Abstract
Background
After tooth extraction, pain due to dry socket and pain in the adjacent tooth are common. The aim of this study was to retrospectively analyze pain in the adjacent tooth after surgical extraction of the mandibular third molar.
Methods
Postoperative pain due to dry socket, pain in the adjacent tooth, and pain from other causes were present. Group A included patents with dry socket alone; group B included patients with pain in the adjacent tooth alone; and group C included patients with both. The duration of symptoms was recorded. In addition, the prognosis of pain was divided into the complete improvement, improvement, maintenance, deterioration, and complete deterioration groups.
Results
A total of 312 mandibular third molars were extracted from 13, 60, and 10 patients in groups A, B, and C, respectively. The mean duration of symptoms was 5 days in group A and B and 15.2 days in group C. There were statistically significant differences in the duration of symptoms between groups A and C and groups B and C.
Conclusion
Pain in the adjacent tooth after third molar extraction can be caused by inflammatory reactions and pressure on this tooth. The pain caused by pressure on the periodontal ligament and alveolar bone results from the cytokines released by osteoclasts, which are responsible for bone destruction. However, pain from periodontal ligament damage caused by excessive pressure may be misunderstood as pulpal pain. Unconscious parafunctional habits, such as clenching and bruxism, could also be associated with post-extraction pain.
The most common cause of post-extraction pain is dry socket (localized osteitis). An extraction socket with an exposed bone, either whole or in part, is diagnosed as dry socket, and stimulation of this extraction socket induces sharp persistent pain and odor [1]. Another cause of post-extraction pain is hypersensitivity of the adjacent tooth [2345]. Pain in the adjacent tooth could be caused by injuries from the forces exerted during extraction, dislocation of large restorations, subluxations, and crown fractures [2345]. There have been a few studies on the clinical features and prognosis of pain associated with injuries of the adjacent tooth. The aim of this study was to analyze the clinical characteristics, prognoses, causes, and treatment of pain in the adjacent tooth after extraction of the third molars.
This study was performed from January 2015 to January 2016 including 312 healthy participants with American Society of Anesthesiologists physical status class 1 or 2, who underwent surgical removal of the mandibular third molars by an oral and maxillofacial surgery specialist at the Wonkwang University.
After the administration of local anesthetics (2% lidocaine containing a vasoconstrictor), an enveloped flap was raised. A surgical straight handpiece was used for bone removal and/or tooth separation. The indicated third molar was completely removed with minimal trauma to the adjacent second molar. After bone removal, an absorbable collagen sponge was inserted to prevent delayed postoperative bleeding, and one or two sutures were placed. In all patients, intraoperative pain was controlled with additional local anesthesia. After the surgery, first-generation cephalosporins and acetaminophen or tramadol analgesics were administered orally for three days. The postoperative instructions provided to the patients were: 1) bite on the gauze; 2) apply an ice pack immediately after the surgery; 3) re-visit on postoperative day 1 or 2 for dressing; and 4) re-visit for suture removal after one postoperative week.
At the follow-up, the patients were asked whether or not they had pain, and it was checked if pain was experienced upon probing of the extraction socket or the adjacent tooth. The patient was diagnosed with dry socket when the bone was exposed, either whole or in part. A hypersensitive response to percussion or mobility of the adjacent tooth (second molar) was examined to detect pain in the adjacent tooth.
