Abstract
The effectiveness of dental implants in patients with disability, who are non-compliant during treatment, is controversial because of their poor oral health. Thus, oral health-care and management in such patients is concerning. Moreover, limited information is available on prognosis after implant placement. Herein, we describe a patient with schizophrenia who underwent dental implantation under multiple inductions of general anesthesia (5 times) and required conservative treatment and tooth extraction for multiple dental caries and retained roots because of inadequate oral health-care. Postoperatively, fracture of the prosthodontics and progression of dental caries were observed, and with 3 additional inductions of general anesthesia, conservative treatment, implant surgery, and prosthesis implantation were conducted. Postoperative 12-month follow-up since the last prosthesis implantation showed successful results. For patients with schizophrenia, multiple implantation can reduce horizontal bone loss and achieve aesthetic results compared to treatment with removable prosthodontics and could serve as an alternative treatment modality.
Removable prosthodontics are considered adequate to treat most tooth extraction cases among patients with disability having poor oral health-care. However, the attachment, detachment, and management of prothesis are difficult in patients with impaired posture maintenance or limb control [1]. Therefore, treatment with fixed prosthetic implants can save time and provide an aesthetic alternative.
Currently, the use of implant in general patients has a high success rate, with 90–95% long-term success rate [23]. However, implant treatment in patients with disability has limited application because of the lack of compliance and oral care [4]. And in 2011 Arnaiz et al. reported that schizophrenia patients had higher scores than the control group with respect to missing teeth [5]. But in 2017, Kim et al. reported that satisfactory results in 19 patients with mental disability with implant therapy [6]. Additional reports indicate that treatment with prosthetic implants may be considered in patients with inadequate oral health-care [7].
Herein, we present successful recovery of oral function after placement of additional implant, prosthesis, and conservative treatment of caries, since four years of performing an immediate implantation in a patient with schizophrenia.
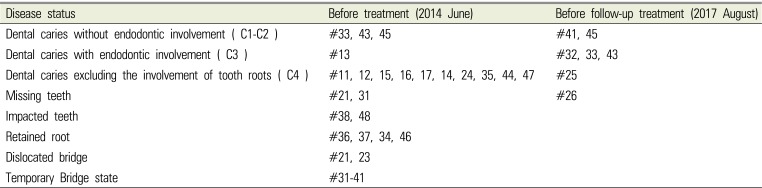
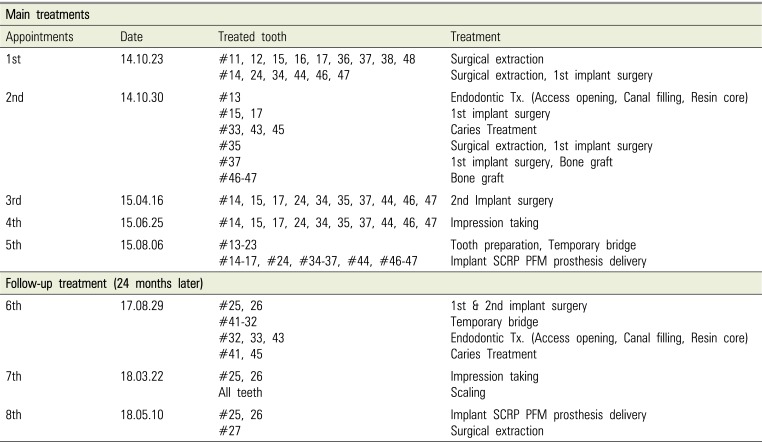
In June 2014, a 62-year-old male presented with a chief complaint of multiple dental caries. Underlying comorbidities included schizophrenia and hypothyroidism, and he took levothyroxine sodium (0.075 mg qd), clozapine (400 mg qd), lorazepam (0.5 mg bid), propranolol (40 mg bid), haloperidol (10 mg qd), and risperidone (4 mg qd). The patient was non-compliant toward treatment. A list of his dental problems is presented in Table 1.
Collaborative examination between the departments of prosthodontics, conservative dentistry, oral & maxillofacial surgery, and dental anesthesiology indicated that extraction of 15 teeth (#11, 12, 14, 15, 16, 17, 24, 34, 36, 37, 38, 44, 46, and 48) and treatment of caries in 4 teeth (#13, 33, 43, 45) were required; the treatment was scheduled to be performed under multiple rounds of general anesthesia (Fig. 1). At first examination, the use of a denture was indicated after tooth extraction. However, the patient's guardian asked for an implant; therefore, the treatment plan was revised to implant and prosthesis placement on following guardian's consent after explaining the advantages and disadvantages of the treatment, costs involved, and guardian's responsibility for postoperative oral health-care. In October 2014, under general anesthesia, the 15 indicated teeth were extracted and the immediate implantation of 6 implants on sites #14, 24 (4.0 * 10.0 mm), 34, 44 (4.5 * 10.0 mm), 46, and 47(5.0 * 8.5 mm) was conducted. After one week, the #35 tooth was extracted and four implants were placed at sites #15 (4.5 * 10.0 mm), 17 (4.5 * 8.5 mm), 35 (4.5 * 10.0 mm), and 37 (4.5 * 10.0 mm). Xenogenic bone grafting (Bio-Oss, Geistlich) was performed in the left and right mandibular molar tooth regions. Conservative treatment was performed for teeth #13, 33, 43, and 45. All the implants used OSSTEM TS III SA, and in two surgeries, 16 teeth were extracted and 10 implants were placed.
