This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To evaluate de novo and resolved urgency and urgency urinary incontinence (UUI) after midurethral sling operations in patients with stress urinary incontinence (SUI) and mixed urinary incontinence (MUI).
Materials and Methods
Patients who underwent midurethral sling operations because of SUI and MUI between January 2012 and December 2016 were reviewed. Patients were divided into three groups (pure SUI, SUI with urgency, and MUI). Patients with MUI were subcategorized as SUI predominant, equivalent, and UUI predominant. Postoperative de novo, persistent or disappearance of urgency or UUI were compared.
Results
A total of 334 patients were included: 76 with pure SUI, 78 with SUI with urgency, and 180 with MUI. In the MUI group, 138 patients were SUI predominant, 12 patients were equivalent, and 30 patients were UUI predominant. De novo urgency developed in 5 patients (6.6%) in the pure SUI group. In the SUI with urgency group, 51 patients (65.4%) became urgency-free, and 3 (3.8%) developed de novo UUI. UUI resolved in 135 patients (75.0%): 110 (79.7%) in the SUI-predominant group, 9 (75.0%) in the equivalent group, and 16 (53.3%) in the UUI-predominant group. The patients' preoperative perception of predominant UUI was the predictive factor for persistent UUI in the multivariate analysis (hazard ratio, 5.722; p=0.001).
Conclusions
De novo urgency and UUI developed in a relatively small number of patients after a midurethral sling operation. The resolution rate of UUI was significantly low in patients who had previous pelvic surgery or who preoperatively perceived UUI as a more bothersome symptom.
Go to :

Keywords: Suburethral slings, Urinary incontinence, Urinary incontinence, urge
INTRODUCTION
Stress urinary incontinence (SUI) is a common type of urinary incontinence in women. The prevalence of SUI is age dependent, ranging from 29% to 75% [
1]. Various surgical options are available for the correction of SUI, and the midurethral sling is currently the mainstay of treatment of female SUI owing to its efficacy and low complication rate [
2]. However, several kinds of storage symptoms, including frequency, urgency, and urgency urinary incontinence (UUI), can accompany SUI. In fact, mixed urinary incontinence (MUI), which is the coexistence of SUI and UUI, is also frequently observed in incontinent patients [
3]. The severity of SUI and UUI varies among patients with MUI; some patients may present with predominant SUI or UUI, whereas others may have an equivalent degree of SUI or UUI symptoms. Regardless of the predominant symptom, both SUI and MUI can result in significant deterioration in a patient's quality of life [
4].
Surgical correction of SUI can improve concurrent overactive bladder (OAB) symptoms such as urgency and UUI [
5]. Alternatively,
de novo urgency and UUI are observed in some patients with no previous evidence of storage symptoms after anti-incontinence surgery [
6]. However, the pathophysiology of improved OAB symptoms in MUI and the risk factors for
de novo OAB symptoms after sling operations are unclear [
7]. In addition, the exact resolution rate of MUI and the prevalence of
de novo OAB vary among studies. Successful correction of SUI is the primary end point of anti-incontinence surgery; however, adequate information regarding complications and changes in OAB symptoms is crucial as both are principal reasons for decreased patient satisfaction.
The optimal timing for the diagnosis and treatment of OAB symptoms after a sling operation might be controversial. The prevalence of OAB increases with aging, and it is almost impossible for clinicians to simply observe symptoms in real clinical settings. Treatment should be initiated at a certain point to improve both the patients' symptoms and their quality of life. In our previous study, we observed perioperative urgency for 1 year to identify the optimal time at which to commence further treatment after placement of transobturator tension-free vaginal tape. Patients' OAB symptoms became stationary after a certain period. We recommended treatment of OAB if urgency was noted at 1 month postoperatively in patients with preexisting urgency and after 6 months in those without preoperative urgency [
8].
In the present study, we primarily aimed to assess the prevalence and severity of de novo or resolved urgency and UUI after midurethral sling surgery. Secondly, we attempted to determine the predictive factors for postoperative de novo urgency and UUI in SUI, and persistent UUI in MUI.