Patients diagnosed with dry socket were treated conservatively until the pain disappeared. Patients with pain in the adjacent tooth were instructed to avoid biting with the opposing teeth while chewing and to control teeth clenching and bruxism. In addition, all patients were instructed to re-visit until the pain was relieved.
Patient data were retrospectively collected from medical records. Patients who did not attend more than one follow-up after surgical extraction of the mandibular third molar, such as the follow-up for dressing or suture removal, were excluded from the study.
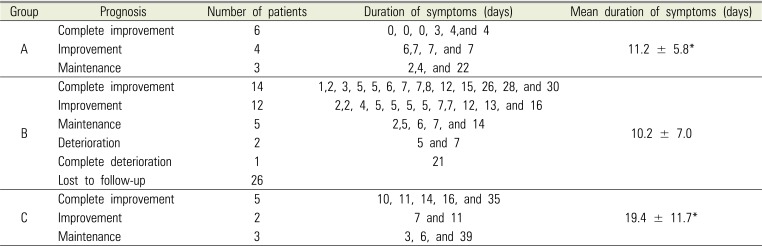
Based on the cause of pain, the patients were classified into groups A, B, and C and others. Group A included patients with dry socket alone; group B included patients with pain in the adjacent tooth alone; group C included patients with both dry socket and pain in the adjacent tooth (Fig. 1 and 2); others included patients with moderate pain but no bone exposure or pain in the adjacent tooth. In patients who attended more than two follow-ups, the duration of symptoms was recorded from the first episode (symptom onset) to the last episode. In addition, patients whose symptoms persisted for more than two days were categorized under the complete improvement, improvement, maintenance, deterioration, or complete deterioration group.
The study was approved by the Institutional Review Board (IRB) of the Wonkwang University Dental Hospital (IRB number: WKDIRB 201907-01) and was performed in accordance with relevant guidelines and regulations. The statistical significance was assessed at the 95% confidence level with a cross-analysis, an independent sample t-test, and a variance analysis to determine the differences in sex and age distribution and duration of symptoms among the groups.
A total of 312 mandibular third molars were extracted, of which 138 were on the left side and 174 were on the right side. There were 164 men and 148 women, with a mean age of 26.6 years (standard deviation: 10.9 years).
The age ranged from 13 to 76 years.
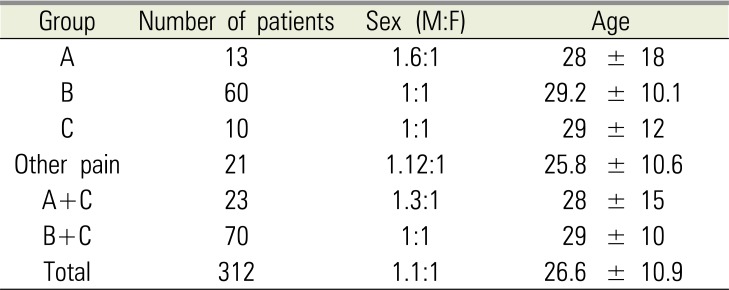
Table 1 shows the age and sex distribution of the patients based on the groups. A total of 104 patients complained of pain (33.3%) at the follow-up after surgical extraction, and after examination, 13, 60, 10, and 21 patients were categorized under groups A, B, C, and others, respectively (Fig. 1 and 2). The proportion of men in group A was higher than that in others, but the difference was not statistically significant.
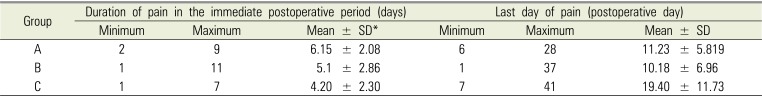
The mean duration of symptoms was 5 days in groups A and B and 15.2 days in group C. Among the patients in the complete improvement and improvement groups, the mean durations of symptoms in groups A, B, and C were 3.8, 9, and 29.7 days, respectively. There were statistically significant differences in the duration of symptoms between groups A and C and between groups B and C (Table 2 and 3).
An extraction socket with an exposed bone, either whole or in part, is diagnosed as dry socket, and stimulation of this extraction socket induces sharp persistent pain and odor [1]. However, pain develops gradually in the adjacent tooth and is occasionally progressive in severity. Pain in the adjacent tooth is often felt at night or on pressure application and is characteristically dull, continuous, and gradually progressive. It increases with percussion of the adjacent tooth (second molar) and may be moderate at rest but exacerbated on biting of the opposing teeth while chewing, teeth clenching, and bruxism. The bone pain described by Mercadante, et al. has the following similar characteristics: 1) gradual onset over weeks or months; 2) progressive intensity; 3) localization; 4) presentation at night or on occlusion; 5) dull and continuous in character; 6) associated with pressure in the area of involvement; 7) moderate on resting but exacerbated with body movements and postures, such as standing, walking, or sitting [6].