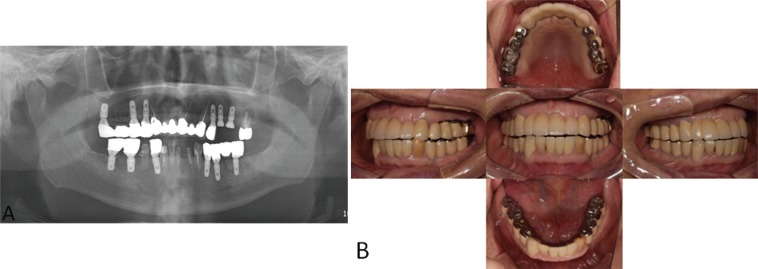
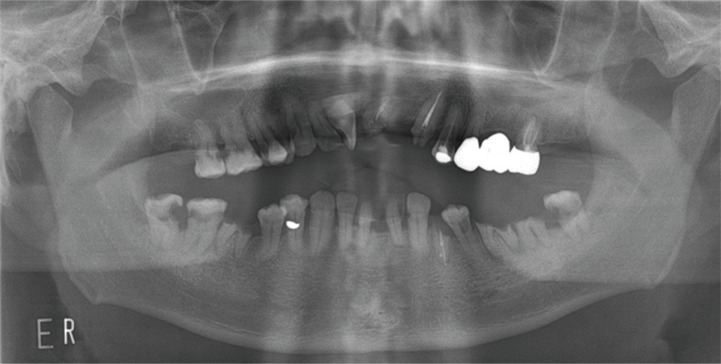
Six months after the first operation, a second operation was performed under general anesthesia in April 2015 (Fig. 2) and no unusual findings were observed [8]. Dental impressions were obtained in June 2015 and the screw-cement retained prosthesis (SCRP) porcelain fused metal (PFM) crown was implanted in August under general anesthesia. No complications presented besides screw retightening due to the detachment of the prosthetic implant in #24 in November 2015. The patient had good oral hygiene. At postoperative 24-month follow-up, severe caries was found at #25 tooth area, and in August 2017, the existing bridge was cut; #25 tooth was extracted, and two implants at sites #25 (4.0 * 8.5 mm) and #26 (4.5 * 8.5 mm) were placed (Fig. 3A). Conservative treatment was performed for teeth #32, 33, 41, 43, and 45. In March 2018, dental impression and full mouth scaling were procured under general anesthesia, and in May 2018, the SCRP PFM prosthesis was implanted at #25 and 26 under general anesthesia (Fig. 3B). Moreover, tooth #27 was extracted because of chronic periapical periodontitis. Continued follow-up and scaling were performed at the department of prosthesis, and the implants demonstrated successful retention without failure (June 27, 2019). The patient's oral condition before follow-up treatment is presented in Table 1. Information on the treatment procedures are shown in Table 2.
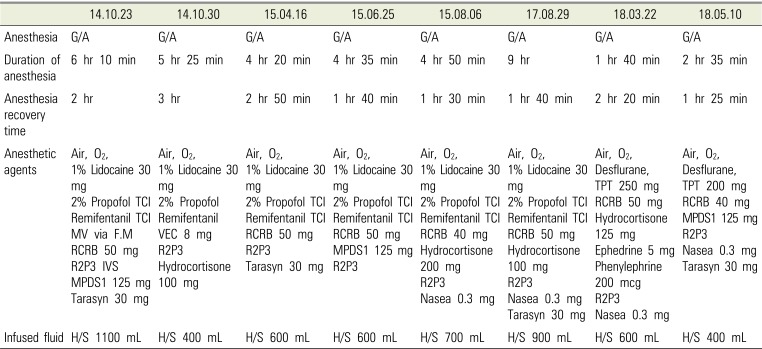
Preoperative electrocardiogram (ECG) before the induction of general anesthesia showed sinus rhythm with right bundle branch block. Chest radiograph was unremarkable with linear atelectasis at both the lower lung fields. Serum TSH and free T4 were 4.39 µIU/mL and 1.17 ng/dL, respectively. Other preoperative laboratory findings were normal.
We explained to the patient's guardian about the anesthesia procedure and case reports, and a written consent was obtained. The patient fasted for 8 hours on the day of induction of anesthesia, but the usual medication was instructed to be taken two hours before hospitalization. He had no premedication for general anesthesia. A 22-gage IV catheter was inserted into the upper arm and standard monitoring equipment (pulse oximetry, end-tidal CO2, ECG lead, and noninvasive blood pressure monitoring) and Bispectral index were used. After sufficient preoxygenation, general anesthesia was induced and maintained using the effect-site model with TCI of propofol in combination with (lidocaine 30 mg) and remifentanil. The target concentrations of propofol and remifentanil were set at 3 µg/mL and 3 ng/mL, respectively, during induction, and were maintained at 1–3 µg/mL and 1-–3 ng/mL, respectively, according to hemodynamic changes. After loss of eyelash reflex, a bolus dose of rocuronium (50 mg) was administered; nasotracheal intubation with an endotracheal tube (RAE cuffed; 7.0 mm) was performed with laryngoscope after 3 minutes. The patient was maintained on volume-controlled mechanical ventilation with O2/air mixture and tidal volume was 6–8 mL/kg. Respiratory rate was adjusted to maintain the end-tidal partial pressure of carbon-dioxide at 30–35 mmHg. Propofol and remifentanil infusions continued until completion of the procedure.