Go to :

MATERIALS AND METHODS
Patients who underwent a midurethral sling operation for SUI by a single surgeon at a single tertiary center between January 2012 and December 2016 were screened. The following patients were excluded: 1) those with neurogenic bladder, for example, a history of cerebrovascular accident, Parkinson disease, or spinal cord injury; 2) those with previous anti-incontinence surgery; and 3) those who underwent concurrent repair of pelvic organ prolapse. We reviewed the patients' baseline demographics, preoperative urodynamic data, and perioperative medical records.
Preoperatively, patients underwent a thorough history taking, completed a 1-hour pad test, and were required to fill out a 3-day voiding diary. Our voiding diary includes the patient perception of intensity of urgency scale (PPIUS) [
9] and a 5-point urgency scale (0–4) that patients checked for each voiding. Urgency was defined as greater than or equal to grade 2 and UUI was defined as PPIUS grade 4. Urodynamic study was performed in all patients for insurance coverage of the anti-incontinence operation in the country. In patients with MUI, the patients were asked which symptom was subjectively more bothersome (SUI vs. UUI). In patients with subjectively dominant UUI, we considered behavioral and medical therapy first. The sling operation was performed when UUI was well-controlled or when patients were eager for primary correction of SUI. All patients underwent transobturator outside-in suburethral mesh insertion under monitored anesthesia care or general anesthesia.
Routine postoperative visits were scheduled at 1 week, 2 months, 6 months, and 1 year after the operation for patients with pure SUI. However, in the case of patients with preoperative OAB symptoms, shorter follow-up at postoperative 1 month was recommended. At each postoperative visit, all patients underwent uroflowmetry and a detailed interview with the surgeon regarding their subjective voiding symptoms (SUI, urgency, and UUI) and were recommended to submit a 3-day voiding diary to assess the presence of urgency and UUI objectively. In the case of discrepancy between subjective symptoms and the voiding diary, comprehensive discussion with patients was done to clarify the exact voiding symptoms.