Pain in the adjacent tooth after extraction of a third molar could be caused largely by the inflammatory reaction after osteotomy and the pressure applied after the extraction.
The buccal bone is frequently removed during surgical extraction of the mandibular third molar, and in cases of extraction of a completely impacted tooth, the osteotomy is often extended to the buccal side of the second molar and is close to the periodontal ligament space of this tooth.
The periodontal ligament is densely innervated by free nerve endings [7], and therefore, is more sensitive to pain compared to the surrounding bone tissues. The healing process following tooth extraction with bone removal might be similar to the healing process following an indirect (secondary) fracture. Blood clots are formed; the inflammatory reaction begins; and the acute inflammatory response peaks within 24 hours and lasts for seven days [8]. At this time, tumor necrosis factor-α, interleukin (IL)-1, IL-6, IL-11, and IL-18 are released [9]; inflammatory cells are recruited; and angiogenesis is stimulated. These cytokines play a role in triggering pain or in lowering the pain threshold [10]. They may migrate to the periodontal ligament, which is located close to the osteotomy site, and contribute to pain in the adjacent tooth following the extraction, by lowering the pain threshold at the noxious free nerve endings in the periodontal ligament.
The effect of pressure on the adjacent tooth during and after extraction may be attributed analogously to occlusal trauma. Occlusal trauma is an injury of the teeth or their attachments from excessive occlusal forces [11]. The periodontal ligament consists of dense fibrous connective tissues, which attach and support the teeth to the alveolar bone [12]. Therefore, pain caused by application of pressure on teeth could be associated with the periodontal ligament [11]. Excessive occlusal forces may increase the degree of tooth movement and decrease the bone density [1314]. Moreover, they may affect the periodontal ligament and the alveolar bone [15].
Occlusal traumas can clinically present as tooth movements, fractures, migrations, sensitivity to extremes of temperature, wear facets, premature occlusal contacts, and pain on muscle palpation. Radiographically, alteration of the lamina dura, widening of the periodontal ligament space, evidence of root resorption, and bone loss may be observed [1617181920].
Frost first proposed a hypothesis in 1965 that bone changes in volume and structure in response to physical demands, such as application of pressure [21]. The theory of occlusal overload inducing bone resorption is supported by reports of the intracellular biological signaling process [22]. In the absence of pressure, disuse atrophy leads to bone resorption, and fatigue overloading of the bone also causes microfractures and resorption of the bone [2324].
Cytokines, such as bradykinin, prostaglandin, nerve growth factors, serotonin, adenosine triphosphate, and proton, which are released by osteoclasts to stimulate bone resorption, stimulate the nociceptors in the bone and periodontal ligament and cause bone pain [25]. Roqué M, et al. described the association between bone destruction and pain, stating that pain is the result of bone destruction, and progressive bone destruction increases the pain intensity [26].
In experimental animal models of trauma from occlusion, the density and size of the calcitonin gene-related peptide and substance P immunoreactive nerve increased locally in the gingiva, periodontal ligament, and pulp tissues. In addition, axonal proliferation and morphologic changes in the nerve appeared in the pulp tissues. Nerve reactions in the periodontal tissues were localized in the cervical and apical regions [27]. Thus, pain may be associated with damage to the periodontal ligament from pressure application, while it may be misunderstood as pulpal pain [12]. Postoperative endodontic examination for delayed or severe pain in the adjacent tooth revealed positive tooth vitality, excluding the adjacent teeth with preoperative caries with pulpal involvement (Fig. 3 and 4).
