Abstract
The purpose of this review study is to evaluate sexual function and its effective factors in menopause. A systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The key words of “menopause,” “postmenopause,” “postmenopausal,” “premenopause,” “pre-menopausal period,” “sexual function,” “sexual health,” “sexuality,” “sexual and gender disorders,” “sexual development,” “sexual dysfunction,” “sexual disorders,” “sexual behavior and “sexual activity” were used in combination with the Boolean operators OR and AND. After reviewing the selected articles, 27 papers were selected based on the criteria for entering the study and the goals set. The results of the reviewed articles showed that, in the physical domain, the factors affecting sexual function can be mentioned, age, hormonal changes, medical problems and reproductive history. Sexual disorders in menopause can be affected by some of the individual and social characteristics and psychological problems. Considering the fact that many psychological and social injuries occur in this period following sexual disorders; therefore, policies and programs for improving the quality of life of women in menopause should be aimed at eliminating sexual dysfunction, correcting attitudes and negative emotions and help to women for more comfortable in menopause.
Go to : 
Menopause is one of the evolutionary stages that all women experience through aging, and this phenomenon exposes them to massive changes.12 Reducing estrogen levels in early stages of menopause period leads to a wide range of symptoms which can affect women's physical, mental and sexual health and affect work, social activities, mood, communication with others, life pleasure, and ultimately the quality of their life.3 In fact, women during menopause experience a transitional period that if a person feels that he is not able to change the structure of her life, there may be a developmental crisis in her life, and the physiological changes of this period may have a profound effect on her personal feelings and satisfaction with her life.45 The most comprehensive talk of menopause is menstruation, following the decline in ovarian activity at the end of women's fertility period, and short and medium term effects such as vasomotor disorders, urinary symptoms, atrophic vaginitis, and sexual disorders, as well as long-term effects such as osteoporosis and cardio-vascular disorders, along with many evolutionary, physical, emotional and social abnormalities.6 Sexuality and sexual function is regarded as one of the issues, which can be considered in this regard. A set of psychosocial aspects such as sexual stimulation and sexual desire are called sexual function.7 Sexuality is defined as a physical, emotional, psychological, and social welfare state associated with sexual desires, not just lack of disease, dysfunction, or disability. At this stage of life, women will face many problems and complications from the lack of sex hormones.8 Sexual relationships are one of the most important factors affecting the happiness of marital life, which, if not convincing, leads to a feeling of failure, defeat, and lack of security.9 The most significant causes of sexual disorders in this period are physiological changes of body, psychological problems and lack of sexual knowledge,10 which cause the sensitive period of menopause to become very risky, because sexual disorders lead to the destruction of the mental health of the family by creating or intensifying the psychological problems reciprocally. In this regard, many of the aggressions, controversies, and monitoring and control of couples in each other's activities can be linked to these disorders.910 Recognizing and studying human sexual behaviors is one of the most important public health issues, especially mental health.11 The World Health Organization considers sexual hygiene as an integrity and coordination among mind, body, and soul in order to promote human's social and intellectual aspects in her or his way through personality promotion, leading to communication and love. Therefore, any disorder leading to inconsistency and as a consequence of dissatisfaction with the sexual relationship can cause sexual dysfunction.12 The prevalence of sexual dysfunction among all women is estimated to be 25% to 63%. This outbreak is higher in women with menopause and reaches from 68% to 86.5%. Sexuality is not exclusively a physical phenomenon, but it relies on the individual's lifestyle, a deep and comprehensive grasp of someone from herself as a human being, the attitudes of others towards her and other factors.
Sexuality is more involved than any other activity in culture, society, and emotional values. Therefore, sexual desire affects all aspects of the individual's lives.13 Numerous factors can influence the sexual function of postmenopausal women, which has been addressed in numerous studies. In general, factors affecting sexual function have been studied in three domains including physical, emotional, and social factors. Considering the fact that socio-economic and cultural factors can influence on a person's and society's perception of sex and sexual behaviors, this study was conducted to evaluate the sexual function of postmenopausal women, along with its effective factors.
Go to : 
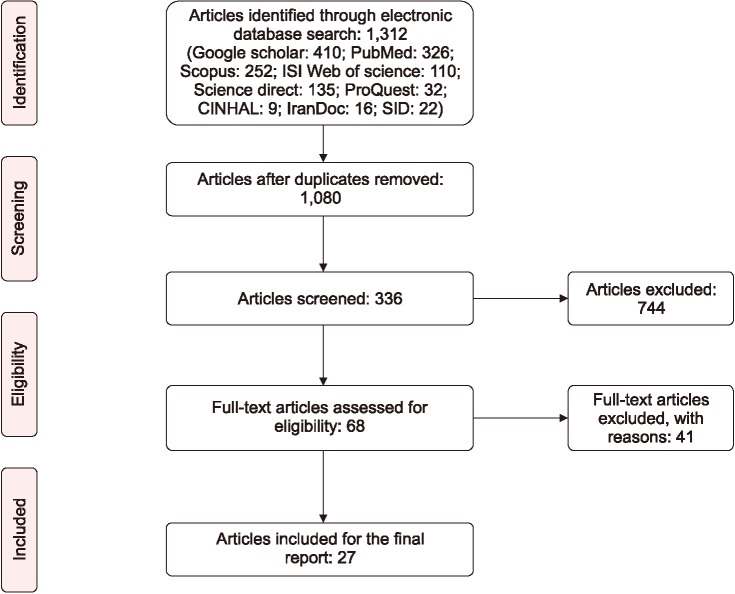
The review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.1415 The review included English language papers published from January 1, 2000 to July 21, 2017 through searching in Google Scholar (Google Inc., Mountain View, CA, USA), PubMed (National Library of Medicine, Bethesda, MD, USA), Ovid (New York, NY, USA), ISI Web of Science (Thomson Reuters, New York, NY, USA), Science Direct (Elsevier, Amsterdam, Netherlands), Scopus (Elsevier), ProQuest (Ann Arbor, MI, USA), CINHAL (EBSCO, Ipswich, MA, USA), IranDoc (Iranian Research Institute for Information Science and Technology, Tehran, Iran) and SID (Scientific Information Database, Tehran, Iran).
The search key words included “menopause,” “menopausal,” “post-menopause,” “post-menopausal,” “pre-menapause,” “pre-menopausal period,” “sexual function,” “sexual health,” “sexuality,” “sexual and gender disorders,” “sexual development,” “sexual dysfunction,” “sexual disorders,” “sexual behavior” and “sexual activity/ies.” Using OR and AND, the key words were combined and entered in the search box of the databases as follows: (menopause OR menopausal OR post-menopause OR postmenopausal OR post-menopausal OR pre-menapause OR pre-menopausal period) AND (sexual function OR sexual health OR sexuality OR sexual and gender disorders OR sexual development OR sexual dysfunction OR sexual disorders OR sexual behavior OR sexual activity/ies).
Figure 1 illustrates the process of study selection. After reviewing 1,312 articles, 27 articles including: 12 cross sectional, 7 descriptive, 3 prospective, 2 futuristic studies, 2 systematic reviews, and 1 qualitative study were selected.