On the basis of their initial symptoms, we divided the patients into three groups: those with pure SUI, SUI with urgency, and MUI. Patients with MUI were subcategorized as SUI predominant, equivalent (SUI=UUI), and UUI predominant. Prevalence and risk factors of de novo or resolved urgency and UUI were analyzed in each group. De novo or persistent urgency and UUI were assessed between 1 and 12 months postoperatively right before initiation or resumption of OAB treatment.
1. Statistical analysis
Statistical analysis was performed by using IBM SPSS statistics software, version 21.0 (IBM Corp., Armonk, NY, USA). Results were considered significant if the p-value was <0.05. We used Student's t-test and chi-square analysis to compare baseline characteristics among groups. For objective comparison of voiding parameters, paired t-test or Wilcoxon signed rank test was performed. Logistic regression analysis was used to demonstrate risk factors for de novo urgency, UUI, or persistent UUI.
2. Ethics statement
The Institutional Review Board at Asan Medical Center approved this retrospective study (approval number: 2018-1084), and informed consent was waived because of the study design.
Go to :

RESULTS
1. Baseline demographics and urodynamic findings of the patients
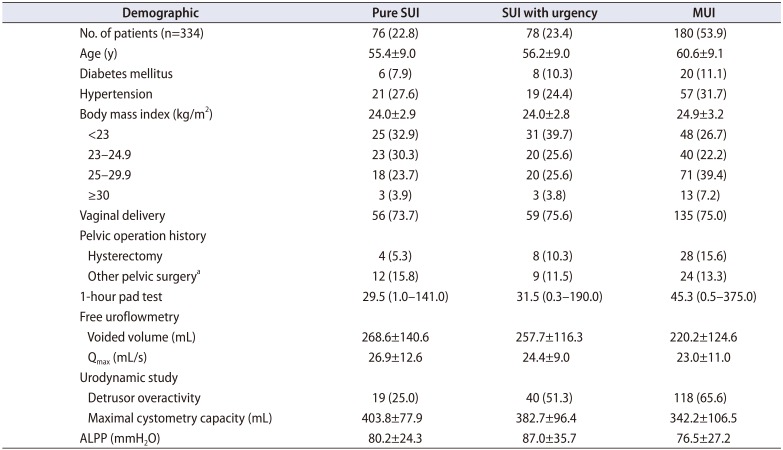
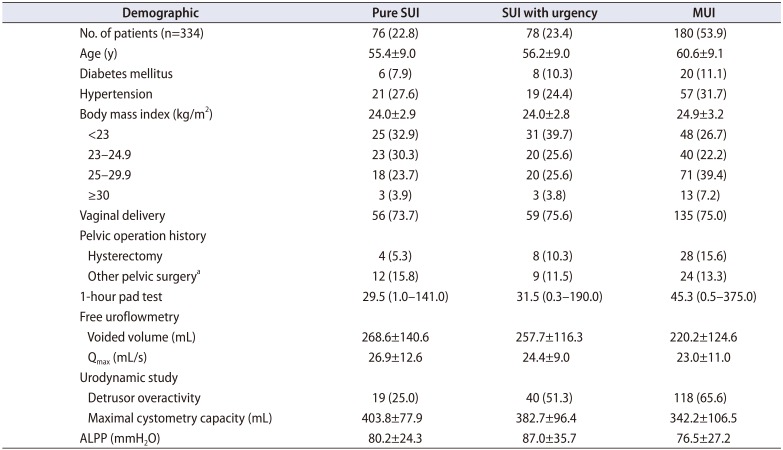
A total of 334 patients (mean age, 58.4±9.4 years) were included in the study. The mean time of symptom evaluation was 7.7 months. Overall, 76 patients had pure SUI, 78 had concurrent OAB dry, and 180 had MUI. Patients in the MUI group were significantly older than those in the pure SUI group (p<0.001). The MUI group had a higher body mass index (BMI, p=0.043) and tended to be more overweight (BMI ≥25 kg/m2, 46.6%) than the patients in the pure SUI group (27.6%). In addition, the MUI group had a higher proportion of patients with vaginal delivery and hysterectomy (p=0.023). There was no significant difference in demographics between the pure SUI and the SUI with urgency groups.
A perioperative voiding diary was available for 59.2% of the pure SUI group, 89.7% of the SUI with urgency group, and 83.3% of the MUI group. Patients with MUI had a significantly smaller voided volume, lower maximal flow rate (Q