However, this study could not ascertain whether or not post-extraction pain was caused by the pressure applied during extraction. The proportion of patients who complained of pain in the adjacent tooth after extraction of the third molar was 22.4%. Most patients did not complain of pain after extraction. Although the possibility that the pain was caused by the pressure applied on the bone and the tooth adjacent to the mandibular third molar during extraction could not be completely excluded, the surgeon had taken special care during extraction to ensure that the extraction force was not exerted on the adjacent tooth by surgically dividing the third molar during the extraction. Furthermore, the pain can be caused by a single application of pressure and not by continuous pressure because the pain associated with bone resorption is moderate at rest and deteriorates with movement or pressure application [6].
The pain from periodontal ligament damage can be caused by persistent postoperative stress from biting on the gauze with more force than necessary to achieve hemostasis after extraction and from the forces exerted because of parafunctional habits, such as unconscious clenching and nighttime grinding, which can also contribute to alveolar bone loss [2829].
Pain after surgical removal of the mandibular third molar could originate from the periodontal ligament or from the bone of the adjacent tooth. Therefore, the patients' age, duration of pain, and prognosis could help in distinguishing this condition from dry socket. In this study, the differences in age among the patient groups were not statistically significant, but the time required for symptom relief was longer in group C (mean: 19.4 days) compared to group A (mean: 11.2 days).
In patients with pain in the adjacent tooth, the symptoms gradually improved after following the instructions of controlled chewing in the affected area and resolving the parafunctional habits. When symptoms persisted for over three weeks, periapical radiography was performed. However, bone resorption was not apparent in the periapical view in such cases (Fig. 3 and 4).
Pain in the adjacent tooth after extraction of the third molar can be improved by limiting the pressures applied on the affected tooth. Therefore, in patients who do not limit/control unconscious parafunctional habits, such as clenching and bruxism, the pain may not improve and may deteriorate. The effects of parafunctional habits on the prognosis of painful teeth should be investigated in future studies.
This study had several limitations. There was no control group with patients who did not receive instructions on mastication and parafunctional habits for relief of postoperative pain in the adjacent tooth. However, considering the retrospective nature of the study, it is clinically pertinent that such instructions were not omitted for any patient. Furthermore, for an alternative study design, comparing the clinical results among different surgeons was not pertinent because the criteria for the indication of extraction, surgical technique, and postoperative follow-up and management would be different.
Further studies with the use of the visual analog scale to quantify pain in the adjacent teeth and a prospective study design using pain records would contribute to the prevention and effective treatment of post-extraction pain.
ACKNOWLEDGMENTS
This study was supported by Wonkwang University in 2018. We would like to thank Editage (www.editage.co.kr) for English language editing.
References
1. Jüri K. Alling CC, Helfrick JF, Alling RD, editors. Impacted Teeth. 1st ed. Philadelphia: Saunders Co;1993. p. 371.
2. Haug RH, Perrott DH, Gonzalez ML, Talwar RM. The American Association of Oral and Maxillofacial Surgeons age-related third molar study. J Oral Maxillofac Surg. 2005; 63:1106–1114. PMID: 16094577.

