Masticatory muscle tendon-aponeurosis hyperplasia (MMTAH) is a new clinical condition associated with limited mouth opening.
In 2000, Inoue et al.3 reported a patient with hyperplasia of only the masseter muscle aponeurosis, accompanied by limited mouth opening and a square mandible. Moreover, Murakami et al.4 reported 10 chronic severe mandibular hypomobility patients exhibiting square mandible with hyperplasia of the mandibular angle. Beckers5 reported a patient with bilateral masseter muscle hypertrophy accompanied by limited mouth opening in 1977 from Switzerland. Her mandible appeared square and bilateral resection of the masseter muscles did not improve limited mouth opening. Thus, cases of limited mouth opening accompanied by a characteristic square mandible have been reported.
In 2005, MMTAH was recognized as a new disease at the conference of the Japanese Society for Oral and Maxillofacial Surgeons. Subsequently, the disease was defined and approved at the conference for the Japanese Society of Temporomandibular Joint in 20086. In 2009, the disease name of MMTAH was first published in an international journal by Yoda et al.7. Thereafter, MMTAH came to be very well known disease. In 2014, a case of MMTAH was reported from Switzerland by Worni et al.8. In 2015, Lehman et al.9 reported four female patients who presented limited mouth opening. Although they were not diagnosed with MMTAH, we consider that these must have been cases of MMTAH10. Furthermore, anesthesiologists reported cases of MMTAH that resulted in difficult laryngoscopy after the initiation of anesthesia11.
The main symptom of MMTAH is limited mouth opening. Because the condition progresses very slowly from adolescence, patients have few subjective symptoms and limited mouth opening may only be identified by dentists during visits to dental clinics. In the 142 patients reported at the conference for the Japanese Society of Temporomandibular Joint, the maximum opening at the first medical examination was 5 to 43 mm (mean, 23.5 mm)11. Patients usually have no pain in the region of the temporomandibular joint or muscles, and the lateral and anterior movements of the mandible are not limited.
A characteristic feature of this disease is a square mandible with a small gonial angle and flattening of the occlusal planes1213.(Fig. 1, 2) The square mandible, which exhibits a prominent mandibular angle, may be due to hyperplasia of the aponeurosis and tendon. Both coronoid processes are thickened anteroposteriorly, but there is no contact between the coronoid process and the zygomatic arch on mouth opening.
Magnetic resonance imaging (MRI) shows a hyperplastic aponeurosis and masseter muscle. In horizontal MRI sections, the bilateral overhang of the masseter muscle along the anterior border of the mandibular ramus is noted, and low intensity areas showing the aponeurosis are detected on the lateral aspect and inside the masseter muscle14. Minowa et al.15 reported that aponeuroses are rarely found below the lower half of the anterior margin of the masseter muscles. However, thickened aponeuroses are often observed to extend into this lower half in patients with MMTAH. On maximum mouth opening, intraoral palpation along the anterior border of the masseter muscle reveals a hard cord-like structure resulting from hyperplasia of the aponeuroses, which is consistent with the MRI findings.(Fig. 3)
The diagnostic criteria for MMTAH are as follows: (1) limited mouth opening that progresses very slowly from adolescence and no limitation of lateral or anterior mandibular movement; (2) intraoral palpation reveals a hard cord-like structure along the overhang of the anterior border of the masseter muscle on maximum mouth opening (Fig. 4); and (3) a square mandible7.
