Abstract
Purpose
We introduce our novel procedure for transvesicoscopic ureteral reimplantation using the Politano-Leadbetter technique (TVUR-PL). We describe the detailed surgical procedure and report operative outcomes.
Materials and Methods
We report a retrospective analysis of operative outcomes of TVUR-PL performed in children with vesicoureteral reflux (VUR) from January 2017 to July 2018. The analyzed operative outcomes included patient demographics, operative times, intra- and postoperative complications, indwelling duration of urethral Foley catheter, hospital length of stay, and treatment success.
Results
A total of 47 patients (17 males, 30 females) underwent TVUR-PL during the study period, including 18 unilateral and 29 bilateral cases (76 ureters). All operations were successfully completed without open conversion. The median operative time was 121 minutes for unilateral cases and 178 minutes for bilateral cases. The median duration of placement of a urethral Foley catheter was 2 days. There were no intra- or postoperative complications. Only one patient (1/47 patients, 2.1%), who had no postoperative VUR on voiding cystourethrography, experienced febrile urinary tract infection during the follow-up period.
Recent advances in small-diameter endoscopic, laparoscopic, and robotic techniques and the development of digital imaging techniques have led to the development of minimally invasive surgical procedures for the treatment of pediatric vesicoureteral reflux (VUR) [1]. Transvesicoscopic ureteral reimplantation (TVUR) is a method of filling the bladder with CO2 gas and inserting a camera and laparoscopic instruments into the bladder and performing a procedure to extend the length of the submucosal ureter in the same way as open transvesical ureteral reimplantation. To date, many surgeons have reported the results of TVURs, which are much less invasive than conventional open reimplantation but have similar success rates [234567891011121314151617]. However, most of the reported methods were of TVUR using Cohen's ureteral reimplantation technique (TVUR-Cohen) [23456789101112131617].
In this article, we introduce our novel TVUR operation using the Politano-Leadbetter technique (TVUR-PL) and report the operative outcomes. We also describe the detailed surgical procedure and highlight details that surgeons should be careful of in order to perform the operation successfully.
We retrospectively reviewed the operative outcomes of children with VUR who underwent TVUR-PL from January 2017 to July 2018. The initial treatment of all the children was continuous antibiotic prophylaxis and correction of bladder bowel dysfunction. Surgical correction was considered when the kidneys were at higher risk for renal deterioration such as in cases with high-grade VUR or recurrent febrile urinary tract infections (UTIs). A single surgeon performed all the procedures. Patients were followed with ultrasound at 1 and 6 months after ureteral reimplantation. Routine voiding cystourethrography (VCUG) was not checked if there was no postoperative febrile UTI. Patients who have less than a 6-month follow-up period were excluded from analysis. The analyzed operative outcomes included patient demographics, operative times, intra- and postoperative complications, urethral Foley catheter indwelling period, hospital length of stay, and clinical treatment success.
We used the following surgical equipment: an 8.5-Fr pediatric cystoscope, a 3-mm laparoscopic camera, three 3-mm laparoscopic trocars, 4-Fr ureteral stents, and 18-gauge spine needles (Fig. 1).
The surgical procedure was as follows (Supplementary material):
1. Patient position: The patient is prepared in the lithotomy position.
2. Pneumovesicum formation: The first hitch stitch is made under cystoscopic vision. When the bladder is fully filled with normal saline, it is punctured at the level of between the umbilicus and the pubic bone in the midline with an 18-gauge spinal needle with a loop of 3-0 Monocryl filament string. Another puncture is made with an 18-gauge spinal needle with a 3-0 Monocryl filament sting. The Monocryl filament is passed through the loop of Monocryl filament and the loop is pulled outside. The one Monocryl filament makes a hitch stich between the lower abdominal wall and the detrusor muscle, preventing air leaks during the transvesicoscopic surgery. After the first hitch stitch is securely made, a 3-mm laparoscopic camera trocar is inserted into the bladder. A 4-Fr ureteral stent is inserted into the refluxing ureter. Normal saline is suctioned and the bladder is filled with CO2 gas through the 3-mm laparoscopic trocar. The 3-mm laparoscopic camera is inserted. The second and third hitch stitches and lateral trocars are inserted under pneumovesicoscopic vision in a similar fashion.