Intravenous pyridostigmine (15 mg), glycopyrrolate (0.4 mg), steroid, and antiemetics were administered postoperatively. Extubation was performed after establishment of regular spontaneous breathing pattern. The patient was transferred to the recovery room. In the recovery room, the patient showed stable vital signs. Oxygen was supplied at a flow rate of 6 L/min with a simple facial mask. After the first general anesthesia, because of extended recovery time, the patient was hospitalized and discharged the next day. However, for subsequent 7 instances of general anesthesia, the patient was discharged the same day. Information of eight general anesthesia is shown in Table 3.
Patients with schizophrenia experience delusions, hallucinations, behavioral disorders, speech disorders, and severe emotional changes. Schizophrenia is a neuropsychiatric disorder caused by dysfunctional dopaminergic activity [91011]. Patients on prolonged regimen of anti-schizophrenic medications have reduced biological response to stimuli, with increased risk of complications after general anesthesia due to the underlying diseases. Therefore, possibility of interaction between antipsychotics and anesthetics should be examined. Possible side effects of general anesthesia in patients with schizophrenia include arrhythmia, hypotension, tachycardia, prolonged anesthesia, seizure, confusion, and impaired thermoregulation. Therefore, pre- and postoperative continuation of antipsychotic medication, and dose reduction of anesthesia should be considered. And this patient need to undergo multiple inductions of general anesthesia; therefore, the withdrawal symptoms, possibility of recurrence, and postoperative delirium caused by drug discontinuation should be considered. Anesthetic precautions to prevent the occurrence of postoperative complications in patients is needed.
Compared to general population, patients with schizophrenia usually have poor dental hygiene [12]. Our patient initially had minor symptoms of schizophrenia, good oral care, and was compliant toward general dental treatment. And the patient's guardian was extremely cooperative and responsible toward the oral treatment and for the patient's oral health-care. After tooth extraction, the patient's condition was presumed to satisfy the following conditions: 1) Intact socket walls; 2) Facial bone wall at least 1 mm thick; 3) Thick soft tissue; 4) No acute infection at extracted site; and 5) Availability of the bone apical and palatal to the socket to provide primary stability [13]. Therefore, an immediate implantation after tooth extraction was decided. In November 2015, 30 months after first implant prosthesis placement, the panoramic images showed no abnormalities and no other clinically significant problem was found. In May 2018, 12 months after second implant prosthesis placement, good clinical outcomes were obtained.
In conclusion implants, rather than removable prosthodontics, may be favorable for aesthetically and predictably favorable outcomes in patients with schizophrenia treated under careful surgical plan with collaboration between oral and maxillofacial surgery, dental anesthesia, and prosthesis departments. Multiple implantations can be conducted without difficulty using this approach. In addition, the schizophrenic patients tended to limit the number of general anesthesia as much as possible, but in this case, multiple treatments were required due to the implant treatment. Nevertheless, we report a good result without complications in several general anesthesia.
References
1. Schou S, Holmstrup P, Hjørting-Hansen E, Lang NP. Plaque-induced marginal tissue reactions of osseointegrated oral implants: a review of the literature. Clin Oral Implants Res. 1992; 3:149–161. PMID: 1298429.
2. Arvidson K, Bystedt H, Frykholm A, von Konow L, Lothigius E. A 3-year clinical study of Astra dental implants in the treatment of edentulous mandibles. Int J Oral Maxillofac Implants. 1992; 7:321–329. PMID: 1289257.
3. Kim JH, Kim YK. Clinical study about the implant treatment in patients with systemic disease. Implantology. 2009; 13:64–75.
4. Gabre P, Martinsson T, Gahnberg L. Longitudinal study of dental caries, tooth mortality and interproximal bone loss in adults with intellectual disability. Eur J Oral Sci. 2001; 109:20–26. PMID: 11330930.

