INTRODUCTION
MATERIALS AND METHODS
Animals
PDL progenitor cell culture
Characteristics of isolated PDL progenitor cells
Colony-forming-units assay
Osteogenic and adipogenic differentiation
Collagen matrix as a carrier of PDL progenitor cells
Study design and protocols
 | Figure 1Clinical photographs of the surgical procedure. (A) Preoperative view of the first, second, and third premolars. (B) A dehiscence defect with a size of 5×5 mm (width × length) was surgically created. (C) Each site of the dehiscence defect was grafted with collagen matrix with PDL progenitor cells (COL/CELL group), grafted with collagen matrix alone (COL group), or left without any material (CTL group). (D) Primary closure was then performed.COL group: collagen matrix group, COL/CELL group: PDL progenitor cells with collagen matrix group, PDL: periodontal ligament, CTL group: sham control group.
|
Histologic processing
Histologic and histomorphometric analysis
 | Figure 2Schematic drawing of measurements. The bottom of the defect was set at the most apical point of the planed root surface, the most coronal point of newly formed cementum on the root surface was marked by a straight line, and the most apical point of the long junctional epithelium was also marked by a straight line. The newly formed bone was distinguished from the preexisting alveolar bone by its color.B: bone, PDL: periodontal ligament, C: cementum, JE: junctional epithelium, DH: defect height, NC: new cementum, CTA: connective-tissue adhesion, EA: epithelial adhesion, NB: new bone.
|
Statistical analysis
RESULTS
Characterization of PDL progenitor cells
 | Figure 3Characterization of PDL progenitor cells as mesenchymal stem cells. (A, B) Colony-forming-units assay revealed colony formation at 14 days after cell plating (stained with crystal violet). Although the colony formation decreased from (A) P3 to (B) P4, the size of the colonies was similar at (C) P3 and (D) P4. Adipogenic and osteogenic differentiation were induced after 4 and 2 weeks, respectively.PDL: periodontal ligament; P: passage.
|
SEM analysis of collagen matrix seeded with PDL progenitor cells
 | Figure 4Scanning electron microscopy photographs showing collagen matrix with periodontal ligament progenitor cells in the experimental group at observation periods of (A) 0 minutes, (B) 10 minutes, and (C) 30 minutes . The number of cells tended to decrease from 0 to 30 minutes, with some cells showing a spindle-like appearance. |
Clinical observations
Histologic and histomorphometric results
 | Figure 5Photomicrographs of the buccolingual section in the dehiscence defects of periodontal tissue in the (A) CTL, (B) COL, and (C) COL/CELL groups, displaying the sites from the apical extension of the surgically created defect (apical insert; a, d, and g) along the root surface to the coronal extension of the newly formed alveolar bone and cementum (midroot insert; b, e, and h), and the apical extension of epithelial adhesion (c, f, and i; hematoxylin-eosin stain).PDL: periodontal ligament, AB: alveolar bone, Ce: cementum, JE: junctional epithelium, COL group: collagen matrix group, COL/CELL group: PDL progenitor cells with collagen matrix group, CTL group: sham control group.
|
 | Figure 6Low-magnification photographs of the buccolingual section of the dehiscence defects of periodontal tissue in the (a) CTL, (b) COL, and (c) COL/CELL groups, along with high-magnification photographs from the sites of the dehiscence defects of periodontal tissue in the (A) CTL, (B) COL, and (C) COL/CELL groups. The newly formed PDL did not differ across the 3 groups (hematoxylin-eosin stain).Ce: cementum, PDL: periodontal ligament, AB, alveolar bone, CTL group: sham control group, COL group: collagen matrix group, COL/CELL group: PDL progenitor cells with collagen matrix group.
|
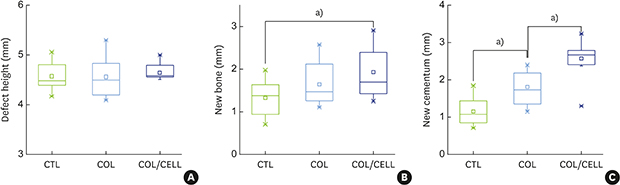
Table 1
Results of histometric analyses of periodontal tissue formation after surgery (1-way analysis of variance)

 | Figure 7Comparison of periodontal tissue formation. (A) The defect height did not differ significantly across the 3 groups (P=0.84). (B) New bone formation did not differ significantly across the 3 groups (P=0.058). However, the Tukey post hoc test revealed a significant difference between the CTL and COL/CELL groups (P=0.046). (C) New cementum formation differed significantly across the 3 groups (P=0.001).CTL group: sham control group, COL group: collagen matrix group, COL/CELL group: PDL progenitor cells with collagen matrix group.
a)P<0.05.
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download