3. Osborn TP, Frederickson G Jr, Small IA, Torgerson TS. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg. 1985; 43:767–769. PMID: 2995624.

4. Bouloux GF, Steed MB, Perciaccante VJ. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am. 2007; 19:117–128. PMID: 18088870.

5. Bui CH, Seldin EB, Dodson TD. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003; 61:1379–1389. PMID: 14663801.

6. Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. 1997; 69:1–18. PMID: 9060007.

7. Miki K, Honma S, Ebara S, Kumamoto K, Murakami S, Wakisaka S. Changes in the distribution of periodontal nerve fibers during dentition transition in the cat. PLoS One. 2015; 10:e0129826. PMID: 26083023.

8. Cho TJ, Gerstenfeld LC, Einhorn TA. Differential temporal expression of members of the transforming growth factor beta superfamily during murine fracture healing. J Bone Miner Res. 2002; 17:513–520. PMID: 11874242.
9. Gerstenfeld LC, Cullinane DM, Barnes GL, Graves DT, Einhorn TA. Fracture healing as a post-natal developmental process: molecular, spatial, and temporal aspects of its regulation. J Cell Biochem. 2003; 88:873–884. PMID: 12616527.

10. De Jongh RF, Vissers KC, Meert TF, Booij LH, De Deyne CS, Heylen RJ. The role of interleukin-6 in nociception and pain. Anesth Analg. 2003; 96:1096–1103. PMID: 12651667.

11. Ikeda T, Nakano M, Brando E, Suzuki A. The effect of traumatic occlusal contact on tooth pain threshold in humans. J Oral Rehabil. 1998; 25:589–595. PMID: 9781861.
12. Gulabivala K, Ng YL. Tooth organogenesis, morphology and physiology. Endodontics. 4th ed. St. Louis: Mosby;2014. p. 2–32.
13. Polson AM, Zander HA. Effect of periodontal trauma upon intrabony pockets. J Periodontol. 1983; 54:586–591. PMID: 6580411.

14. Lindhe J, Ericsson I. The influence of trauma from occlusion on reduced but healthy periodontal tissues in dogs. J Clin Periodontol. 1976; 3:110–122. PMID: 1064595.

15. Feller L, Khammissa RA, Schechter I, Thomadakis G, Fourie J, Lemmer J. Biological events in periodontal ligament and alveolar bone associated with application of orthodontic forces. ScientificWorldJournal. 2015; 2015:876509. PMID: 26421314.

16. Ramfjord SP, Ash MM Jr. Significance of occlusion in the etiology and treatment of early, moderate and advanced periodontitis. J Periodontol. 1981; 52:511–517. PMID: 6793705.

18. Glover ME. Occlusal therapy and its role in the etiology and treatment of periodontal diseases. Tex Dent J. 1988; 105:18–22.
19. Wank GS, Kroll YJ. Occlusal trauma. An evaluation of its relationship to periodontal prostheses. Dent Clin North Am. 1981; 25:511–532. PMID: 7021239.
20. Burgett FG. Trauma from occlusion. Periodontal concerns. Dent Clin North Am. 1995; 39:301–311. PMID: 7781828.
21. Hattner R, Epker BN, Frost HM. Suggested sequential mode of control of changes in cell behaviour in adult bone remodelling. Nature. 1965; 206:489–490. PMID: 5319106.

22. Hughes JM, Petit MA. Biological underpinning of Frost's mechanostat thresholds: The important role of osteocytes. J Musculoskelet Neuronal Interact. 2010; 10:128–135. PMID: 20516629.
23. Verborgt O, Gibson GJ, Schaffler MB. Loss of osteocyte integrity in association with microdamage and bone remodeling after fatigue in vivo. J Bone Miner Res. 2000; 15:60–67. PMID: 10646115.

24. Bentolila V, Boyce TM, Fyhrie DP, Drumb R, Skerry TM, Schaffler MB. Intracortical remodeling in adult rat long bones after fatigue loading. Bone. 1998; 23:275–281. PMID: 9737350.

25. Benemei S, Nicoletti P, Capone JG, Geppetti P. CGRP receptors in the control of pain and inflammation. Curr Opin Pharmacol. 2009; 9:9–14. PMID: 19157980.

26. Roqué M, Martinez MJ, Alonso P, Català E, Garcia JL, Ferrandiz M. Radioisotopes for metastatic bone pain. Cochrane Database Syst Rev. 2003; (4):CD003347. PMID: 14583970.

27. Kvinnsland I, Heyeraas KJ. Effect of traumatic occlusion on CGRP and SP immunoreactive nerve fibre morphology in rat molar pulp and periodontium. Histochemistry. 1992; 97:111–120. PMID: 1373126.

