Abstract
Purpose
To compare and analyze the rate of prevention of two venous thromboembolism prophylaxis guidelines in patients with artificial joint arthroplasty and hip joint fracture. Proper prophylaxis for preventing thromboembolism in orthopedic surgery is significant because of this fetal complication.
Materials and Methods
This study compared and retrospective analyzed the rate of prevention using the medical records and radiographs of patients who underwent orthopedic surgery from March 2009 to February 2011 according to the American College of Chest Physicians (ACCP) guidelines and from March 2012 to February 2014 according to the American Academy of Orthopedic Surgeons (AAOS) guidelines.
Results
The guidelines for venous thromboembolism prophylaxis have been applied to patients with artificial joint replacement and hip joint fracture, the compliance rate of the ACCP guidelines was 56.0% before surgery, 67.0% after surgery with chemical prophylaxis, and 80.5% with mechanical prophylaxis. In addition, the compliance rate of the AAOS guidelines was 74.1% with chemical prophylaxis, and 88.3% with mechanical prophylaxis, which was higher than the ACCP guidelines. The compliance rates of mechanical and chemical prophylaxis before and after surgery of the ACCP guidelines, and the compliance rate of mechanical and chemical prophylaxis of the AAOS guidelines were compared and analyzed. The results revealed statistical significance (p<0.05) before and after total knee replacement arthroplasty and hip joint fracture internal fixation and total high risk orthopedic surgery.
Figures and Tables
 | Figure 1Flow chart of patients treated according to the American College of Chest Physicians guidelines. TKRA, total knee replacement arthroplasty; THRA, total hip replacement arthroplasty; HFS, hip fracture surgery. |
 | Figure 2Flow chart of patients treated according to the American College of Orthopedic Surgeons guidelines. TKRA, total knee replacement arthroplasty; THRA, total hip replacement arthroplasty; HFS, hip fracture surgery. |
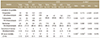
Table 3
Baseline Characteristics of Patients (2009. 3–2011. 2) at High Risk of Venous Thromboembolism with the ACCP Guideline

Table 4
Baseline Characteristics of Patients (2012. 3–2014. 2) at High Risk of Venous Thromboembolism with the AAOS Guidelines

Table 5
Patterns of Thromboprophylaxis of ACCP Guidelines for Patients at High Risk of Venous Thromboembolism

Table 7
Patterns of Thromboprophylaxis of the AAOS Guidelines for Patients at High Risk for Venous Thromboembolism

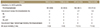
Table 9
Compliance and Outcome Analysis of the Guidelines
Values are presented as number (%). *p-value by Pearson chi-squared test, †p-value by Fisher's exact test. ACCP, American College of Chest Physicians; AAOS, American Acardemy of Orthopedic Surgeons; TKRA, total knee replacement arthroplasty; THRA, total hip replacement arthroplasty; HFS, hip fracture surgery.
References
1. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008; 133:381S–453S.
2. Kerr J, Linkins LA. High incidence of in-hospital pulmonary embolism following joint arthroplasty with dalteparin prophylaxis. Thromb Haemost. 2010; 103:123–128.

3. Hirsh J, Guyatt G, Albers GW, Harrington R, Schünemann HJ. Antithrombotic and thrombolytic therapy: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008; 133:110S–112S.
4. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016; 149:315–352.
5. Bratzler DW, Raskob GE, Murray CK, Bumpus LJ, Piatt DS. Underuse of venous thromboembolism prophylaxis for general surgery patients: physician practices in the community hospital setting. Arch Intern Med. 1998; 158:1909–1912.
6. Stratton MA, Anderson FA, Bussey HI, et al. Prevention of venous thromboembolism: adherence to the 1995 American College of Chest Physicians consensus guidelines for surgical patients. Arch Intern Med. 2000; 160:334–340.
7. Nicolaides A, Fareed J, Kakkar AK, et al. Prevention and treatment of venous thromboembolism: international consensus statement (guidelines according to scientific evidence). Clin Appl Thromb Hemost. 2013; 19:116–118.
8. SIGN. Prevention and management of venous thromboembolism. A national clinical guideline. Edinburgh: Scottish Intercollegiate Guidelines Network (SIGN);2010.
9. Park YS. Guideline for the prophylaxis of venous thromboembolism in hip surgery patients. J Korean Orthop Assoc. 2011; 46:95–98.

10. Guyatt G, Gutterman D, Baumann MH, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force. Chest. 2006; 129:174–181.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download