max), and lower maximal cystometric capacity than did the patients with pure SUI (p=0.011, p=0.021, and p<0.001, respectively). Urodynamic detrusor overactivity (DO) was more frequently observed in the MUI and SUI with urgency group than in the pure SUI group (65.6% vs. 51.3% vs. 25.0%, respectively, p=0.001). There was no significant difference in abdominal leak point pressure among groups (
Table 1).
Table 1
Baseline demographics of the patients
|
Demographic |
Pure SUI |
SUI with urgency |
MUI |
|
No. of patients (n=334) |
76 (22.8) |
78 (23.4) |
180 (53.9) |
|
Age (y) |
55.4±9.0 |
56.2±9.0 |
60.6±9.1 |
|
Diabetes mellitus |
6 (7.9) |
8 (10.3) |
20 (11.1) |
|
Hypertension |
21 (27.6) |
19 (24.4) |
57 (31.7) |
|
Body mass index (kg/m2) |
24.0±2.9 |
24.0±2.8 |
24.9±3.2 |
|
<23 |
25 (32.9) |
31 (39.7) |
48 (26.7) |
|
23–24.9 |
23 (30.3) |
20 (25.6) |
40 (22.2) |
|
25–29.9 |
18 (23.7) |
20 (25.6) |
71 (39.4) |
|
≥30 |
3 (3.9) |
3 (3.8) |
13 (7.2) |
|
Vaginal delivery |
56 (73.7) |
59 (75.6) |
135 (75.0) |
|
Pelvic operation history |
|
|
|
|
Hysterectomy |
4 (5.3) |
8 (10.3) |
28 (15.6) |
|
Other pelvic surgerya
|
12 (15.8) |
9 (11.5) |
24 (13.3) |
|
1-hour pad test |
29.5 (1.0–141.0) |
31.5 (0.3–190.0) |
45.3 (0.5–375.0) |
|
Free uroflowmetry |
|
|
|
|
Voided volume (mL) |
268.6±140.6 |
257.7±116.3 |
220.2±124.6 |
|
Qmax (mL/s) |
26.9±12.6 |
24.4±9.0 |
23.0±11.0 |
|
Urodynamic study |
|
|
|
|
Detrusor overactivity |
19 (25.0) |
40 (51.3) |
118 (65.6) |
|
Maximal cystometry capacity (mL) |
403.8±77.9 |
382.7±96.4 |
342.2±106.5 |
|
ALPP (mmH2O) |
80.2±24.3 |
87.0±35.7 |
76.5±27.2 |

2. Prevalence and severity of de novo or resolved urgency and UUI
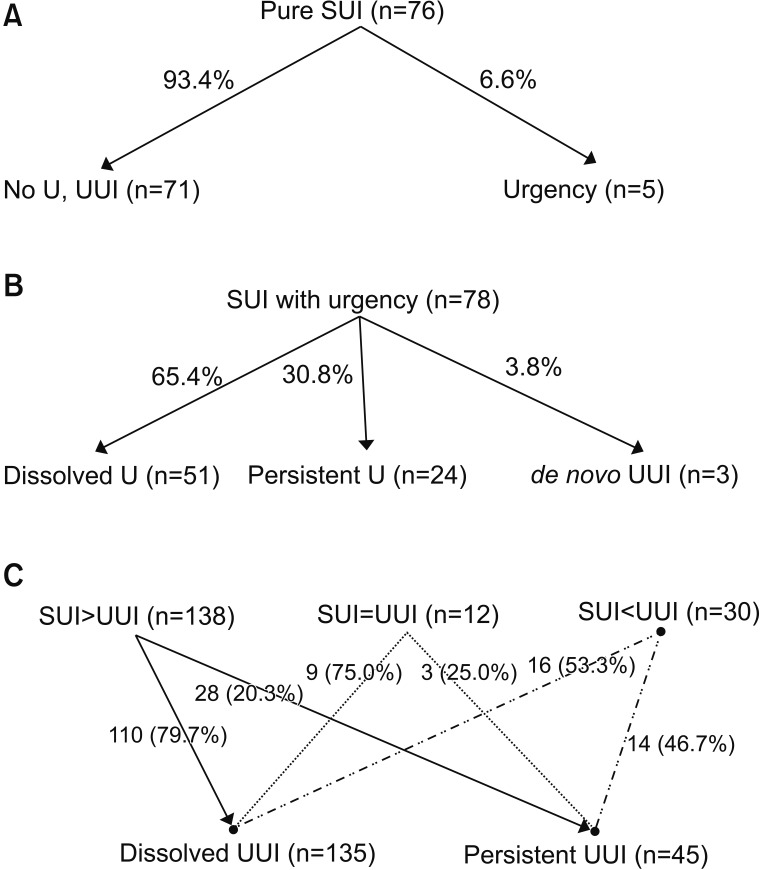
In the pure SUI group,
de novo urgency developed in five patients (6.6%,
Fig. 1A). Among them, four patients had positive DO in the preoperative urodynamic study. The severity of urgency was tolerable in four patients; only one patient required medical treatment.
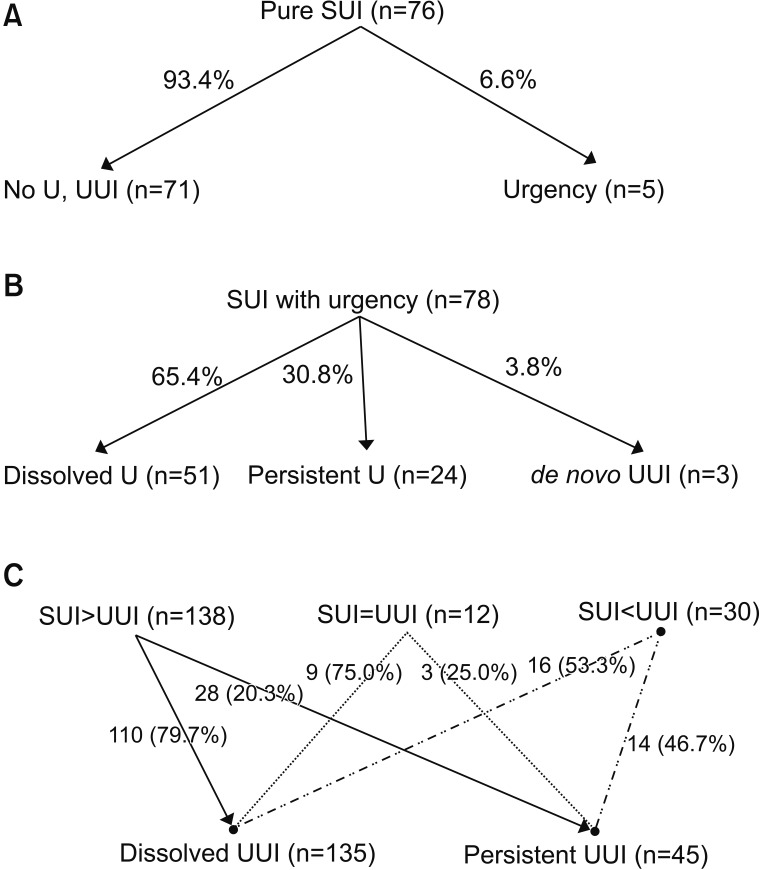 | Fig. 1Changes in urgency and urgency urinary incontinence (UUI) after a midurethral sling operation. (A) Pure stress urinary incontinence (SUI) group, (B) SUI with urgency group, (C) mixed urinary incontinence (MUI) group. U, urgency.