3. Ureteral mobilization: A traction suture using 4-0 Vicryl is made just distally from the ureteral orifice in the 6 o'clock direction. Ureteral mobilization proceeds transvesicoscopically using a hook electrode and laparoscopic dissector. A gentle traction of the ureter facilitates the dissection. In male patients, caution should be taken to prevent injury to the vas deferens, which may be found during the dissection.
4. Submucosal tunnel formation: The dissection between the mucosal layer and the detrusor should be started at 2 to 3 cm (5 times the length of the ureteral caliber, 1:5 ratio) proximally from the original ureteral orifice. The dissection plane should be wide enough to freely pass the ureter between the mucosa and the detrusor.
5. Moving the ureter proximally: After opening the proximal hiatus, the ureter can be found though the opened window. Pulling the end of the ureter facilitates identification of the ureter through the window. When the ureter is found, it should be pulled out through the window and moved proximally as in the open Politano-Leadbetter ureteral reimplantation operation.
6. Closure of the original hiatus: The hiatus that was opened during ureteral mobilization at the position of the original ureteral orifice is closed with 4-0 Vicryl.
7. Interpositioning of the ureter between the submucosal tunnel.
8. Closure of the proximal defect.
9. Fixing suture between the ureteral orifice and the detrusor: After moving the ureter again from the proximal position to the original position between the mucosa and the detrusor plane, the ureteral orifice will be located at the original position. The ureteral orifice is fixed to the detrusor. The final ureteral course is natural.
Operative time was measured from the start of cystoscopy to skin closure for each case. Postoperative complications were categorized according to the Clavien grading system [18]. Clinical success was defined as the resolution of presenting indications for surgery.
A total of 47 patients (17 males, 30 females) underwent TVUR-PL during the study period, including 18 unilateral (9 right and 9 left) and 29 bilateral cases. All patients had recurrent febrile UTIs; the median number of preoperative febrile UTIs was 2.5 (range, 1–8) (Table 1).
All operations were successfully completed without open conversion. The median operative time was 121 minutes for unilateral cases and 178 minutes for bilateral cases. The median duration of urethral Foley catheter placement was 2 days. There were no intra- or postoperative complications. Only one patient (1/47 patients, 2.1%) experienced a febrile UTI during the follow-up period. The patient was a 6-year-old girl who had left grade IV VUR combined with neurogenic bladder caused by lipomeningomyelocele. She had previously undergone a dextranomer/hyaluronic acid (DX/ HA) copolymer (Deflux®; Q-Med Scandinavia, Uppsala, Sweden) injection but underwent TVUR-PL again for recurrence of VUR. There was no VUR when we checked VCUG after treatment of her febrile UTI (Table 2).
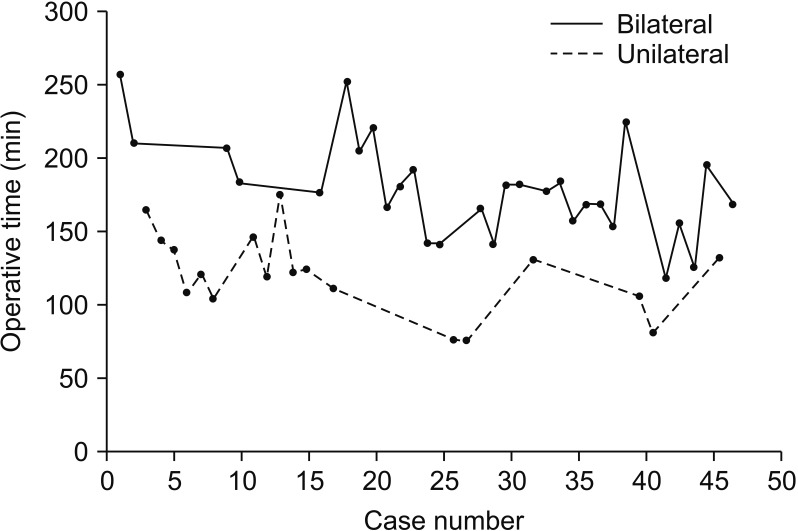
The operative time decreased with increasing case numbers. The average operative time for the last 5 cases was significantly shorter (105 minutes for unilateral cases and 152 minutes for bilateral cases, p<0.05) than that for the first 5 cases (135 minutes for unilateral cases and 207 minutes for bilateral cases, p<0.05) except for complexed cases (previous Deflux injection or VUR with neurogenic bladder) (Fig. 2).
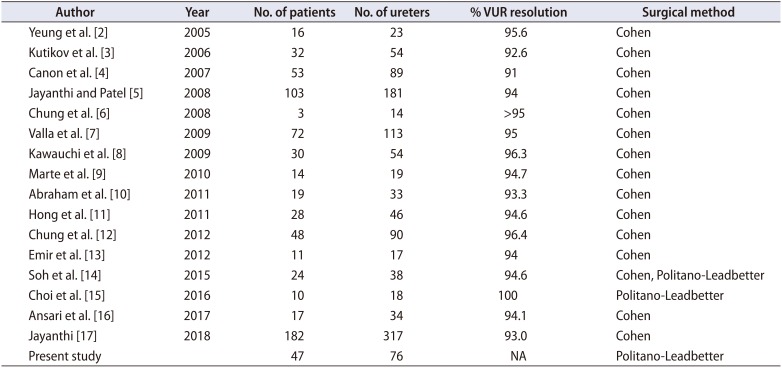
Since TVUR was first introduced in 2005, it has been gaining popularity as a minimally invasive surgical treatment option for VUR [234567891011121314151617]. Until now, most of the reported TVUR procedures have been based on the Cohen technique, a method of creating a cross-trigonal submucosal tunnel, which has the disadvantage that the direction of the ureter after the operation is not natural (Table 3) [234567891011121314151617].