28. Waerhaug J. Pathogenesis of pocket formation in traumatic occlusion. J Periodontol. 1955; 26:107–118.

29. Roberts WE. Bone physiology, metabolism, and biomechanics in orthodontic practice. In : Graber TM, Vanarsdall RL, editors. Orthodontics: Current Principles and Techniques. 2nd ed. St Louis: Mosby;1994. p. 193–234.
Fig. 1
Classification of patients based on the cause of pain after surgical extraction of the mandibular third molar
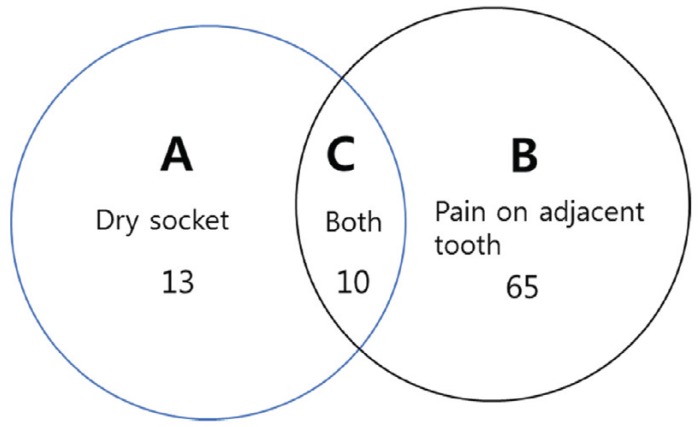
Fig. 2
The Consolidated Standards of Reporting Trials flow diagram for the cause and prognosis of pain after surgical extraction of the mandibular third molar. Abbreviations: CI = Complete improvement; I = improvement; M = maintenance; D = deterioration; CD = Complete deterioration