|
In the SUI with urgency group,
de novo UUI developed in three patients (3.8%). Two patients had positive DO in the preoperative urodynamic study. Fifty-one patients (65.4%) had resolved urgency (
Fig. 1B). In those with persistent urgency (30.8%), the subjective severity of urgency was improved in 11, the same in 7, and aggravated in 6. In the voiding diary, daily episodes of frequency decreased from 9.0±3.7/day to 7.4±2.4/day (p=0.05) and episodes of urgency decreased from 2.7±2.6/day to 1.8±2.2/day (p=0.407). Preoperatively, 10.3% of patients (8 of 78) had been treated with anticholinergics, and among them, four patients continued to take the medication after the operation. Seven patients started OAB medication with a mean interval of 3.3±1.9 months.
In the MUI group, 138 patients had predominant SUI (SUI>UUI). After the operation, 110 patients (79.7%) had resolved UUI, with resolved urgency in 79 and remnant urgency in 31. In patients with residual urgency, symptoms were improved in 26 and the same in 5. In the voiding diary, daily episodes of frequency decreased from 9.8±3.5/day to 8.0±3.0/day (p=0.044) and episodes of urgency decreased from 5.2±5.1/day to 3.3±4.4/day (p=0.322). Twenty-eight patients (20.3%) had persistent UUI (
Fig. 1C). Among them, the degree of urgency was improved in 15, the same in 7, and aggravated in 6. In the aspect of UUI, the patients' subjective symptoms were improved in 15, the same in 6, and aggravated in 7. Daily episodes of frequency decreased from 9.9±4.5/day to 7.9±1.9/day (p=0.039), episodes of urgency decreased from 6.8±6.0/day to 3.0±3.6/day (p=0.016), and UUI decreased from 2.9±6.5/day to 0.8±1.9/day (p=0.028).
Twelve patients presented with equivalent symptoms (SUI=UUI), and seven patients had been treated with OAB medication. After the operation, nine patients (75.0%) had resolved UUI, including five with resolved urgency and four with remnant urgency. In patients with residual urgency, the severity of urgency was improved in two, the same in one, and aggravated in one. Daily episodes of frequency decreased from 10.5±4.0/day to 7.1±0.5/day (p=0.109) and episodes of urgency decreased from 8.0±9.9 to 1.5±0.7/day (p=0.317). Three patients (25.0%) had persistent UUI. The patients' degree of urgency was improved in two and aggravated in one. UUI was improved in two and aggravated in one. Daily episodes of frequency changed from 8.7±0.5/day to 7.3±1.0/day (p=0.180), episodes of urgency changed from 3.5±0.7/day to 2.5±0.7/day (p=0.317), and UUI changed from 2.5±0.7/day to 2.0±1.4/day (p=0.317).