5. Arnaiz A, Zumárraga M, Díez-Altuna I, Uriarte JJ, Moro J, Pérez-Ansorena MA. Oral health and the symptoms of schizophrenia. Psychiatry Res. 2011; 188:24–28. PMID: 21055830.

6. Kim IH, Kuk TS, Park SY, Choi YS, Kim HJ, Seo KS. Prognosis following dental implant treatment under general anesthesia in patients with special needs. J Dent Anesth Pain Med. 2017; 17:205–213. PMID: 29090251.

7. Isaksson R, Becktor JP, Brown A, Laurizohn C, Isaksson S. Oral health and oral implant status in edentulous patients with implant-supported dental prostheses who are receiving long-term nursing care. Gerodontology. 2009; 26:245–249. PMID: 19555359.

8. Nam H, Sung KW, Kim MG, Lee K, Kwon D, Chi SI, et al. Immediate implant placement for schizophrenic patient with outpatient general anesthesia. J Dent Anesth Pain Med. 2015; 15:147–151. PMID: 28879272.

9. McCarthy MM, Ching S, Whittington MA, Kopell N. Dynamical changes in neurological diseases and anesthesia. Curr Opin Neurobiol. 2012; 22:693–703. PMID: 22446010.

10. Veenith T, Burnstein RM. Management of patients with neurological and psychiatric disorders. Surgery. 2010; 28:441–445.

11. Lieb K, Selim M. Preoperative evaluation of patients with neurological disease. Semin Neurol. 2008; 28:603–610. PMID: 19115168.

12. McCreadie R, Stevens H, Henderson J, Hall D, McCaul R, Filik R, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004; 110:306–310. PMID: 15352933.

13. Morton D, Chen ST, Martin WC, Levine RA, Buser D. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants. 2014; 29:216–220. PMID: 24660199.

Fig. 2
A: Panoramic view of the implant on 2nd operation (2015.04.16), B: Right maxillary and mandibular part, C: After the 2nd operation
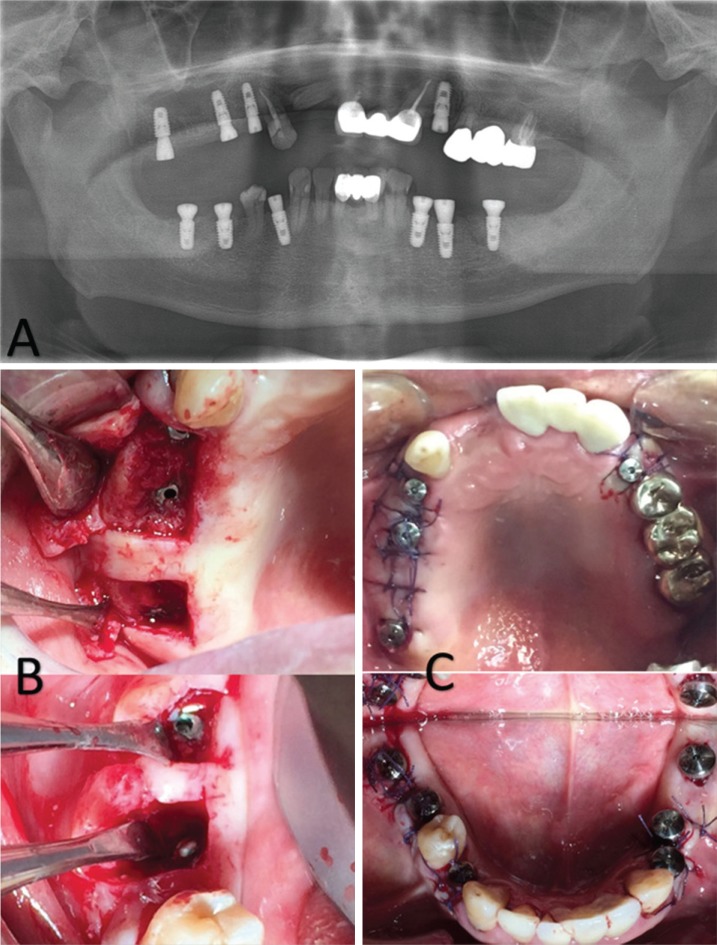
Fig. 3
A: Panoramic view of implant for tooth number #24, 25 (2017.09.14) B: Clinical photo of tooth number #24, 25 implant prosthesis delivery (2018.05.10)




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download