Politano-Leadbetter ureteral reimplantation is a popular technique for open transvesical anti-reflux surgery in which the ureteral course remains natural after the operation [19]. This surgical technique has been employed in TVUR by only a few surgeons until now [1415], and our surgical method was developed by referring to their techniques.
The first report about TVUR-PL was published by Soh et al. in 2015 [14]. Even though our method was modified from their surgical method, our method has several advantages over theirs. First, Soh et al. [14] inserted a cystoscope through the original hiatus and monitored the structure of the outer bladder wall with the cystoscope to safely separate the ureter from the connective tissue around the posterior bladder wall and to move the ureter through the newly created proximal hiatus. This procedure requires not only 2 monitors to monitor the laparoscope and the cystoscope, but also a surgeon in the laparoscopic field and another surgeon to perform cystoscopy. We found the mobilized ureter directly through the window of the new hiatus without cystoscopy and moved it proximally. Thus, our operative procedure is much simpler than their method. Second, they inserted the additional trocar through the urethra, and inserted a miniature dissector trough this trocar and used the dissector to make the submucosal tunnel from the caudal to the cephalad direction. Because it is impossible to insert a trocar through the male urethra, their TVUR-PL surgical technique was performed in female patients only. In contrast, we proceeded to create a submucosal tunnel from the cephalad to the caudal direction by using only the existing lateral trocars without inserting an additional trocar through the urethra. Because we did not insert an additional trocar through the urethra, our operation could be performed in male patients as well as in female patients.
Choi et al. [15] reported another TVUR-PL technique that includes the surgical procedure of moving the mobilized ureter to the new hiatus by cutting the detrusor between the original hiatus and the new hiatus, moving the ureter through the incised detrusor, and then suturing the detrusor again. This technique has the potential to induce postoperative edema and inflammation of the detrusor due to the incision and reattachment of the detrusor, so that the urethral Foley catheter should be inserted for a sufficient period of time in order to restore the bladder. The average duration of Foley catheter indwelling was 5.1 days in their report. By contrast, our surgical method allows us to find the ureter directly through the new hiatus and move it proximally. Therefore, it is advantageous to not unnecessarily cut and resuture the detrusor. The maintenance period of the Foley catheter was as short as 1 to 2 days after the operation.
Our TVUR-PL surgical procedure has some advantages and disadvantages compared with the TVUR-Cohen technique. The advantages are as follows. First, our surgical approach allows us to maintain the natural direction of the ureter after surgery. Maintaining the direction of the natural ureter is advantageous when the child is subsequently subjected to urologic procedures such as ureteroscopic surgery or ureteral catheterization. Second, our surgical procedure makes it easy to create a submucosal tunnel. In the conventional TVUR-Cohen procedure, the process of making the submucosal tunnel is performed by using an instrument through the lateral trocars, so dissection between the mucosal and detrusor layers is somewhat blind because it is difficult to observe the dissection plane through the laparoscopic camera located in the midline. In contrast, using our surgical method, the direction of making the submucosal tunnel is from the new hiatus to the original hiatus. Therefore, the dissection plane can be observed under the magnified field of view from the laparoscopic camera. Thus, the dissection plane of the detrusor and mucosal layers can be separated easily and stably. Third, our surgical method makes it possible to secure a more stable submucosal tunnel length when the VUR is associated with urinary tract anomalies such as ureterocele or hutch diverticulum, which involve bladder trigone. Whereas the length of the submucosal tunnel in the cross-trigonal direction is limited, the posterior wall of the bladder is wide enough so that the Politano-Leadbetter procedure allows a sufficient submucosal tunnel. If necessary, the length of the submucosal tunnel can be increased by further submucosal dissection to the bladder neck, in other words, adding a Glenn-Anderson