1. Barrett M. The handbook of clinically tested herbal remedies. Birmingham (NY): The Haworth Herbal Press®;2004.
2. Barnes J, Anderson LA, Phillipson JD, Newall CA. Herbal medicines: a guide for healthcare professionals. London: Pharmaceutical Press;2002.
3. Bamford JT, Ray S, Musekiwa A, van Gool C, Humphreys R, Ernst E. Oral evening primrose oil and borage oil for eczema. Cochrane Database Syst Rev. 2013; (4):CD004416. PMID:
23633319.

4. Morse NL, Clough PM. A meta-analysis of randomized, placebo-controlled clinical trials of Efamol evening primrose oil in atopic eczema. Where do we go from here in light of more recent discoveries? Curr Pharm Biotechnol. 2006; 7:503–524. PMID:
17168667.
5. Kerscher MJ, Korting HC. Treatment of atopic eczema with evening primrose oil: rationale and clinical results. Clin Investig. 1992; 70:167–171.

6. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty acid (fish or evening primrose oil) for schizophrenia. Cochrane Database Syst Rev. 2000; (2):CD001257. PMID:
10796622.
7. Belch JJ, Hill A. Evening primrose oil and borage oil in rheumatologic conditions. Am J Clin Nutr. 2000; 71(1 Suppl):352S–356S. PMID:
10617996.

8. Joe LA, Hart LL. Evening primrose oil in rheumatoid arthritis. Ann Pharmacother. 1993; 27:1475–1477. PMID:
8305783.
9. Wang W, Chen HS, Liu JP. Evening Primrose Oil or other essential fatty acids for the treatment of pre-menstrual syndrome (PMS). Cochrane Database Syst Rev. 2018; 2:CD001123.

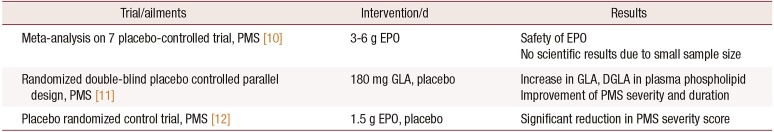
10. Budeiri D, Li Wan, Dornan JC. Is evening primrose oil of value in the treatment of premenstrual syndrome? Control Clin Trials. 1996; 17:60–68. PMID:
8721802.

11. Watanabe S, Sakurada M, Tsuji H, Matsumoto S, Kondo K. Efficacy of γ-linolenic acid for treatment of premenstrual syndrome, as assessed by a prospective daily rating system. J Oleo Sci. 2005; 54:217–224.
12. Saki M, Akbari S, Saki M, Tarrahi MJ, Gholami M, Pirdadeh S. The effect of primrose oil on the premenstrual syndrome among the female students in Lorestan University of Medical Sciences: a triple blind study. J Nurs Midwifery Sci. 2015; 2:20–26.

13. Gautam S, Srivastava A, Kataria K, Dhar A, Ranjan P, Kumar J. New breast pain chart for objective record of mastalgia. Indian J Surg. 2016; 78:245–248. PMID:
27358525.

14. Graham J, Franks S, Bonney RC. In vivo and in vitro effects of gamma-linolenic acid and eicosapentaenoic acid on prostaglandin production and arachidonic acid uptake by human endometrium. Prostaglandins Leukot Essent Fatty Acids. 1994; 50:321–329. PMID:
7938084.
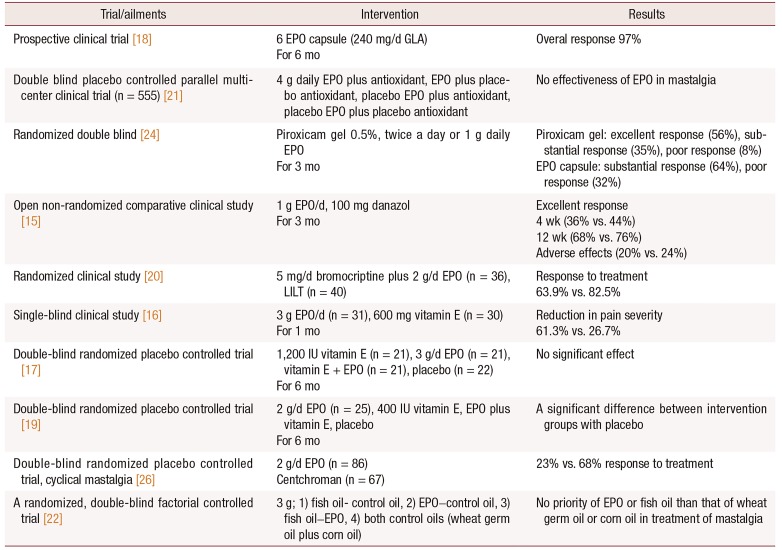
15. Parveen S, Sarwar G, Ali M, Channa GA. Danazol versus oil of evening primrose in the treatment of mastalgia. Pak J Surg. 2007; 23:10–13.
16. Fathizadeh N, Takfallah L, Ehsanpour S, Namnabati M, Askari S. Effects of evening primrose oil and vitamin E on the severity of periodical breast pain. Iran J Nurs Midwifery Res. 2009; 13:90–93.
17. Pruthi S, Wahner-Roedler DL, Torkelson CJ, Cha SS, Thicke LS, Hazelton JH, et al. Vitamin E and evening primrose oil for management of cyclical mastalgia: a randomized pilot study. Altern Med Rev. 2010; 15:59–67. PMID:
20359269.
18. Cheung KL. Management of cyclical mastalgia in oriental women: pioneer experience of using gamolenic acid (Efamast) in Asia. Aust N Z J Surg. 1999; 69:492–494. PMID:
10442919.
19. Alvandipour M, Tayebi P, Alizadeh Navaie R, Khodabakhshi H. Comparison between effect of evening primrose oil and vitamin E in treatment of cyclic mastalgia. J Babol Univ Med Sci. 2011; 13:7–11.
20. Saied GM, Kamel RM, Dessouki N. Low intensity laser therapy is comparable to bromocriptine-evening primrose oil for the treatment of cyclical mastalgia in Egyptian females. Tanzan Health Res Bull. 2007; 9:196–201. PMID:
18087899.