Although MRI can help visualize tendons and aponeuroses, the criteria for diagnosing hyperplasia in these tissues have not yet been established.
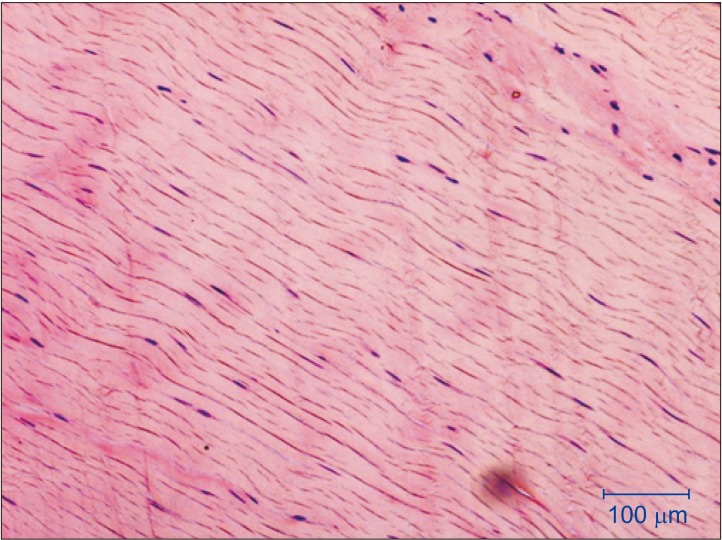
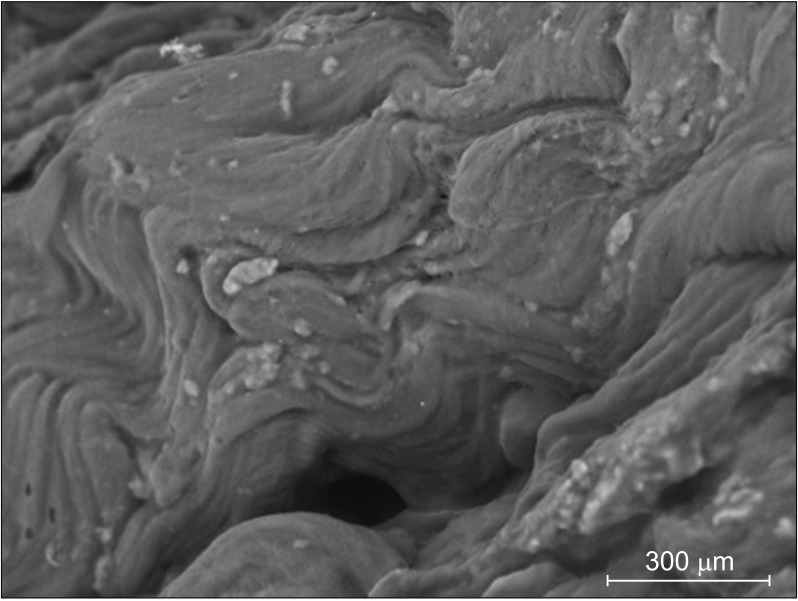
Tendon and aponeuroses tissues in MMTAH show normal structures on macroscopic examination17.(Fig. 5) This finding suggests that tendon tissues in MMTAH undergo hyperplasia. However, the aberrant sound heard on cutting tendon tissues with scissors indicates hardness of the tendon tissues, suggesting occurrence of anomalous changes7. Electron microscopy reveals mineralized nodules in the tendon tissues of MMTAH patients, in comparison to tendon tissues of individuals without facial deformity (FD)18.(Fig. 6) On energy dispersive X-ray analysis, silicon, calcium, and phosphorous are observed in the tendons of MMTAH patients18.
Moreover, according to a proteomic analysis of the temporalis muscle tendon of MMTAH patients and in comparison to FD, fibrinogen fragment D and β-crystallinA4 (CRYBA4) were upregulated, while myosin light chain 4 (MYL4) was downregulated in MMTAH patients1920. Inactivation of myosin II causes abnormalities in the collagen fibers of the tendon along with downregulation of MYL4, suggesting that MYL4 reduction is associated with pathological conditions in MMTAH. CRYBA4, which plays a vital role in protecting cells in non-lens tissues from damage caused by environmental and/or metabolic stress, is upregulated in the tendons of MMTAH patients, thus indicating that it may have a role in the stress response or pathology associated with the development of MMTAH.
The etiology of MMTAH remains unclear. MMTAH is more common in women and parafunctional habits such as a clenching or grinding are often associated with the condition. It is therefore suggested to be an acquired disease due to work hypertrophy3. We examined the effect of estrogen on the tenocyte function and the relationship between mechanical stress and crystallin beta A4 (Cryba4), using murine TT-D6 tenocytes. A physiological dose of estrogen increased the levels of scleraxis and tenomodulin (markers of tendon development) in TT-D6 tenocytes. A mechanical loading assay using tensile force revealed that tensile force increases the Cryba4 levels in tenocytes21. This suggests that mechanical stress may affect tendon differentiation.
However, all cases of MMTAH progress very slowly from adolescence and show bilateral involvement. These clinical futures suggest the possibility of congenital disease. Thus, we hypothesize that this disease has both environmental and genetic factors, as a multifactorial genedisease22.
Conservative treatments such as mouth opening training, pharmacotherapy, occlusal splint have shown no significant Conservative treatments such as mouth opening training, pharmacotherapy, occlusal splint have shown no significant effects in patients with MMTAH. The standard therapy is surgical treatment, including anterior partial aponeurectomy of the masseter muscle, and coronoidectomy7. Coronoidectomy should be performed to remove the tendon arising from the posterior and superior aspects of the coronoid process. Although mandibular anglectomy is also reported2324, we think that it is unnecessary for the improvement of the limited mouth opening. However, mandibular anglectomy can still be performed for aesthetic reasons.
We previously reported a case presentation with videos25, in which we introduced the surgical procedures for MMTAH patients in detail. Surgical treatment is performed under general anesthesia. Muscular relaxation does not improve the restricted mouth opening.
