2. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005; 83(3):457–502.

3. Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Millwood). 2010; 29(5):766–772.

4. Villani J, Mortensen K. Nonemergent emergency department use among patients with a usual source of care. J Am Board Fam Med. 2013; 26(6):680–691.

5. DeVoe JE, Tillotson CJ, Wallace LS, Lesko SE, Pandhi N. Is health insurance enough? A usual source of care may be more important to ensure a child receives preventive health counseling. Matern Child Health J. 2012; 16(2):306–315.

6. Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res. 2002; 37(6):1509–1529.

7. Bartman BA, Moy E, D'Angelo LJ. Access to ambulatory care for adolescents: the role of a usual source of care. J Health Care Poor Underserved. 1997; 8(2):214–226.

8. Devoe JE, Tillotson CJ, Wallace LS, Lesko SE, Angier H. The effects of health insurance and a usual source of care on a child's receipt of health care. J Pediatr Health Care. 2012; 26(5):e25–e35.

9. Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med. 1991; 114(4):325–331.

10. Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996; 86(12):1742–1747.

11. Pati S, Shea S, Rabinowitz D, Carrasquillo O. Health expenditures for privately insured adults enrolled in managed care gatekeeping vs indemnity plans. Am J Public Health. 2005; 95(2):286–291.

12. Meyer TJ, Prochazka AV, Hannaford M, Fryer GE. Randomized controlled trial of residents as gatekeepers. Arch Intern Med. 1996; 156(21):2483–2487.

13. Martin DP, Diehr P, Price KF, Richardson WC. Effect of a gatekeeper plan on health services use and charges: a randomized trial. Am J Public Health. 1989; 79(12):1628–1632.

14. Fullerton CA, Witt WP, Chow CM, Gokhale M, Walsh CE, Crable EL, et al. Impact of a usual source of care on health care use, spending, and quality among adults with mental health conditions. Adm Policy Ment Health. 2018; 45(3):462–471.

15. Ferris TG, Perrin JM, Manganello JA, Chang Y, Causino N, Blumenthal D. Switching to gatekeeping: changes in expenditures and utilization for children. Pediatrics. 2001; 108(2):283–290.

16. Gerdtham UG, Jönsson B, MacFarlan M, Oxley H. The determinants of health expenditure in the OECD countries: a pooled data analysis. Dev Health Econ Public Policy. 1998; 6:113–134.

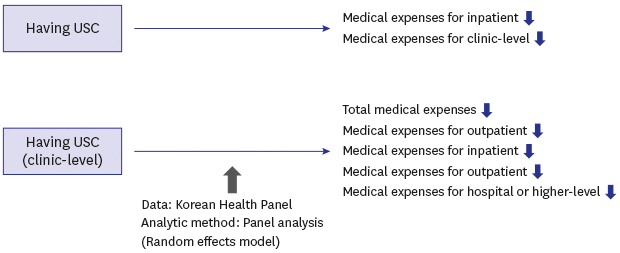
17. Yoon HJ, Choi JW, Lee SA, Park EC. Influence of usual source of care on outpatient visit and expense of hypertension patients. Korean J Hosp Manag. 2017; 22(1):1–9.
18. Chai YS, Lee JK, Park SS, Kim HJ, Kang IG, Kim GS, et al. Use of emergency medical services and characteristics of urgent and non-urgent adult patients according to the usual source of care: a Korea medical expenditure panel study. J Korean Soc Emerg Med. 2015; 26(2):129–137.
19. Lee SD, Shin E, Lim JY, Lee SG, Kim JM. Effects of usual source of care by patients with diabetes on use of medical service and medical expenses. Korean J Hosp Manag. 2017; 22(3):1–17.
20. Kim SJ. The Effect of USC on Medical Use and Medical Costs. In : The 6th Korea Health Panel Conference; Seoul: Korea Institute for Health and Social Affairs;2014.
21. Kim JY, Baek SM, Jeong TY. Difference in Differences Analysis of USC Effect. In : The 6th Korea Health Panel Conference; Seoul: Korea Institute for Health and Social Affairs;2014.
22. Pati S, Shea S, Rabinowitz D, Carrasquillo O. Does gatekeeping control costs for privately insured children? Findings from the 1996 medical expenditure panel survey. Pediatrics. 2003; 111(3):456–460.

23. Moon S, Choi M. The effect of usual source of care on the association of annual healthcare expenditure with patients' age and chronic disease duration. Int J Environ Res Public Health. 2018; 15(9):E1844.

24. Han JO, Kang KH, Yim J. The usual source of healthcare and frequent visits to emergency departments. Korean J Emerg Med Serv. 2017; 21(3):97–107.
25. Kuder JM, Levitz GS. Visits to the physician: an evaluation of the usual-source effect. Health Serv Res. 1985; 20(5):579–596.
26. Ettner SL. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health. 1996; 86(12):1748–1754.

27. Kim DR. The effect of having usual source of care on the choice among different types of medical facilities. Health Policy Manag. 2016; 26(3):195–206.

28. Lee JY, Jo MW, Yoo WS, Kim HJ, Eun SJ. Evidence of a broken healthcare delivery system in Korea: unnecessary hospital outpatient utilization among patients with a single chronic disease without complications. J Korean Med Sci. 2014; 29(12):1590–1596.

29. Hyun MK. Effect of work on medical expenditures by elderly: findings from the Korean health panel 2008–2013. Saf Health Work. 2018; 9(4):462–467.

30. Kang SH, Ju YJ, Yoon HJ, Lee SA, Kim W, Park EC. The relationship between catastrophic health expenditure and health-related quality of life. Int J Equity Health. 2018; 17(1):166.

31. Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen's behavioral model of health services use: a systematic review of studies from 1998–2011. Psychosoc Med. 2012; 9:Doc11.
32. de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003; 56(3):221–229.

33. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383.

34. Kim KM, Jeon H, Lee JH. Having a physician rather than a place as a usual source of care would be better: from 2012 Korea Health Panel Data. J Korean Med Sci. 2017; 32(1):4–12.
35. Sung NJ, Choi YJ, Lee JH. Primary care comprehensiveness can reduce emergency department visits and hospitalization in people with hypertension in South Korea. Int J Environ Res Public Health. 2018; 15(2):E272.

36. Martin DP, Diehr P, Price KF, Richardson WC. Effect of a gatekeeper plan on health services use and charges: a randomized trial. Am J Public Health. 1989; 79(12):1628–1632.

37. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32(5):718–728.

39. Clark TS, Linzer DA. Should I use fixed or random effects? Political Science Research and Methods. 2015; 3(2):399–408.

40. Organization for Economic Cooperation and Development, World Health Organization. Health at a Glance: Asia/Pacific 2018: Measuring Progress towards Universal Health Coverage. Paris: OECD publishing;2018.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download