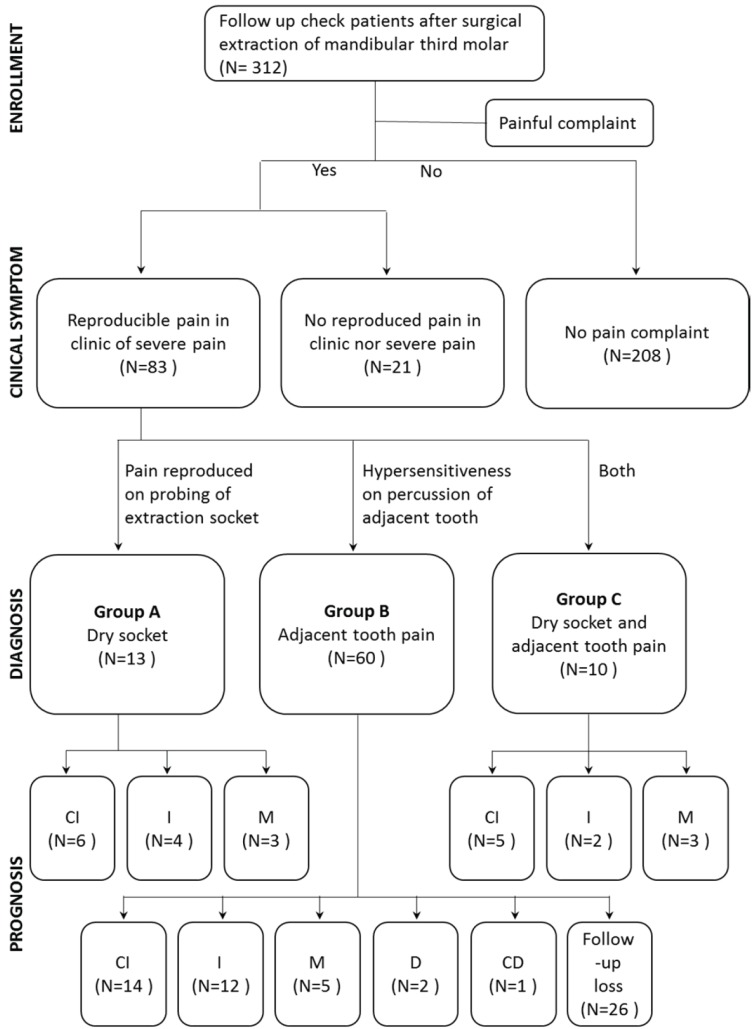
Fig. 3
Panoramic radiograph of a 45-year-old man from group B acquired before #48 extraction and periapical radiographs acquired simultaneously and three weeks after the extraction
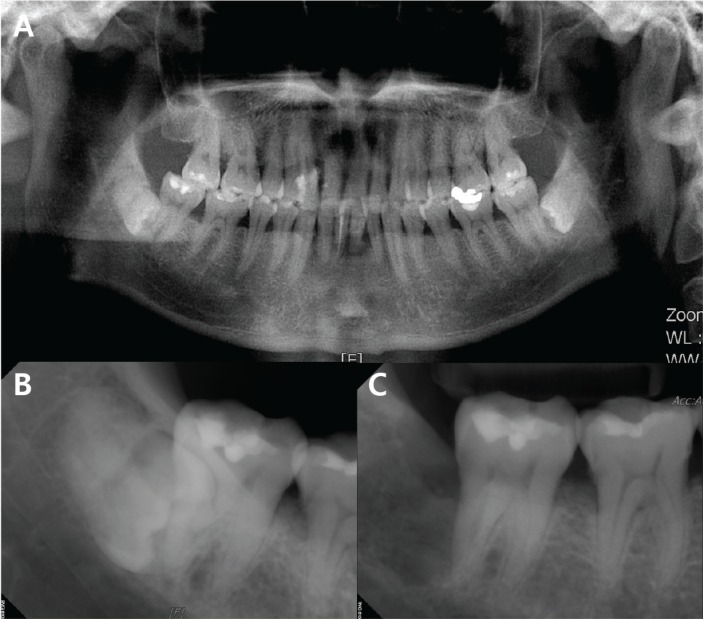
Fig. 4
Panoramic radiograph of a 27-year-old man from group C acquired before #38 extraction and periapical radiographs acquired simultaneously and eight weeks after the extraction because of persistent pain in the adjacent tooth (#37)
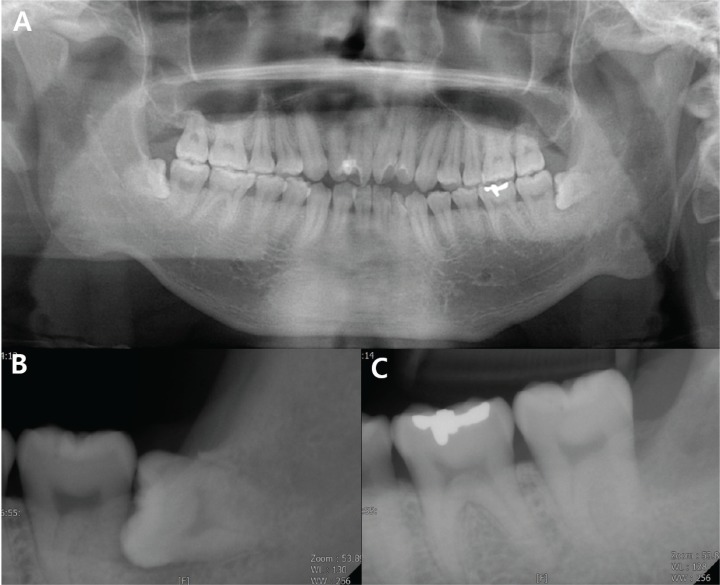
Table 1
Comparison of sex and age among patient groups classified based on the cause of pain after surgical extraction of the mandibular third molar




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download