An incision is made in the oral mucosa, the same as in sagittal split ramus osteotomy, and the anterior margin of the mandibular ramus is exposed. The masseter muscle will then be visible on the outer aspect of the mandibular ramus. The aponeurosis is revealed and exhibits a silvery-white color on the exfoliating upward and outward of the masseter muscle.(Fig. 7) The aponeurosis are detached from the muscle tissue and excised as large as possible using scissors or electrosurgical knives. Aponeurectomy of the masseter muscle should be performed bilaterally.
The temporal tendon attached to the coronoid process is then exposed. An abnormal sound can be heard on exfoliating this periosteum with a raspatory. Then the anterior, lateral and medial tendons are removed from the coronoid process. (Fig. 8) Although the posterior tendon should be cut as much as possible, it is often difficult to excise it completely. By clasping the coronoid process tightly with the help of a Pean or Kocher forceps, the coronoid process is excised using cutting instruments, such as a Lindemann drill or an ultrasonic surgical instrument. Coronoidectomy should be performed bilaterally. After confirming that the mouth has opened more than 45 mm, the surgical incision can be closed using sutures. Continuous intraoral drainage is effective for reducing postoperative swelling and conducting mouth opening training.
Immediate oral intake and training in intentional clenching are required postoperatively to prevent open bite. Mouth opening training should be started 5 days after surgical treatment. Postoperative mouth opening training is an important prognostic factor. The training involves widely opening the mouth for 30 seconds with the help of a mouth opener. This is repeated more than 3 times, using analgesics to control the pain. The patient is discharged once they can open their mouth more than 40 mm without using the mouth opener. This training should be continued for at least 6 months.
In previous reports, patients who underwent surgical treatment showed good long-term results7. MRI after 1 year reveals that the temporal muscle is reattached to the resected stump of the bone, and a reduction in the cross-sectional area of the masseter muscle26.
We compared the outcomes of patients who underwent surgery (19 patients) and those who did not (9 patients)27. The mean increase in mouth opening after 2 years was 20.2 mm in the surgical group and 2.4 mm in the non-surgical group. Adequate mouth opening training for 6 months after surgery was a key factor for obtaining good outcomes. Thus, the general condition and personality of individual patients should be evaluated carefully before surgery to predict whether or not they will be able to endure the pain associated with postoperative mouth opening training.
MMTAH is still new and is hardly recognized in Korea. However, there are definitely MMTAH patients in Korea. This author hypothesizes that it is probably misdiagnosed as a refractory temporomandibular disorder. Surgery is useful for the management of MMTAH. It is my hope that the wide recognition of MMTAH will contribute to the health of patients.
Notes
Ethics Approval and Consent to Participate: Written informed consent was obtained from an individual participant included in the study.
Consent for Publishing Photographs: Written informed consent was obtained from the patient for publication of this article and accompanying images.
How to cite this article: Yoda T. Masticatory muscle tendon-aponeurosis hyperplasia accompanied by limited mouth opening. J Korean Assoc Oral Maxillofac Surg 2019;45:174–179. https://doi.org/10.5125/jkaoms.2019.45.4.174
References
1. Dhanrajani PJ, Jonaidel O. Trismus: aetiology, differential diagnosis and treatment. Dent Update. 2002; 29:88–92. 94PMID: 11928347.