procedure. The disadvantage of our operation is that the surgical procedure is more complicated than the conventional TVUR-Cohen procedure. Our TVUR-PL procedure requires making a new hiatus and moving the ureter through the hiatus. Therefore, the number of laparoscopic sutures is increased and the operative time is longer than for the TVUR-Cohen procedure. Another issue is potential peritoneal tearing. Peritoneal tearing is possible during the process of making a proximal new hiatus during the TVUR-PL operation. If peritoneal tearing occurs, CO2 gas moves into the peritoneal cavity and compresses the bladder from the outside, which makes it difficult to maintain pneumovesicum.
In our analysis of the learning curve, the mean time for the operation was 135 minutes for unilateral reimplantation and 207 minutes for bilateral reimplantation for each of the first 5 cases. However, the operative time was 105 minutes for unilateral cases and 152 minutes for bilateral reimplantation for each of the last 5 cases. In the early stage of surgical experience, it took a long time to find the ureter through the newly opened hiatus and to move the ureter proximally. As the number of operations increased, the time required for this procedure was reduced.
Following are tips for surgeons planning to perform the TVUR-PL procedure to overcome the challenges that may be encountered. First, if the patient undergoing surgery is a young child with a small bladder, the lateral port should be inserted at a more superiomedial position. This port placement facilitates ureteral mobilization by moving the laparoscopic instrument away from the ureteral orifice. Second, it is better to begin the separation of the proximal mucosa and the bladder muscle sufficiently wide to reduce the occurrence of mucosal tearing while making the mucosal tunnel. Widening the starting dissection site can reduce the tension on the mucous membrane and reduce the risk of tearing. Third, to prevent the peritoneal tearing that may occur during the opening of the new hiatus, the detrusor should be opened gradually layer by layer. If the full layer of the detrusor is open at some point, opening the rest of the detrusor based on the layer of the open point can prevent peritoneal tearing. Fourth, the ureter can be more easily found by making the hiatus hole slightly larger in the process of finding the ureter through the new hiatus. Even if the size of the new hiatus hole is large, there is no serious air leak to make the operation difficult. Also, even if the size of the hole is large, it does not matter if the hole is sutured later. If it is difficult to locate the ureter directly beneath the open site, it is helpful to locate the ureter as it progresses through the laparoscopic field in the direction of the original ureteral orifice. This is because, even after the ureter has been mobilized, the ureter's movement range around the ureteral orifice is narrow and is located at that site.
A weakness of our study is that we did not perform postoperative VCUG for follow-up imaging. However, most of the patients (97.9%) had no postoperative febrile UTI, which suggests that the purpose of the anti-reflux operation was achieved from the viewpoint of clinical success. The TVUR procedure reproduces the open ureteral reimplantation technique in a similar way under laparoscopy. Therefore, the mechanism of eliminating the reflux is the same as for open ureteral reimplantation. After open ureteral reimplantation, the possibility of reflux is very high and the postoperative VCUG test may be omitted [20]. The various TVUR operations reported so far have reported postoperative radiologic success rates of 93% to 100% [234567891011121314151617], which is similar to the success rate of open ureteral reimplantation. Therefore, we think that the radiologic success of our TVUR-PL operation is very high when we assume that febrile UTI did not occur in all patients after our operation.
Our novel TVUR-PL operation is a safe and effective minimally invasive surgical treatment option for children with VUR. The main advantage of our new operation over the previously reported TVUR-Cohen operation is that our surgical approach allows us to maintain the natural direction of the ureter after surgery and makes it easier to create the submucosal tunnel.
References
1. Baek M, Kim KD. Current surgical management of vesicoureteral reflux. Korean J Urol. 2013; 54:732–737. PMID: 24255753.