In a study conducted by Dombek et al.16 the rate of sexual dysfunction was reported 70.3% among postmenopausal women. In addition, Jonusiene et al.17 reported this rate as 67.9% among postmenopausal women in Lithuania. In a sectional study done by Masliza et al.,18 confirmed that the prevalence of sexual dysfunction in women was 85.2% in Malaysia. Blümel et al.19 reported the prevalence of sexual dysfunction between 21% and 98.5% in their study, and this difference was related to the studied country and populations. In Iran, Kabudi,20 in his research on the knowledge about menopause and sexual function of women over 35 years old in Kermanshah, reported that sexual dysfunction responses in two phases of sexuality and erection in 141 menopausal women is 70%. However, Yazdanpanahi et al.21 reported the prevalence of sexual dysfunction during menopause as much as 88.7%. In another report in 2002 from the USA, this rate was 30%.22 Nazarpour et al.23 in their study aimed at examining the relationship between sexual function and the life quality of 405 Iranian postmenopausal women, determined that the average total score of sexual function was 24.11 ± 1.10. Further, the lowest and highest scores were related to erection and satisfaction, respectively. According to other studies, the prevalence of sexual dysfunction during menopause was achieved 51.3% in Chile,24 40.4% in Nigeria,25 and 35.9% in Brazil.26 Furthermore, in a population-based study, which was conducted in 28 cities of Iran, it was estimated that 39% of women over 50 years old are indulged with sexual dysfunction.27 In this regard, in a review study, da Silva Lara et al.28 found that 22% of postmenopausal women were involved in sexual activity only for the satisfaction of their husbands, and they were not willing to participate in these activities. Hashemi et al.29 in another cross-sectional study on 225 postmenopausal women between 45 and 65 years old in Iran, revealed that 70% of studied women at least are suffering from one sexual problem. Furthermore, in the study conducted by Topatan and Yıldız30 on 450 postmenopausal women in Turkey, a positive relationship was observed between multiple sexual dysfunctions and the comprehended level of menopause symptoms' intensity. In this regard, Simon et al.31 in their study on 2000 postmenopausal women and men in North America, showed that vaginal discomfort leads to loss of sexual desire (64%), and sexual pain (64%), and almost 30% of women and men introduced vaginal discomfort as a reason for stopping intercourse. In some studies, sexual complaints such as reduced sexual activity, decreased sexual response, difficulty in reaching to orgasm, and loss of genital sensation are associated with decreased estradiol levels.32 As mentioned, the factors affecting sexual function can be categorized in three domains: physical, emotional, and social. Sexual function of women after menopause is often influenced by vasomotor, neurogenic, endocrine, muscular, psychotic, drowsiness and symptoms of metabolic and psychological disorders.11
By examining some studies, it was found that there is a negative correlation between sexual function and individual' s age.2433 Other studies have reported positive association between poor sexual function and age.3435 In addition, in some studies, a negative relationship was found between the age of the spouse and female sexual function.36 In the field of education, a number of studies have revealed a positive connection between the level of female education or sexual partner with sexual function.83738 Beygi et al.39 considered spouse's education as an effective element in the sexual function of postmenopausal women. The study done by Dennerstein et al.40 confirmed the relationship between the education of couples and sexual dysfunction of women.
About estrogen deprivation, there has been an agreement on the reduction of sexual function.41 Other studies reported that lower levels of testosterone can predict sexual dysfunction in postmenopausal women.42 In his review, Schwenkhagen43 emphasized that reducing sexual desire, sexual stimulation, vaginal lubrication, etc., are associated with a decrease in the level of androgen. In another study, Gerber et al.33 conducted an interventional study on the effects of testosterone and psychological variables on the sexual function of postmenopausal women and indicated that there is a relationship between testosterone levels and sexual satisfaction between men 1 and 5 years after menopause. Further, Nappi et al.44 conducted a test on hormonal and psychological aspects and their association with sexual function during menopause and early stages of menopause. The results confirmed that sexual function was generally various at different stages of menopause. The application of hormone replacement therapy in a number of studies revealed positive impacts on the sexual function of postmenopausal women.4546 However, in another study, hormone therapy was not considered to be effective in stimulation and desire.45
According to some studies, ovarian disorders and bladder surgeries were related to sexual dysfunction.16 Based on the results of the study by Nazarpour et al.23 the incidence of medical problems in a person or a spouse was suggested as a remarkable factor in the sexual function of menopausal women. Among the medical problems, cardiovascular diseases, diabetes, and musculoskeletal problems in postmenopausal women were accounted as predictive factors in the scores of some domains and the overall score of sexual function.234748 Other studies have reported the connection between medical problems such as overactive bladder syndrome with sexual function in postmenopausal women.3849 Obesity issue is regarded as one of the other medical problems. In another study, increased sexual activity was observed among women with lower body mass index.50 Other factors are related to physical activity. In this regard, the results of a study indicated that exercise is a variable which is significantly related to sexual satisfaction.33
In a survey conducted by Guthrie et al.,51 which lasted 9 years, it became clear that as the menopause's start delays, sexual abnormalities may increase from 42% to 88% due to a severe decrease of sexual hormones. The results of a review study revealed that overall sexual function decreased from 88% in the first year after menopause to 34% after 8 years.28 However, Blumel et al.52 reported that sexual function increases after five years of menopause which is related to a reduction in the severity of symptoms and a shift away from acute menopausal conditions. The reason for this contradiction may be due to the positive attitude that women in some societies gain toward menopause after menstruation. Another review indicated that low sexual function was positively associated to the number of pregnancies, deliveries, and abortions.35
Among the factors studied in different studies, the psychoemotional field, depression, anxiety are highlighted. The findings of the studies reported that there is a significant relationship between sexual dysfunction, depression and anxiety.173953 Furthermore, they suggested that depression is the most important element in describing sexual dysfunction.21 Researchers believe that reducing sexual desire causes mental, emotional disorders and interpersonal distress, leading to a decline in general health.54