2. Satheeshkumar PS, Mohan MP, Jacob J. Restricted mouth opening and trismus in oral oncology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014; 117:709–715. PMID: 24842447.

3. Inoue N, Yamaguchi T, Satou J, Satou C, Minowa K, Iizuka T. A case of restricted mandibular movement resulting from hyperplasia of the masseter muscle aponeurosis. Jpn J Oral Maxillofac Surg. 2000; 46:307–309.

4. Murakami K, Yokoe Y, Yasuda S, Tsuboi Y, Iizuka T. Prolonged mandibular hypomobility patient with a “square mandible” configuration with coronoid process and angle hyperplasia. Cranio. 2000; 18:113–119. PMID: 11202821.

5. Beckers HL. Masseteric muscle hypertrophy and its intraoral surgical correction. J Maxillofac Surg. 1977; 5:28–35. PMID: 265349.

6. Kakudo K, Yoda T. New concept of limited mouth opening associated with square mandible: diagnosis and treatment for masticatory muscle tendon-aponeurosis hyperplasia. J Jpn Soc TMJ. 2009; 21:28–30.
7. Yoda T, Sato T, Abe T, Sakamoto I, Tomaru Y, Omura K, et al. Long-term results of surgical therapy for masticatory muscle tendon-aponeurosis hyperplasia accompanied by limited mouth opening. Int J Oral Maxillofac Surg. 2009; 38:1143–1147. PMID: 19682860.

8. Worni A, Mericske-Stern R, Iizuka T, Büttner M. Eingeschärnkte Mundöffnung-was nun? Swiss Dent J. 2014; 124:935–944. PMID: 25253540.
9. Lehman H, Fleissig Y, Abid-el-raziq D, Nitzan DW. Limited mouth opening of unknown cause cured by diagnostic coronoidectomy: a new clinical entity? Br J Oral Maxillofac Surg. 2015; 53:230–234. PMID: 25596795.

10. Yoda T, Sato T. Re: Limited mouth opening of unknown cause cured by diagnostic coronoidectomy: a new clinical entity? Br J Oral Maxillofac Surg 2015:53(3):230–4. Br J Oral Maxillofac Surg. 2015; 53:476–477.

11. Arika T, Kakudo K. Hyperplasia of tendon and aponeurosis of masticatory muscles (HyTAM)-clinical appearance. J Jpn Soc TMJ. 2009; 21:31–34.
12. Nakamoto N, Sato T, Enoki Y, Nakamoto A, Hori N, Fukushima Y, et al. An analysis of maxillofacial morphology of patients with hyperplasia of the tendon and aponeurosis of masticatory muscles using cephalometric radiography. J Jpn Soc TMJ. 2011; 23:149–154.
13. Yoda T. [New diagnoses and treatments of temporomandibular disorders aided by chart illustrations]. Tokyo: Ishiyaku Publishers;2012. Japanese.
14. Kobayashi K, Shimoda S, Yoda T, Kakudo K. Current status of MR imaging for the masticatory muscle tendon-aponeurosis hyperplasia. J Jpn Soc TMJ. 2009; 21:35–39.
15. Minowa K, Inoue N, Ashikaga Y, Yoshida S, Totsuka Y, Nakamura M. Comparison of magnetic resonance imaging and gross findings regarding masseter muscle aponeuroses in cadavers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 86:275–279. PMID: 9768414.

16. Hayashi N, Yoda T, Tomoda T, Yumoto M, Kitamura T, Okubo M, et al. Longitudinal epidemiological survey on suspected masticatory muscle tendon-aponeurosis hyperplasia in adolescents. J Jpn Soc TMJ. 2018; 30:187–194.
17. Chiba R. Histopathologic evaluation of aponeurectomy materials in masticatory muscle tendon-aponeurosis hyperplasia. J Jpn Soc TMJ. 2009; 21:51–54.
18. Sato T, Hori N, Nakamoto N, Akita M, Yoda T. Masticatory muscle tendon-aponeurosis hyperplasia exhibits heterotopic calcification in tendons. Oral Dis. 2014; 20:404–408. PMID: 23750917.

19. Sato T, Nakamoto A, Hori N, Enoki Y, Fukushima Y, Nakamoto N, et al. Proteomic analysis of masticatory muscle tendon-aponeurosis hyperplasia: a preliminary study using a 2D-DIGE system. J Oral Maxillofac Surg Med Pathol. 2012; 24:185–188.

20. Nakamoto A, Sato T, Hirosawa N, Nakamoto N, Enoki Y, Chida D, et al. Proteomics-based identification of novel proteins in temporal tendons of patients with masticatory muscle tendon--aponeurosis hyperplasia. Int J Oral Maxillofac Surg. 2014; 43:113–119. PMID: 23870541.