Thirty patients presented with dominant UUI (SUI<UUI) and 25 patients had been treated with OAB medication. After the operation, 16 patients (53.3%) had resolved UUI including 12 patients with resolved urgency and 4 with remnant urgency. In patients with residual urgency, the severity of urgency was improved in two and the same in two. Daily episodes of frequency decreased from 6.0±0.1/day to 5.5±0.2/day (p=0.180) and episodes of urgency decreased from 3.0±4.2/day to 2.8±4.0/day (p=0.317). Fourteen patients (46.7%) had persistent UUI, and their urgency severity was improved in four, the same in three, and aggravated in seven. UUI was improved in five, the same in two, and aggravated in seven. Daily episodes of frequency changed from 10.8±2.3/day to 8.1±2.7/day (p=0.058), episodes of urgency changed from 7.2±4.7/day to 5.2±4.6/day (p=0.397), and UUI changed from 2.2±1.7/day to 1.8±1.2/day (p=0.715).
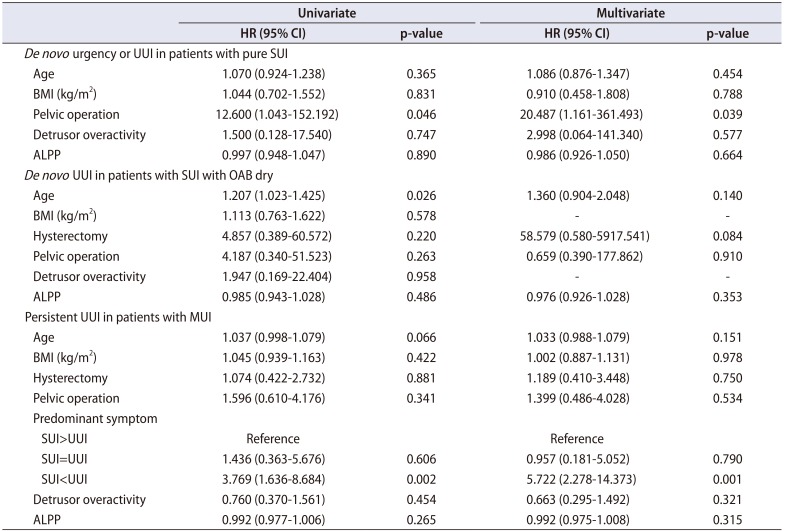
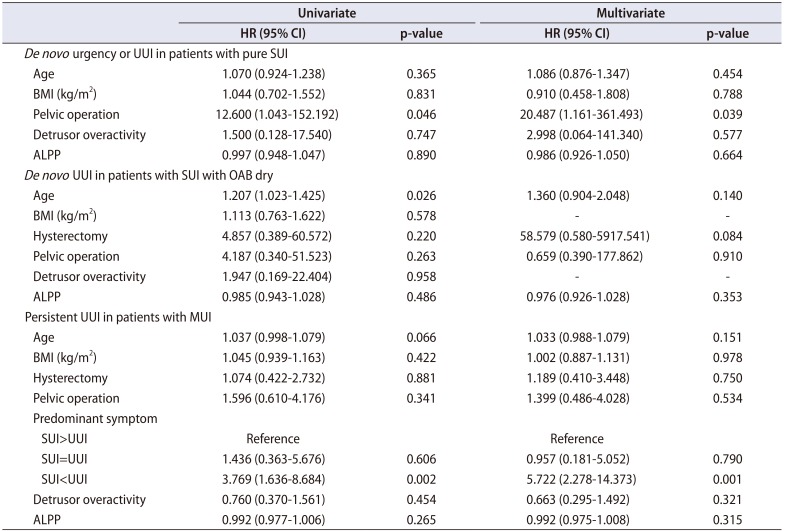
3. Risk factors of de novo or persistent urgency or UUI
In patients with pure SUI, previous pelvic operation was associated with
de novo urgency (hazard ratio [HR], 20.487; p=0.039) in the multivariate analysis (
Table 2). In the SUI with urgency group, age was associated with
de novo UUI (HR, 1.207; p=0.026) in the univariate analysis but was not significant in the multivariate analysis (
Table 2). Previous hysterectomy tended to increase the risk of
de novo UUI but was not statistically significant (HR, 58.579; p=0.084). In patients with MUI, subjectively predominant UUI was a predictive factor for persistent UUI in the multivariate analysis (HR, 5.722; p=0.001) (
Table 2).