21. Goyal A, Mansel RE. A randomized multicenter study of gamolenic acid (Efamast) with and without antioxidant vitamins and minerals in the management of mastalgia. Breast J. 2005; 11:41–47. PMID:
15647077.

22. Sharma N, Gupta A, Jha PK, Rajput P. Mastalgia cured! Randomized trial comparing centchroman to evening primrose oil. Breast J. 2012; 18:509–510. PMID:
22892074.

23. Blommers J, de Lange-De Klerk ES, Kuik DJ, Bezemer PD, Meijer S. Evening primrose oil and fish oil for severe chronic mastalgia: a randomized, double-blind, controlled trial. Am J Obstet Gynecol. 2002; 187:1389–1394. PMID:
12439536.

24. Qureshi S, Sultan N. Topical nonsteroidal anti-inflammatory drugs versus oil of evening primrose in the treatment of mastalgia. Surgeon. 2005; 3:7–10. PMID:
15789786.

25. van der Sluijs CP, Bensoussan A, Liyanage L, Shah S. Women's health during mid-life survey: the use of complementary and alternative medicine by symptomatic women transitioning through menopause in Sydney. Menopause. 2007; 14(3 Pt 1):397–403. PMID:
17202872.
26. Farzaneh F, Fatehi S, Sohrabi MR, Alizadeh K. The effect of oral evening primrose oil on menopausal hot flashes: a randomized clinical trial. Arch Gynecol Obstet. 2013; 288:1075–1079. PMID:
23625331.

27. Kollias J, Macmillan RD, Sibbering DM, Burrell H, Robertson JF. Effect of evening primrose oil on clinically diagnosed fibroadenomas. Breast. 2000; 9:35–36. PMID:
14731582.

28. Jamilian M, Afshar R. Effects of combined evening primrose oil and vitamin D intake on hs-CRP, oxidative stress and pregnancy outcomes in women with gestational diabetes. J Arak Univ Med Sci. 2017; 19:43–51.

29. D'Almeida A, Carter JP, Anatol A, Prost C. Effects of a combination of evening primrose oil (gamma linolenic acid) and fish oil (eicosapentaenoic + docahexaenoic acid) versus magnesium, and versus placebo in preventing pre-eclampsia. Women Health. 1992; 19:117–131. PMID:
1492408.
30. Pizzorno JE, Murray MT, Joiner-Bey H. The clinician's handbook of natural medicine. St. Louis: Elsevier Health Sciences;2016.
31. Diansuy NN, Aguilar AS. The effectiveness of evening primrose oil gel capsule as a cervical ripening agent during labor induction as measured by bishop score on term singleton pregnant patients. Philipp Obstet Gynecol Soc. 2017; 41:1–4.
32. Dove D, Johnson P. Oral evening primrose oil: its effect on length of pregnancy and selected intrapartum outcomes in low-risk nulliparous women. J Nurse Midwifery. 1999; 44:320–324. PMID:
10380450.

33. Vahdat M, Tahermanesh K, Mehdizadeh Kashi A, Ashouri M, Solaymani Dodaran S, Kashanian M, et al. Evening primrose oil effect on the ease of cervical ripening and dilatation before operative hysteroscopy. Thrita. 2015; 4:e29876.

34. Tanchoco M, Aguilar AS. Cervical priming prior to operative hysteroscopy: a randomized controlled study comparing the efficacy of laminaria versus evening primrose oil (EPO). J Minim Invasive Gynecol. 2015; 22(6S):S45.

35. Jamison JR. Clinical guide to nutrition and dietary supplements in disease management. Amsterdam: Churchill Livingstone;2003.
36. Stockley IH. Stockley's drug interactions: a source book of interactions, their mechanisms, clinical importance, and management. London: Pharmaceutical Press;2002.
37. Gardner Z, McGuffin M. American Herbal Products Association's botanical safety handbook. Boca Raton, (FL): CRC Press/Taylor & Francis;2013.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download