Graziottin and Basson,55 in their study, reported that sexual behaviors are complex and diverse and are influenced by interpersonal relationships, lifestyle and cultural conditions. This behavior is closely related to the biological structure and the general feeling of the individual towards himself or herself as a man or a woman, and the experiences and developments of a person with respect to sexual matters. The underlying and interpersonal issues are responsible for most of the changes, which are experienced in sexual life during menopausal years, but they are not responsible for all of them.56 Further, social expectations have a negative impact on sexual desire. Some cultures believe that older women are diverted from sexuality.57 Nisar and Ahmed Sohoo58 demonstrated that postmenopausal women from traditional societies often tend to take care of children, grandchildren and religious practices during this time, and that participation in sexual activities is observed as later priority for them. Evidences from other investigations have suggested that the prevalence of sexual dysfunction is affected by racial, religious, cultural and attitudinal factors because social attitudes, cultural roles and religious believes can influence the sexual orientation of older women.834 García Padilla et al.59 proved that increased sexual dysfunction and other menopausal symptoms among these women are related to their low sexual awareness. Nappi and Nijland60 conducted a study in Europe on women's understanding about gender in during menopause. They concluded that 34% of women were at risk of low libido.
In addition, a large number of studies emphasized a significant statistical relationship between the quality of the relationship with the spouse and sexual dysfunction. The results of another study by Beygi et al.39 revealed that the least amount of sexual dysfunctions was found in a group that reported very good relationship with their spouses. Accordingly, the percentage of sexual dysfunctions increased as the quality of couples' relationships in these groups reduced since 100% of the cases had sexual dysfunction in a group with a very bad relationship with their spouses.
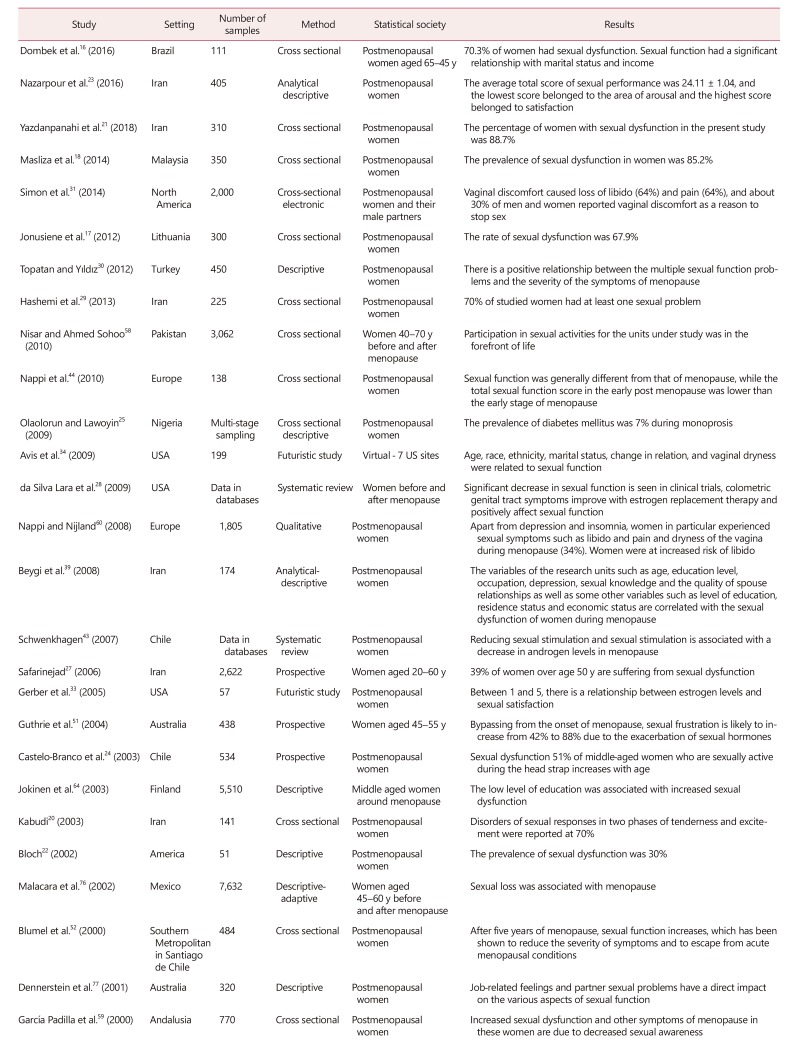
Furthermore, some studies proposed that employed women have a greater sexual desire than housewives, which can affect sexual satisfaction and is considered important in other studies.3961 However, Blumel et al.52 found that housewives had a better quality of life in terms of sex than employed women, while employed women were more likely to be self-confident due to financial independence.6263 The women with low income can have fewer sexual attraction, leading to a decrease in their sexual activities.35 Jokinen et al.64 focused on the occupation of women and sexual disorders. Another study suggests that women's age and marriage can reduce their sexual function.54 The duration of marriage and marriage are considered as other social factors. In another study, less problems were related to sexual intercourse by increase in life expectancy.65 In another study, the length of women's marriage could reduce their sexual function17 and the high risk of sexual dysfunction was significantly related to the duration of marriage.66 The findings of the studies conducted on sexual function and factors affecting the sexual functions of postmenopausal women (physical, mental and social domains) are presented in Table 1.
Go to : 
In many countries around the world, the average life expectancy of women is about 80 years. Although the ovaries have lost their activity 25 years before reaching that age, menstrual bleeding does not continue until the age of 51 years on average. Thus, every woman is associated the last third part of her life with lack of production and deficiency of sex hormones. Symptoms of menopause are often due to the reduction of estrogen hormone, which can lead to complications such as hot flashes, sweating, headaches, muscle and joint aches, sleep disorders, etc., which may have an adverse effect on the quality of life of a person and the starting point for a series of side effects. For example, urogenital epithelia atrophy can lead to frequent urination, pain during urination, and discomfort in the vaginal area.67 Other symptoms of estrogen deficiency include depression, fatigue, redness and inflammation of the skin, memory disorders, lack of concentration and loss sexual desire.68 Therefore, the proposed studies have considered the effect of estrogen deprivation in reducing sexual function.334243 Regarding physical activities such as exercise, Lange-Collett69 argued that exercise and nutrition are two important factors in the life of postmenopausal women and determined their health status. In another study, Verit et al.35 reported exercise as an alternative treatment option for reducing menopausal symptoms such as psychological, mediational, physical, and sexual symptoms. In the same study, the effect of regular exercise on the improvement of sexual function was highlighted.33 Based on the results of some studies, it seems that the presence of medical condition is regarded as one of the outstanding issues which can influence sexual function.23384950 Chronic medical conditions tend to decrease simulation and desire. In this regard, Nascimento et al.70 in their systematic review about sexual dysfunction and cardiovascular diseases, reported that in all women, all areas of sexual functions such as tenderness, simulation, lubrication, orgasm, sexual satisfaction and pain are affected by cardiovascular diseases and cardiovascular disease are risk factors for developing sexual dysfunction in women and men. The severity of heart diseases increases the incidence of sexual dysfunction. In addition, the psychosocial factors originated from cardiovascular events gradually affected the sexual life of patients which contribute to sexual dysfunctions. Further, symptoms of depression associated with cardiovascular diseases lead to impaired sexual response. In an experiment by Doruk et al.71 the scores of sexual desire, stimulation and lubrication in the type I diabetic group were significantly lower than in the control group. However, no risk factor was discovered which could predict sexual dysfunction in diabetic women. Postmenopausal women experience numerous psychological changes and have feelings about their negative reactions to menopausal transformations. These changes can affect interpersonal, social, family, and the total quality of their life.72 The reduction of sexual function is considered as one of the important complications of this period which play a negative effect on their sexual function according to the reviewed articles.171819 Additionally, some studies indicated that postmenopausal women experience aging, altered mental image of their appearance, and feelings of femininity end, disability, disappointment, depression, and anxiety which can influence their sexual function.72 In line with the results of some control studies,17213953 Borissova et al.73 reported that decreased libido in postmenopausal women may be related to some psychological factors like depression. Danaci et al.74 indicated that anxiety and depression have a profound effect on sexual relationships. Some experiments emphasized the relationship between age and sexual function.2433343536 An increase in age leads to a decrease in sexual responses and sexual desire, as well as the frequency of sexual intercourse during menopause. Consequently, sexual function faces with disorder which can be an important factor in reducing sexual function in postmenopausal women.75 In addition, Malacara et al.,76 in another study on Mexican women with urban and rural settlements, reported that libido was affected by aging so that postmenopausal women tended to have reduced sexual desire more than women before menopause. Dennerstein et al.77 demonstrated that women's sexual responses during middle age are influenced by two factors of age, while Gott and Hinchliff78 reported that aging and long-term relationships with the spouse are needed to counteract the decline in couples' sexual desires. Ponholzer et al.,79 in their study on the risk factors and the prevalence of sexual dysfunction among 703 Australian women, found that 22%, 35%, and 39% had sexual desire dysfunctions, sexual arousal, and orgasmic problems, respectively, and all of these factors increased significantly by aging. Similarly, in another study, on low sexual desire in middle-aged and old women, Hartmann et al.80 found similar results by indicating the prevalence of sexual dysfunction, especially low sexual desire and sexual arousal disorders with aging. The stressors in life, the underlying factors such as the quality of communication and personality factors, past experiences and sexual desires, and physical and mental health are other important predictors of female sexual dysfunction in this study. The level of education is a predictive variable for psychological complications and negative emotions of menopause which can affect women's sexual function during this period,8373840 and it is regarded as one of the reasons that education increases self-confidence and helps to have a good impression of health.81 The results of some studies revealed that female sexual function is reduced by increasing the level of education.8283 On the other hand, the study on the reviewed articles confirmed the relationship between sexual performance and the quality of the relationship with the spouse.39 In another study conducted by Liu and Eden,84 many Chinese postmenopausal women believed that a decline in sexual activity begins with menopause and if their husbands were willing to remarry due to disrupted sexual relationship, they would agree on this because they believed that during this period, lack of libido may lead to separation and more emotional distance with their husbands. In addition, Beutel et al.85 reported old German men consider proper relationships with their wives as a factor in increasing sexual desire. In this regard, Kingsberg86 proved that the mental or physical problems of the sexual partner and, consequently, the reduction of the desired relationship with the partner are key factors for developing sexual dysfunctions. Further, having a good relationship between the couples during middle and old age decreases the dramatic effect of their physical and psychological statues of these individuals on their sexual relationship and these individuals can follow normal sexual activities. The prevalence of sexual dysfunctions varies from country to country. Considerable differences among the statistics can be attributed to racial, religious, cultural and attitudinal factors, because social attitude, cultural roles and religious believes can affect the experience of sexual desires of elderly women,87 as it was highlighted by a large number of studies.83458 Wright88 believes that female sexual value and attraction are only for reproduction in some cultures, while Deacon et al.89 emphasize that women are less important than the women at the age of fertility in terms of sexual value due to lack of reproduction and it seems to be more likely as the result of community culture. This is justified by the fact that having a high income is likely to lead to more mental relief, which leads to sexual satisfaction. The middle age is a period of attention to spirituality, and people often evaluate themselves and have a special look at the end of their lives. The type of religious attitude is important to sexual relationships and can affect sexual satisfaction.87 Findings confirm the relationship between sexual function and awareness of postmenopausal women.5960 Knowledge of menopause trend can increase orgasmicity. High awareness which can be achieved through higher education can change attitudes and thoughts toward gender, reduce anxiety, and helps the individual adapt to menopause.90 In another review conducted on Chinese women, Beutel et al.85 concluded that they had no information about treatments which can eliminate sexual dysfunction and their awareness was very low. Increasing sexual awareness during this period helps the individuals not to consider the sexual dysfunctions abnormal which are resulted from menopausal symptoms and changes in sexual behavior by aging, but attempted to adapt, resolve or mitigate these problems. Therefore, the role of sexual awareness in preventing and treating sexual disorders in women is quite obvious. It seems embarrassment to talk about sexual issues, the lack of proper understanding of sexual issues, and lack of sufficient information about these issues are regarded as some significant causes of sexual problems in the early experiences of married life.66 Palacios et al.91 found that examining the sexual history of postmenopausal women since fertility age is the first step in diagnosing and treating postmenopausal women with sexual dysfunction, which is consistent with the results of the studies which correlated sexual function with the number of pregnancies and childbirth.35 Regarding hormonal treatment, it seems that the hormone administration and its onset are effective in the level of sexual function.92 As it was already mentioned, some studies have shown the protective effect of hormone therapy on sexual function.4546
Go to : 
Regarding all of the results obtained from this study, it is recommended that the staff of health centers should remind menopausal women about their evolution by aging and reaching menopause. In addition, they should emphasize sexual desire in every person's life by contemplated programming for the continuous and sequential training courses for menopausal women about sexual activity, the physiological changes during menopause, and their way of adapting themselves in order to prevent them from psychological and social consequences of sexual dysfunctions.
Go to : 
References
1. Heidari M, Ghodusi M, Rafiei H. Sexual self-concept and its relationship to depression, stress and anxiety in postmenopausal women. J Menopausal Med. 2017; 23:42–48. PMID: 28523258.

2. Heidari M, Shahbazi S, Ghafourifard M, Ali Sheikhi R. Prediction of marital satisfaction based on emotional intelligence in postmenopausal women. J Menopausal Med. 2017; 23:196–201. PMID: 29354620.

3. Shirvani M, Heidari M. Quality of life in postmenopausal female members and non-members of the elderly support association. J Menopausal Med. 2016; 22:154–160. PMID: 28119895.

4. Kim TH, Lee HH. Atlernative therapy trends among Korean postmenopausal women. J Menopausal Med. 2016; 22:4–5. PMID: 27152306.
5. Jafari M, Seifi B, Heidari M. Risk assessment: factors contributing to discomfort for menopausal women in workplace. J Menopausal Med. 2017; 23:85–90. PMID: 28951855.

6. Enkhbold T, Jadambaa Z, Kim TH. Management of menopausal symptoms in Mongolia. J Menopausal Med. 2016; 22:55–58. PMID: 27617236.

7. Thompson WK, Charo L, Vahia IV, Depp C, Allison M, Jeste DV. Association between higher levels of sexual function, activity, and satisfaction and self-rated successful aging in older postmenopausal women. J Am Geriatr Soc. 2011; 59:1503–1508. PMID: 21797827.

8. Ornat L, Martínez-Dearth R, Muñoz A, Franco P, Alonso B, Tajada M, et al. Sexual function, satisfaction with life and menopausal symptoms in middle-aged women. Maturitas. 2013; 75:261–269. PMID: 23684086.

9. Chedraui P, Pérez-López FR, Sánchez H, Aguirre W, Martínez N, Miranda O, et al. Assessment of sexual function of mid-aged Ecuadorian women with the 6-item Female Sexual Function Index. Maturitas. 2012; 71:407–412. PMID: 22342384.

10. Cabral PU, Canário AC, Spyrides MH, Uchôa SA, Eleutério J Jr, Amaral RL, et al. Influence of menopausal symptoms on sexual function in middle-aged women. Rev Bras Ginecol Obstet. 2012; 34:329–334. PMID: 22948506.
11. Berman JR. Physiology of female sexual function and dysfunction. Int J Impot Res. 2005; 17(Suppl 1):S44–S51. PMID: 16391543.

12. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26:191–208. PMID: 10782451.
13. Cheng MH, Wang SJ, Wang PH, Fuh JL. Attitudes toward menopause among middle-aged women: a community survey in an island of Taiwan. Maturitas. 2005; 52:348–355. PMID: 16009512.

14. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4:1. PMID: 25554246.

15. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009; 6:e1000100. PMID: 19621070.

16. Dombek K, Capistrano EJ, Costa AC, Marinheiro LP. Risk factors associated with sexual dysfunction in Brazilian postmenopausal women. Int J Impot Res. 2016; 28:62–67. PMID: 26865103.

17. Jonusiene G, Zilaitiene B, Adomaitiene V, Aniuliene R, Bancroft J. Sexual function, mood and menopause symptoms in Lithuanian postmenopausal women. Climacteric. 2012; 16:185–193. PMID: 22845491.

18. Masliza W, Daud W, Yazid Bajuri M, Shuhaila A, Hatta S, Rohaizat Hassan M, et al. Sexual dysfunction among postmenopausal women. Clin Ter. 2014; 165:83–89. PMID: 24770809.
19. Blümel JE, Chedraui P, Baron G, Belzares E, Bencosme A, Calle A, et al. Sexual dysfunction in middle-aged women: a multicenter Latin American study using the Female Sexual Function Index. Menopause. 2009; 16:1139–1148. PMID: 19458559.
20. Kabudi M. The study of over 35 women's knowledge and interaction against menopause. Paper presented at: 1st Congress of Family and Sexual Disorders, Shahed University of Medical Sciences. 2003; Tehran, Iran.
21. Yazdanpanahi Z, Nikkholgh M, Akbarzadeh M, Pourahmad S. Stress, anxiety, depression, and sexual dysfunction among postmenopausal women in Shiraz, Iran, 2015. J Family Community Med. 2018; 25:82–87. PMID: 29922107.
23. Nazarpour S, Simbar M, Ramezani Tehrani F, Alavi Majd H. Relationship between sexual function and quality of life in post-menopausal women. J Mazandaran Univ Med Sci. 2016; 26:90–98.
24. Castelo-Branco C, Blumel JE, Araya H, Riquelme R, Castro G, Haya J, et al. Prevalence of sexual dysfunction in a cohort of middle-aged women: influences of menopause and hormone replacement therapy. J Obstet Gynaecol. 2003; 23:426–430. PMID: 12881088.

25. Olaolorun FM, Lawoyin TO. Experience of menopausal symptoms by women in an urban community in Ibadan, Nigeria. Menopause. 2009; 16:822–830. PMID: 19242385.

26. Valadares AL, Pinto-Neto AM, Osis MJ, Sousa MH, Costa-Paiva L, Conde DM. Prevalence of sexual dysfunction and its associated factors in women aged 40-65 years with 11 years or more of formal education: a population-based household survey. Clinics (Sao Paulo). 2008; 63:775–782. PMID: 19061000.

27. Safarinejad MR. Female sexual dysfunction in a population-based study in Iran: prevalence and associated risk factors. Int J Impot Res. 2006; 18:382–395. PMID: 16395324.

28. da Silva Lara LA, Useche B, Rosa E Silva JC, Ferriani RA, Reis RM, de Sá MF, et al. Sexuality during the climacteric period. Maturitas. 2009; 62:127–133. PMID: 19186014.

29. Hashemi S, Ramezani Tehrani F, Simbar M, Abedini M, Bahreinian H, Gholami R. Evaluation of sexual attitude and sexual function in menopausal age; a population based cross-sectional study. Iran J Reprod Med. 2013; 11:631–636. PMID: 24639800.
30. Topatan S, Yıldız H. Symptoms experienced by women who enter into natural and surgical menopause and their relation to sexual functions. Health Care Women Int. 2012; 33:525–539. PMID: 22577740.

31. Simon JA, Nappi RE, Kingsberg SA, Maamari R, Brown V. Clarifying Vaginal Atrophy's Impact on Sex and Relationships (CLOSER) survey: emotional and physical impact of vaginal discomfort on North American postmenopausal women and their partners. Menopause. 2014; 21:137–142. PMID: 23736862.
32. Gallicchio L, Schilling C, Tomic D, Miller SR, Zacur H, Flaws JA. Correlates of sexual functioning among mid-life women. Climacteric. 2007; 10:132–142. PMID: 17453861.

33. Gerber JR, Johnson JV, Bunn JY, O'Brien SL. A longitudinal study of the effects of free testosterone and other psychosocial variables on sexual function during the natural traverse of menopause. Fertil Steril. 2005; 83:643–648. PMID: 15749493.

34. Avis NE, Brockwell S, Randolph JF Jr, Shen S, Cain VS, Ory M, et al. Longitudinal changes in sexual functioning as women transition through menopause: results from the Study of Women's Health Across the Nation. Menopause. 2009; 16:442–452. PMID: 19212271.
35. Verit FF, Verit A, Billurcu N. Low sexual function and its associated risk factors in pre- and postmenopausal women without clinically significant depression. Maturitas. 2009; 64:38–42. PMID: 19632073.

36. Chedraui P, Pérez-López FR, Mezones-Holguin E, San Miguel G, Avila C. Collaborative Group for Research of the Climacteric in Latin America (REDLINC). Assessing predictors of sexual function in mid-aged sexually active women. Maturitas. 2011; 68:387–390. PMID: 21237590.

37. Llaneza P, Fernández-Iñarrea JM, Arnott B, García-Portilla MP, Chedraui P, Pérez-López FR. Sexual function assessment in postmenopausal women with the 14-item changes in sexual functioning questionnaire. J Sex Med. 2011; 8:2144–2151. PMID: 21679299.

38. Merghati-Khoei E, Sheikhan F, Shamsalizadeh N, Haghani H, Yousofnia Pasha YR, Killeen T. Menopause negatively impacts sexual lives of middle-aged Iranian women: a cross-sectional study. J Sex Marital Ther. 2014; 40:552–560. PMID: 24308863.

39. Beygi M, Fahami F, Hasan-Zahraei R, Arman S. Sexual dysfunction in menopause. J Isfahan Med Sch. 2008; 26:294–300.
40. Dennerstein L, Lehert P, Burger H, Dudley E. Factors affecting sexual functioning of women in the mid-life years. Climacteric. 1999; 2:254–262. PMID: 11910659.

41. Tansupswatdikul P, Chaikittisilpa S, Jaimchariyatam N, Panyakhamlerd K, Jaisamrarn U, Taechakraichana N. Effects of estrogen therapy on postmenopausal sleep quality regardless of vasomotor symptoms: a randomized trial. Climacteric. 2015; 18:198–204. PMID: 25242569.

42. Mostafa T, Mostafa RM, Hassan MM, Nasrallah YS, Salman WS, Taymour M. Female sexual dysfunction among menopausal women. Hum Androl. 2015; 5:23–27.

43. Schwenkhagen A. Hormonal changes in menopause and implications on sexual health. J Sex Med. 2007; 4(Suppl 3):220–226. PMID: 17394594.

44. Nappi RE, Albani F, Santamaria V, Tonani S, Magri F, Martini E, et al. Hormonal and psycho-relational aspects of sexual function during menopausal transition and at early menopause. Maturitas. 2010; 67:78–83. PMID: 20554405.

45. González M, Viáfara G, Caba F, Molina E. Sexual function, menopause and hormone replacement therapy (HRT). Maturitas. 2004; 48:411–420. PMID: 15283933.

46. Nastri CO, Lara LA, Ferriani RA, Rosa-E-Silva AC, Figueiredo JB, Martins WP. Hormone therapy for sexual function in perimenopausal and postmenopausal women. Cochrane Database Syst Rev. 2013; (6):CD009672. PMID: 23737033.

47. Heidari M, Shahbazi S, Ghodusi M. Evaluation of body esteem and mental health in patients with breast cancer after mastectomy. J Midlife Health. 2015; 6:173–177. PMID: 26903758.
48. Heidari M, Ghodusi M. The relationship between body esteem and hope and mental health in breast cancer patients after mastectomy. Indian J Palliat Care. 2015; 21:198–202. PMID: 26009674.

49. Hakimi S, Aminian E, Alizadeh Charandabi SM, Bastani P, Mohammadi M. Risk factors of overactive bladder syndrome and its relation to sexual function in menopausal women. Urologia. 2018; 85:10–14. PMID: 29619902.

50. Park YJ, Kim HS, Chang SO, Kang HC, Chun SH. Sexuality and related factors of postmenopausal Korean women. Taehan Kanho Hakhoe Chi. 2003; 33:457–463. PMID: 15314420.

51. Guthrie JR, Dennerstein L, Taffe JR, Lehert P, Burger HG. The menopausal transition: a 9-year prospective populationbased study. The Melbourne Women's Midlife Health Project. Climacteric. 2004; 7:375–389. PMID: 15799609.

52. Blumel JE, Castelo-Branco C, Binfa L, Gramegna G, Tacla X, Aracena B, et al. Quality of life after the menopause: a population study. Maturitas. 2000; 34:17–23. PMID: 10687878.

53. Mezones-Holguin E, Córdova-Marcelo W, Lau-Chu-Fon F, Aguilar-Silva C, Morales-Cabrera J, Bolaños-Díaz R, et al. Association between sexual function and depression in sexually active, mid-aged, Peruvian women. Climacteric. 2011; 14:654–660. PMID: 21961836.

54. Yangin HB, Sözer GA, Sengün N, Kukulu K. The relationship between depression and sexual function in menopause period. Maturitas. 2008; 61:233–237. PMID: 18951735.

55. Graziottin A, Basson R. Sexual dysfunction in women with premature menopause. Menopause. 2004; 11:766–777. PMID: 15543028.

56. Bachmann GA, Leiblum SR. The impact of hormones on menopausal sexuality: a literature review. Menopause. 2004; 11:120–130. PMID: 14716193.

57. Omu AE, al-Qattan N. Effects of hormone replacement therapy on sexuality in postmenopausal women in a mideast country. J Obstet Gynaecol Res. 1997; 23:157–164. PMID: 9158303.

58. Nisar N, Ahmed Sohoo N. Severity of Menopausal symptoms and the quality of life at different status of Menopause: a community based survey from rural Sindh, Pakistan. Int J Collab Res Intern Med Public Health. 2010; 2:118–130.
59. García Padilla FM, López Santos V, Toronjo Gómez AM, Toscano Márquez T, Contreras Martín A. Evaluation of knowledge about climacteric in Andalusian women. Aten Primaria. 2000; 26:476–481. PMID: 11268549.
60. Nappi RE, Nijland EA. Women's perception of sexuality around the menopause: outcomes of a European telephone survey. Eur J Obstet Gynecol Reprod Biol. 2008; 137:10–16. PMID: 17207567.

61. da Fonseca AM, Cavalcanti AL, Bagnoli VR, da Paixão JS, Penteado SRL, Cardoso EB, et al. Effects of estradiol valerate associated with cyproterone acetate on some clinical and sexuality-related aspects in postmenopausal women. Einstein. 2008; 6:170–174.
62. Osinowo HO. Psychosocial factors associated with perceived psychological health, perception of menopause and sexual satisfaction in menopausal women and controls. West Afr J Med. 2003; 22:225–231. PMID: 14696946.

63. Elavsky S, McAuley E. Physical activity, symptoms, esteem, and life satisfaction during menopause. Maturitas. 2005; 52:374–385. PMID: 16198515.

64. Jokinen K, Rautava P, Mäkinen J, Ojanlatva A, Sundell J, Helenius H. Experience of climacteric symptoms among 42–46 and 52–56-year-old women. Maturitas. 2003; 46:199–205. PMID: 14585522.

65. Ishak IH, Low WY, Othman S. Prevalence, risk factors, and predictors of female sexual dysfunction in a primary care setting: a survey finding. J Sex Med. 2010; 7:3080–3087. PMID: 20584130.

66. Bolourian Z, Ganjloo J. Evaluating sexual dysfunction and some related factors in women attending Sabzevar Health Care Centers. J Reprod Infertil. 2007; 8:163–170.
67. Brynhildsen J, Hammar M. Low dose transdermal estradiol/norethisterone acetate treatment over 2 years does not cause endometrial proliferation in postmenopausal women. Menopause. 2002; 9:137–144. PMID: 11875333.

68. Shumaker SA, Legault C, Rapp SR, Thal L, Wallace RB, Ockene JK, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the Women's Health Initiative Memory Study: a randomized controlled trial. JAMA. 2003; 289:2651–2662. PMID: 12771112.

69. Lange-Collett J. Promoting health among perimenopausal women through diet and exercise. J Am Acad Nurse Pract. 2002; 14:172–179. PMID: 12001748.

70. Nascimento ER, Maia AC, Pereira V, Soares-Filho G, Nardi AE, Silva AC. Sexual dysfunction and cardiovascular diseases: a systematic review of prevalence. Clinics (Sao Paulo). 2013; 68:1462–1468. PMID: 24270960.

71. Doruk H, Akbay E, Cayan S, Akbay E, Bozlu M, Acar D. Effect of diabetes mellitus on female sexual function and risk factors. Arch Androl. 2005; 51:1–6. PMID: 15764412.

72. Afghari A, Ganji J, Ahmad Shirvani M. Psycho-emotional changes in menopause: a qualitative study. J Mazandaran Univ Med Sci. 2012; 22:27–38.
73. Borissova AM, Kovatcheva R, Shinkov A, Vukov M. A study of the psychological status and sexuality in middle-aged Bulgarian women: significance of the hormone replacement therapy (HRT). Maturitas. 2001; 39:177–183. PMID: 11514116.

74. Danaci AE, Oruç S, Adigüzel H, Yildirim Y, Aydemir O. Relationship of sexuality with psychological and hormonal features in the menopausal period. West Indian Med J. 2003; 52:27–30. PMID: 12806751.
75. Basson R. Women's sexual dysfunction: revised and expanded definitions. CMAJ. 2005; 172:1327–1333. PMID: 15883409.

76. Malacara JM, Canto de Cetina T, Bassol S, González N, Cacique L, Vera-Ramírez ML, et al. Symptoms at pre- and postmenopause in rural and urban women from three States of Mexico. Maturitas. 2002; 43:11–19. PMID: 12270577.

77. Dennerstein L, Dudley E, Burger H. Are changes in sexual functioning during midlife due to aging or menopause? Fertil Steril. 2001; 76:456–460. PMID: 11532464.

78. Gott M, Hinchliff S. How important is sex in later life? The views of older people. Soc Sci Med. 2003; 56:1617–1628. PMID: 12639579.

79. Ponholzer A, Roehlich M, Racz U, Temml C, Madersbacher S. Female sexual dysfunction in a healthy Austrian cohort: prevalence and risk factors. Eur Urol. 2005; 47:366–375. PMID: 15716203.

80. Hartmann U, Philippsohn S, Heiser K, Rüffer-Hesse C. Low sexual desire in midlife and older women: personality factors, psychosocial development, present sexuality. Menopause. 2004; 11:726–740. PMID: 15543025.

81. Pérez JA, Garcia FC, Palacios S, Pérez M. Epidemiology of risk factors and symptoms associated with menopause in Spanish women. Maturitas. 2009; 62:30–36. PMID: 19010615.

82. Tomic D, Gallicchio L, Whiteman MK, Lewis LM, Langenberg P, Flaws JA. Factors associated with determinants of sexual functioning in midlife women. Maturitas. 2006; 53:144–157. PMID: 16368468.

83. Addis IB, Van Den Eeden SK, Wassel-Fyr CL, Vittinghoff E, Brown JS, Thom DH. Sexual activity and function in middle-aged and older women. Obstet Gynecol. 2006; 107:755–764. PMID: 16582109.

84. Liu J, Eden J. Experience and attitudes toward menopause in Chinese women living in Sydney--a cross sectional survey. Maturitas. 2007; 58:359–365. PMID: 17980523.

85. Beutel ME, Schumacher J, Weidner W, Brähler E. Sexual activity, sexual and partnership satisfaction in ageing men--results from a German representative community study. Andrologia. 2002; 34:22–28. PMID: 11996178.

86. Kingsberg SA. The impact of aging on sexual function in women and their partners. Arch Sex Behav. 2002; 31:431–437. PMID: 12238611.
87. Lin TB. Sexuality and the menopause. Paper presented at: First Consensus Meeting on Menopause in the East Asian Region. Geneva, Swiss. 2013.
88. Wright LK. Affection and sexuality in the presence of Alzheimer's disease: a longitudinal study. Sex Disabil. 1998; 16:167–179.
89. Deacon S, Minichiello V, