1. Needham DM, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Sevransky JE, Dennison Himmelfarb CR, et al. Lung protective mechanical ventilation and two year survival in patients with acute lung injury: prospective cohort study. BMJ. 2012; 344:e2124.

2. Esteban A, Frutos-Vivar F, Muriel A, Ferguson ND, Peñuelas O, Abraira V, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013; 188(2):220–230.
3. Mehta AB, Syeda SN, Wiener RS, Walkey AJ. Epidemiological trends in invasive mechanical ventilation in the United States: a population-based study. J Crit Care. 2015; 30(6):1217–1221.

4. Darmon M, Azoulay E, Fulgencio JP, Garrigues B, Gouzes C, Moine P, et al. Procedure volume is one determinant of centre effect in mechanically ventilated patients. Eur Respir J. 2011; 37(2):364–370.

5. Bach PB, Cramer LD, Schrag D, Downey RJ, Gelfand SE, Begg CB. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med. 2001; 345(3):181–188.

6. Nallamothu BK, Saint S, Ramsey SD, Hofer TP, Vijan S, Eagle KA. The role of hospital volume in coronary artery bypass grafting: is more always better? J Am Coll Cardiol. 2001; 38(7):1923–1930.

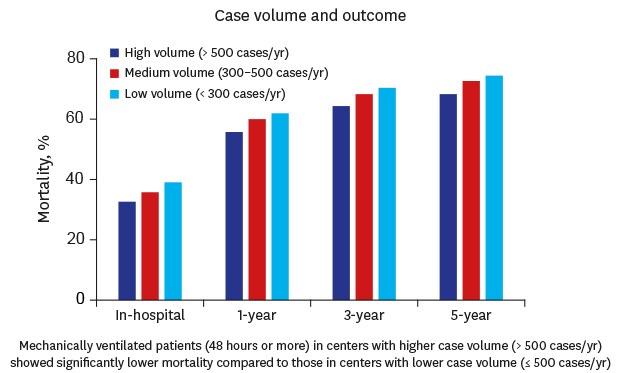
7. Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O'Brien CR, Rubenfeld GD. Hospital volume and the outcomes of mechanical ventilation. N Engl J Med. 2006; 355(1):41–50.

8. Durairaj L, Torner JC, Chrischilles EA, Vaughan Sarrazin MS, Yankey J, Rosenthal GE. Hospital volume-outcome relationships among medical admissions to ICUs. Chest. 2005; 128(3):1682–1689.

9. Moran JL, Solomon PJ. ANZICS Centre for Outcome and Resource Evaluation of the Australian and New Zealand Intensive Care Society. Mortality and intensive care volume in ventilated patients from 1995 to 2009 in the Australian and New Zealand binational adult patient intensive care database. Crit Care Med. 2012; 40(3):800–812.

10. Glance LG, Li Y, Osler TM, Dick A, Mukamel DB. Impact of patient volume on the mortality rate of adult intensive care unit patients. Crit Care Med. 2006; 34(7):1925–1934.

11. Cooke CR, Kennedy EH, Wiitala WL, Almenoff PL, Sales AE, Iwashyna TJ. Despite variation in volume, Veterans Affairs hospitals show consistent outcomes among patients with non-postoperative mechanical ventilation. Crit Care Med. 2012; 40(9):2569–2575.

12. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15.

13. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139.

14. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36(1):8–27.

15. van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009; 47(6):626–633.

16. Wunsch H, Wagner J, Herlim M, Chong DH, Kramer AA, Halpern SD. ICU occupancy and mechanical ventilator use in the United States. Crit Care Med. 2013; 41(12):2712–2719.

17. Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002; 287(3):345–355.
18. Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985–2000: an analysis of bed numbers, use, and costs. Crit Care Med. 2004; 32(6):1254–1259.

19. Jones J, Rowan K. Is there a relationship between the volume of work carried out in intensive care and its outcome? Int J Technol Assess Health Care. 1995; 11(4):762–769.