2. Yeung CK, Sihoe JD, Borzi PA. Endoscopic cross-trigonal ureteral reimplantation under carbon dioxide bladder insufflation: a novel technique. J Endourol. 2005; 19:295–299. PMID: 15865516.

3. Kutikov A, Guzzo TJ, Canter DJ, Casale P. Initial experience with laparoscopic transvesical ureteral reimplantation at the Children's Hospital of Philadelphia. J Urol. 2006; 176:2222–2225. discussion 2225-6. PMID: 17070297.

4. Canon SJ, Jayanthi VR, Patel AS. Vesicoscopic cross-trigonal ureteral reimplantation: a minimally invasive option for repair of vesicoureteral reflux. J Urol. 2007; 178:269–273. discussion 273. PMID: 17499791.

5. Jayanthi V, Patel A. Vesicoscopic ureteral reimplantation: a minimally invasive technique for the definitive repair of vesicoureteral reflux. Adv Urol. 2008; 973616. PMID: 19009038.

6. Chung PH, Tang DY, Wong KK, Yip PK, Tam PK. Comparing open and pneumovesical approach for ureteric reimplantation in pediatric patients--a preliminary review. J Pediatr Surg. 2008; 43:2246–2249. PMID: 19040945.

7. Valla JS, Steyaert H, Griffin SJ, Lauron J, Fragoso AC, Arnaud P, et al. Transvesicoscopic Cohen ureteric reimplantation for vesicoureteral reflux in children: a single-centre 5-year experience. J Pediatr Urol. 2009; 5:466–471. PMID: 19428305.

8. Kawauchi A, Naitoh Y, Soh J, Hirahara N, Okihara K, Miki T. Transvesical laparoscopic cross-trigonal ureteral reimplantation for correction of vesicoureteral reflux: initial experience and comparisons between adult and pediatric cases. J Endourol. 2009; 23:1875–1878. PMID: 19619062.

9. Marte A, Sabatino MD, Borrelli M, Nino F, Prezioso M, Pintozzi L, et al. Pneumovesicoscopic correction of primary vesicoureteral reflux (VUR) in children. Our experience. Eur J Pediatr Surg. 2010; 20:366–370. PMID: 20954105.

10. Abraham MK, Viswanath N, Bindu S, Kedari P, Ramakrishnan P, Naaz A, et al. A simple and safe technique for trocar positioning in vesicoscopic ureteric reimplantation. Pediatr Surg Int. 2011; 27:1223–1226. PMID: 21853299.

11. Hong CH, Kim JH, Jung HJ, Im YJ, Han SW. Single-surgeon experience with transvesicoscopic ureteral reimplantation in children with vesicoureteral reflux. Urology. 2011; 77:1465–1469. PMID: 21333340.

12. Chung MS, Han SW, Jung HJ, Im YJ, Han HH, Na JC, et al. Transvesicoscopic ureteral reimplantation in children with bilateral vesicoureteral reflux: surgical technique and results. J Laparoendosc Adv Surg Tech A. 2012; 22:295–300. PMID: 22356205.

13. Emir H, Mammadov E, Elicevik M, Buyukunal C, Soylet Y. Transvesicoscopic cross-trigonal ureteroneocystostomy in children: a single-center experience. J Pediatr Urol. 2012; 8:83–86. PMID: 21084225.