21. Hayashi N, Sato T, Kokabu S, Usui M, Yumoto M, Ikami E, et al. Possible association of oestrogen and Cryba4 with masticatory muscle tendon-aponeurosis hyperplasia. Oral Dis. 2019; 25:274–281. PMID: 29683234.

22. Sato T, Yoda T. Masticatory muscle tendon-aponeurosis hyperplasia: a new clinical entity of limited mouth opening. Jpn Dent Sci Rev. 2016; 52:41–48. PMID: 28408955.

23. Moroi A, Ueki K, Marukawa K, Okabe K, Mukouzawa A, Nakagawa K, et al. A case of masticatory muscle tendon-aponeurosis hyperplasia improved by mandibular anglectomy. Jpn J Oral Diagn. Oral Med. 2011; 24:188–194.
24. Yoshida H, Oshiro N, Fukuda A, Gamoh S, Shimizutani K, Morita S. A case of reformed coronoid process and mandibular angle after coronoidectomy and anglectomy for masticatory muscle tendon-aponeurosis hyperplasia. Oral Radiol. 2014; 30:129–133.

25. Sato T, Hayashi N, Enoki Y, Okubo M, Nakaoka C, Nakamoto N, et al. Limited mouth opening with a square mandible configuration: a case of masticatory muscle tendon-aponeurosis hyperplasia. J Surg Case Rep. 2015; 2015:rjv020. PMID: 25770956.

26. Nakamoto N, Sato T, Enoki T, Nakamoto A, Hori N, Fukushima Y, et al. Regeneration of tendon and aponeurosis after surgery of masticatory muscle tendon-aponeurosis hyperplasia: report of a case. J Jpn Soc TMJ. 2010; 22:158–162.
27. Hayashi N, Sato T, Fukushima Y, Takano A, Sakamoto I, Yoda T. A two-year follow-up of surgical and non-surgical treatments in patients with masticatory muscle tendon-aponeurosis hyperplasia. Int J Oral Maxillofac Surg. 2018; 47:199–204. PMID: 28823904.

Fig. 2
Three-dimensional computed tomography of MMTAH showing a small gonial angle and flattening of the mandibular plane. Both coronoid processes are thickened anteroposteriorly, but there is no contact between the coronoid process and the zygomatic arch on mouth opening. Adapted from the book of Yoda (Ishiyaku Publishers; 2012)13 with original copyright holder's permission.

Fig. 3
Horizontal section on magnetic resonance imaging (repetition time/echo time [TR/TE], 620.00/13.00) showing overhang of masseter muscle along the anterior border of the mandibular ramus and the aponeurosis as a black area on the outside and inside.
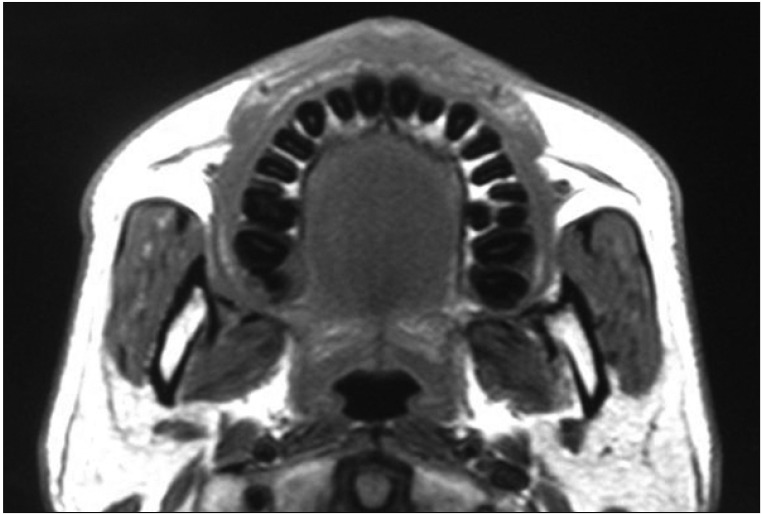
Fig. 4
A hard cord-like structure found along the anterior border of the masseter muscle on intraoral palpation.

Fig. 5
Optical microscopy findings (H&E staining) of the tendon tissue in masticatory muscle tendon-aponeurosis hyperplasia. The tendon fibers are normal.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download