20. Ewart GW, Marcus L, Gaba MM, Bradner RH, Medina JL, Chandler EB. The critical care medicine crisis: a call for federal action: a white paper from the critical care professional societies. Chest. 2004; 125(4):1518–1521.
21. Schechtman D, He JC, Zosa BM, Allen D, Claridge JA. Trauma system regionalization improves mortality in patients requiring trauma laparotomy. J Trauma Acute Care Surg. 2017; 82(1):58–64.

22. Young MP, Gooder VJ, Oltermann MH, Bohman CB, French TK, James BC. The impact of a multidisciplinary approach on caring for ventilator-dependent patients. Int J Qual Health Care. 1998; 10(1):15–26.

23. Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W, et al. Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med. 1999; 27(12):2609–2615.

24. Gajic O, Afessa B. Physician staffing models and patient safety in the ICU. Chest. 2009; 135(4):1038–1044.

25. Kaplan LJ, Shaw AD. Standards for education and credentialing in critical care medicine. JAMA. 2011; 305(3):296–297.

26. Popovich MJ. Is lower mortality outcome and higher patient volume a genuine clinical relationship or an application of coin-flip statistics? Crit Care Med. 2012; 40(3):995–996.

27. Needham DM, Bronskill SE, Rothwell DM, Sibbald WJ, Pronovost PJ, Laupacis A, et al. Hospital volume and mortality for mechanical ventilation of medical and surgical patients: a population-based analysis using administrative data. Crit Care Med. 2006; 34(9):2349–2354.

28. Kanhere MH, Kanhere HA, Cameron A, Maddern GJ. Does patient volume affect clinical outcomes in adult intensive care units? Intensive Care Med. 2012; 38(5):741–751.

29. Abbenbroek B, Duffield CM, Elliott D. The intensive care unit volume-mortality relationship, is bigger better? An integrative literature review. Aust Crit Care. 2014; 27(4):157–164.

30. Shahin J, Harrison DA, Rowan KM. Relation between volume and outcome for patients with severe sepsis in United Kingdom: retrospective cohort study. BMJ. 2012; 344:e3394.

31. Metnitz B, Metnitz PG, Bauer P, Valentin A; ASDI Study Group. Patient volume affects outcome in critically ill patients. Wien Klin Wochenschr. 2009; 121(1-2):34–40.

32. Esteban A, Ferguson ND, Meade MO, Frutos-Vivar F, Apezteguia C, Brochard L, et al. Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med. 2008; 177(2):170–177.

33. Chao CT, Hou CC, Wu VC, Lu HM, Wang CY, Chen L, et al. The impact of dialysis-requiring acute kidney injury on long-term prognosis of patients requiring prolonged mechanical ventilation: nationwide population-based study. PLoS One. 2012; 7(12):e50675.

34. Lee MJ, Chen CJ, Lee KT, Shi HY. Trend analysis and outcome prediction in mechanically ventilated patients: a nationwide population-based study in Taiwan. PLoS One. 2015; 10(4):e0122618.

35. Lieberman D, Nachshon L, Miloslavsky O, Dvorkin V, Shimoni A, Zelinger J, et al. Elderly patients undergoing mechanical ventilation in and out of intensive care units: a comparative, prospective study of 579 ventilations. Crit Care. 2010; 14(2):R48.

36. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004; 351(13):1296–1305.

37. Metra M, Cotter G, Gheorghiade M, Dei Cas L, Voors AA. The role of the kidney in heart failure. Eur Heart J. 2012; 33(17):2135–2142.

38. Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004; 351(13):1285–1295.

39. Lebiedz P, Knickel L, Engelbertz C, Lüders F, Gebauer K, Berdel WE, et al. Impact of preexisting chronic kidney disease on acute and long-term outcome of critically ill patients on a medical intensive care unit. J Nephrol. 2014; 27(1):73–80.

40. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab J. 2014; 38(5):395–403.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download