14. Soh S, Kobori Y, Shin T, Suzuki K, Iwahata T, Sadaoka Y, et al. Transvesicoscopic ureteral reimplantation: Politano-Leadbetter versus Cohen technique. Int J Urol. 2015; 22:394–399. PMID: 25754455.

15. Choi H, Park JY, Bae JH. Initial experiences of laparoscopic intravesical detrusorraphy using the Politano-Leadbetter technique. J Pediatr Urol. 2016; 12:110.e1–110.e7. PMID: 26750185.

16. Ansari MS, Yadav P, Arora S, Singh P, Sekhon V. Bilateral transvesicoscopic cross-trigonal ureteric reimplantation in children: surgical subtleties and a prospective summary. Urology. 2017; 101:67–72. PMID: 27890685.

17. Jayanthi VR. Vesicoscopic cross-trigonal ureteral reimplantation: high success rate for elimination of primary reflux. J Pediatr Urol. 2018; 14:324.e1–324.e5. PMID: 29748123.

18. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.
19. Politano VA, Leadbetter WF. An operative technique for the correction of vesicoureteral reflux. J Urol. 1958; 79:932–941. PMID: 13539988.

20. El-Ghoneimi A, Odet E, Lamer S, Baudouin V, Lottmann H, Aigrain Y. Cystography after the Cohen ureterovesical reimplantation: is it necessary at a training center? J Urol. 1999; 162:1201–1202. PMID: 10458466.