Table 2
Risk factors for de novo or persistent urgency or UUI in SUI patients
|
Univariate |
Multivariate |
|
HR (95% CI) |
p-value |
HR (95% CI) |
p-value |
|
De novo urgency or UUI in patients with pure SUI |
|
|
|
|
|
Age |
1.070 (0.924-1.238) |
0.365 |
1.086 (0.876-1.347) |
0.454 |
|
BMI (kg/m2) |
1.044 (0.702-1.552) |
0.831 |
0.910 (0.458-1.808) |
0.788 |
|
Pelvic operation |
12.600 (1.043-152.192) |
0.046 |
20.487 (1.161-361.493) |
0.039 |
|
Detrusor overactivity |
1.500 (0.128-17.540) |
0.747 |
2.998 (0.064-141.340) |
0.577 |
|
ALPP |
0.997 (0.948-1.047) |
0.890 |
0.986 (0.926-1.050) |
0.664 |
|
De novo UUI in patients with SUI with OAB dry |
|
|
|
|
|
Age |
1.207 (1.023-1.425) |
0.026 |
1.360 (0.904-2.048) |
0.140 |
|
BMI (kg/m2) |
1.113 (0.763-1.622) |
0.578 |
- |
- |
|
Hysterectomy |
4.857 (0.389-60.572) |
0.220 |
58.579 (0.580-5917.541) |
0.084 |
|
Pelvic operation |
4.187 (0.340-51.523) |
0.263 |
0.659 (0.390-177.862) |
0.910 |
|
Detrusor overactivity |
1.947 (0.169-22.404) |
0.958 |
- |
- |
|
ALPP |
0.985 (0.943-1.028) |
0.486 |
0.976 (0.926-1.028) |
0.353 |
|
Persistent UUI in patients with MUI |
|
|
|
|
|
Age |
1.037 (0.998-1.079) |
0.066 |
1.033 (0.988-1.079) |
0.151 |
|
BMI (kg/m2) |
1.045 (0.939-1.163) |
0.422 |
1.002 (0.887-1.131) |
0.978 |
|
Hysterectomy |
1.074 (0.422-2.732) |
0.881 |
1.189 (0.410-3.448) |
0.750 |
|
Pelvic operation |
1.596 (0.610-4.176) |
0.341 |
1.399 (0.486-4.028) |
0.534 |
|
Predominant symptom |
|
|
|
|
|
SUI>UUI |
Reference |
|
Reference |
|
|
SUI=UUI |
1.436 (0.363-5.676) |
0.606 |
0.957 (0.181-5.052) |
0.790 |
|
SUI<UUI |
3.769 (1.636-8.684) |
0.002 |
5.722 (2.278-14.373) |
0.001 |
|
Detrusor overactivity |
0.760 (0.370-1.561) |
0.454 |
0.663 (0.295-1.492) |
0.321 |
|
ALPP |
0.992 (0.977-1.006) |
0.265 |
0.992 (0.975-1.008) |
0.315 |

Go to :

DISCUSSION
The midurethral sling operation has proven short-, mid-, and long-term efficacy for the treatment of SUI and is now the most commonly used technique for correction of SUI [
10]. Both methods of sling placement, outside-in and insideout, are safe and have demonstrated curative efficacy in previous studies [
11]. However,
de novo OAB is reported to develop in 6.4% to 11.5% of patients after the midurethral sling operation [
6]. Patients should be informed about their prognosis, because they may continue to experience deteriorated quality of life with different entities of discomfort.
Our study demonstrated that 6.6% of patients with pure SUI develop de novo urgency and 3.8% of patients with SUI combined with urgency develop de novo UUI within 1 year of a midurethral sling operation. The resolution rate of UUI was significantly higher in patients with predominant SUI than in patients with predominant UUI (79.7% vs. 53.3%). In patients with SUI with urgency, the subjective severity of persistent urgency improved in 45.8% and frequency significantly improved as recorded in a voiding diary. In the case of persistent UUI, subjective urgency and UUI improved in 53.6% and daily episodes of frequency, urgency, and UUI significantly decreased only in patients with predominant SUI.
