Abstract
Purpose
To estimate the annual socioeconomic costs of age-related macular degeneration (AMD) in the Republic of Korea.
Methods
We estimated the costs of illness to society of AMD patients, including medical, nonmedical, and productivity costs. The medical costs included official and nonofficial medical costs, and the nonmedical costs consisted of transportation, time, and nursing costs. We used Korea National Health Insurance Claims Database, National Health Insurance Service-National Sample Cohort, and Korea Health Panel study data in the analysis.
Results
The socioeconomic costs of AMD were estimated to be 694 billion Korean won (KRW) in 2016. This figure was divided into 501 billion KRW (72.1%) for medical costs, 61 billion KRW (8.8%) for nonmedical costs, and 133 billion KRW (19.1%) for productivity costs. The annual per capita socioeconomic cost of AMD was 1.32 million KRW.
Conclusions
We determined the scale and composition of the socioeconomic costs of AMD. Importantly, the productivity costs accounted for approximately 20% of all costs, suggesting that AMD had a significant impact on productivity. Because the disease costs of AMD are expected to increase continuously with the aging population, effective planning at the governmental level for prevention and treatment of AMD should be considered to reduce socioeconomic costs.
Figures and Tables
Table 1
The number and demographics of patients with age-related macular degeneration (AMD) between 2009 and 2016 according to the national claims database
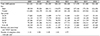
Table 2
The number of injections of ranibizumab and aflibercept per years between 2010 and 2016 according to the national claims database
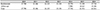
Table 3
The costs for outpatient clinic examinations and treatments of patients with age-related macular degeneration (AMD) (2016 current costs)

References
1. Friedman DS, O'Colmain BJ, Muñoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004; 122:564–572.

2. Park SJ, Kwon KE, Choi NK, et al. Prevalence and incidence of exudative age-related macular degeneration in South Korea: a nationwide population-based study. Ophthalmology. 2015; 122:2063–2070.e1.
3. Bressler SB, Bressler NM, Fine SL, et al. Natural course of choroidal neovascular membranes within the foveal avascular zone in senile macular degeneration. Am J Ophthalmol. 1982; 93:157–163.

4. Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006; 355:1432–1444.

5. Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012; 119:2537–2548.

6. La TY, Cho E, Kim EC, et al. Prevalence and risk factors for age-related macular degeneration: Korean National Health and Nutrition Examination Survey 2008–2011. Curr Eye Res. 2014; 39:1232–1239.

7. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006; 355:1419–1431.

8. Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014; 2:e106–e116.

9. Yoon KC, Mun GH, Kim SD, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008–2009. Korean J Ophthalmol. 2011; 25:421–433.

10. Cho BJ, Heo JW, Kim TW, et al. Prevalence and risk factors of age-related macular degeneration in Korea: the Korea National Health and Nutrition Examination Survey 2010–2011. Invest Ophthalmol Vis Sci. 2014; 55:1101–1108.

11. Obata R, Yanagi Y, Inoue T, et al. Prevalence and factors associated with age-related macular degeneration in a southwestern island population of Japan: the Kumejima Study. Br J Ophthalmol. 2018; 102:1047–1053.

12. Jin G, Ding X, Xiao W, et al. Prevalence of age-related macular degeneration in rural southern China: the Yangxi Eye Study. Br J Ophthalmol. 2018; 102:625–630.

13. Song P, Du Y, Chan KY, et al. The national and subnational prevalence and burden of age-related macular degeneration in China. J Glob Health. 2017; 7:020703.

14. Keel S, Xie J, Foreman J, et al. Prevalence of age-related macular degeneration in Australia: The Australian National Eye Health Survey. JAMA Ophthalmol. 2017; 135:1242–1249.
15. Colijn JM, Buitendijk GHS, Prokofyeva E, et al. Prevalence of age-related macular degeneration in Europe: the past and the future. Ophthalmology. 2017; 124:1753–1763.
16. Sedeh FB, Scott DAR, Subhi Y, Sørensen TL. Prevalence of neovascular age-related macular degeneration and geographic atrophy in Denmark. Dan Med J. 2017; 64:A5422.
17. Hwang HS, Lee SB, Jee D. Association between blood lead levels and age-related macular degeneration. PLoS One. 2015; 10:e0134338.

18. Kim EC, Cho E, Jee D. Association between blood cadmium level and age-related macular degeneration in a representative Korean population. Invest Ophthalmol Vis Sci. 2014; 55:5702–5710.

19. Kim EC, Han K, Jee D. Inverse relationship between high blood 25-hydroxyvitamin D and late stage of age-related macular degeneration in a representative Korean population. Invest Ophthalmol Vis Sci. 2014; 55:4823–4831.

20. Fujiwara S, Zhao X, Teoh C, et al. Disease burden of fractures among patients with osteoporosis in Japan: health-related quality of life, work productivity and activity impairment, healthcare resource utilization, and economic costs. J Bone Miner Metab. 2019; 37:307–318.

21. Shin WG, Kim HU, Kim SG, et al. Work productivity and activity impairment in gastroesophageal reflux disease in Korean full-time employees: a multicentre study. Dig Liver Dis. 2012; 44:286–291.

22. Patel VD, Watanabe JH, Strauss JA, Dubey AT. Work productivity loss in patients with dry eye disease: an online survey. Curr Med Res Opin. 2011; 27:1041–1048.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download