SUPPLEMENTARY MATERIAL
Accompanying video can be found in the ‘Urology in Motion’ section of the journal homepage (https://www.icurology.org). The supplementary video clip can also be accessed by scanning a QR code, and will be available on YouTube: https://youtu.be/aDNx2salIvY.
Table 1
Patient demographics
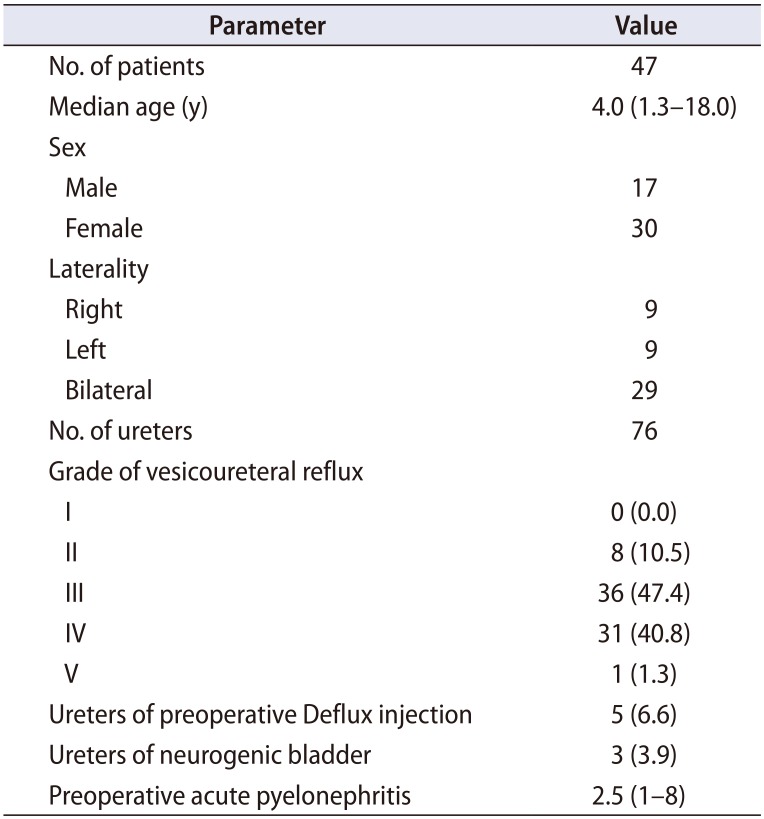
Table 2
Operative and postoperative parameters
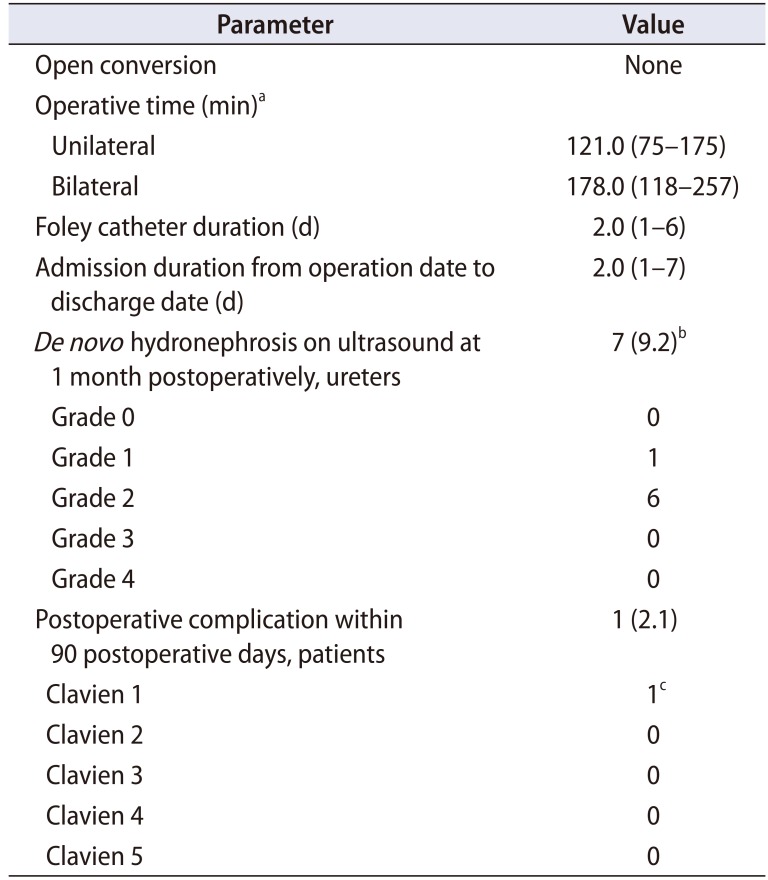
Values are presented as median (range), number (%), or number only.
a:Operative time was measured from the start of cystoscopy to skin closure for each case.
b:All de novo hydronephrosis resolved on ultrasound at 6 months postoperatively.
c:Postoperative febrile urinary tract infection occurred in one patient who had neurogenic bladder caused by lipomeningomyelocele.
Table 3
Review of the literature of surgical outcomes of pneumovesicoscopic ureteral reimplantation in children with vesicoureteral reflux
| Author | Year | No. of patients | No. of ureters | % VUR resolution | Surgical method |
|---|---|---|---|---|---|
| Yeung et al. [2] | 2005 | 16 | 23 | 95.6 | Cohen |
| Kutikov et al. [3] | 2006 | 32 | 54 | 92.6 | Cohen |
| Canon et al. [4] | 2007 | 53 | 89 | 91 | Cohen |
| Jayanthi and Patel [5] | 2008 | 103 | 181 | 94 | Cohen |
| Chung et al. [6] | 2008 | 03 | 14 | >95 | Cohen |
| Valla et al. [7] | 2009 | 72 | 113 | 95 | Cohen |
| Kawauchi et al. [8] | 2009 | 30 | 54 | 96.3 | Cohen |
| Marte et al. [9] | 2010 | 14 | 19 | 94.7 | Cohen |
| Abraham et al. [10] | 2011 | 19 | 33 | 93.3 | Cohen |
| Hong et al. [11] | 2011 | 28 | 46 | 94.6 | Cohen |
| Chung et al. [12] | 2012 | 48 | 90 | 96.4 | Cohen |
| Emir et al. [13] | 2012 | 11 | 17 | 94 | Cohen |
| Soh et al. [14] | 2015 | 24 | 38 | 94.6 | Cohen, Politano-Leadbetter |
| Choi et al. [15] | 2016 | 10 | 18 | 100 | Politano-Leadbetter |
| Ansari et al. [16] | 2017 | 17 | 34 | 94.1 | Cohen |
| Jayanthi [17] | 2018 | 182 | 317 | 93.0 | Cohen |
| Present study | 47 | 76 | NA | Politano-Leadbetter |




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download