Treatment guidelines for MUI are controversial, because both SUI and OAB symptoms should be targeted, but patients with MUI need surgical correction of the SUI component of their symptoms [
12]. A long-term follow-up study of transobturator-transvaginal tape operation in patients with SUI-predominant MUI showed clinically significant improvement in quality of life in 85.3% with a cure rate of 35% for urgency and 41% for UUI [
13]. Current studies suggest that more than half of patients with MUI might experience improvement in their OAB symptoms after a midurethral sling operation. However, most of these studies included only SUI-predominant patients and the degree of OAB symptom improvement is still unclear [
1415]. To overcome these limitations, we separated OAB symptoms into urgency and UUI and evaluated various types of SUI patients on the basis of their symptom severity. The overall cure rate of urgency was 65.4% in patients with SUI with urgency and 70.5% in patients with MUI. The overall cure rate of UUI was 75%. Subjective improvement in remnant UUI was much lower in the group with predominant UUI than in the group with predominant SUI (28.6% vs. 53.6%).
Old age, obesity, parity, nocturia, and OAB-related preoperative urodynamic study findings such as DO and low bladder capacity have been suggested as risk factors for
de novo urgency and UUI [
7]. In our study, previous pelvic operation was associated with
de novo urgency in patients with pure SUI. A recent prospective study by Natale et al. [
16] demonstrated that menopause and age over 60 years are risk factors for postoperative UUI and overall incontinence in patients with MUI. In our study, the patients' preoperative perception of predominant UUI was the only predictive factor for persistent UUI in the multivariate analysis (HR, 5.722; p=0.001). It is known that there could be a correlation between the presence of bladder outlet obstruction and OAB symptoms; however, there was no significant difference in maximal flow rate (22.4±9.7 mL/s vs. 21.1±11.0 mL/s, p=0.352) and post-void residual (50.0±90.5 mL vs. 46.4±69.8 mL, p=0.751) between pre- and postoperative uroflowmetry in cases of
de novo OAB symptoms.
Among 30 patients with predominantly UUI, 6 patients underwent a midurethral sling operation with untreated OAB symptoms. Five patients strongly demanded surgical correction of SUI first without OAB treatment, and one patient was unable to continue taking anticholinergic agents because of severe dry mouth. After the midurethral sling operation, two patients (33.3%) had resolved UUI and four patients had persistent UUI. The resolution rate of UUI was lower than in patients with untreated OAB symptoms (33.3% vs. 58.3%). The midurethral sling operation could be a possible treatment option for UUI-predominant patients if their symptoms are well-controlled. Patients should be aware that their MUI symptoms might be improved, but the cure rate is much lower than in the general population and it decreases in older patients and in those with predominant UUI.
In the current study we mainly presented short-term changes in OAB symptoms after a midurethral sling operation to focus on direct effects of the operation. Meanwhile, physicians should also pay attention to longitudinal changes in OAB symptoms. In our study population, none of the patients in the pure SUI group required further clinic visits. In the SUI with urgency group, three patients with persistent but tolerable urgency needed delayed prescription of anticholinergic agents. One patient developed de novo UUI at postoperative 14.7 months and two patients presented with aggravated urgency symptoms at postoperative 27.3 and 42.7 months, respectively. Thirteen patients with postoperatively dissolved UUI (completely dry, 7; residual urgency, 6) in the MUI group presented with recurrence or aggravation of OAB symptoms with a mean interval of 39.3±13.8 months postoperatively.
The limitation of our study was that it was a retrospective study of a single center without validated questionnaires. However, both the patients' subjective responses and voiding diaries were used for symptom quantification. A patient's subjective perception of their condition is by far one of the most important parameters in successful treatment. Our current findings suggest that adequate preoperative explanation about the prognosis of urgency and UUI after a midurethral sling operation might further increase patients' understanding and satisfaction.
Go to :

CONCLUSIONS
In our study sample, de novo urgency and UUI developed in a relatively small number of patients after a midurethral sling operation. The resolution rate of UUI was lower if the patients perceived UUI as a more bothersome symptom preoperatively. OAB symptoms might resolve postoperatively. When the symptoms persist, the patients' perception of symptom severity might improve in 50% of patients. Especially in patients with SUI-predominant MUI, daily episodes of frequency, urgency, and UUI may decrease significantly.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download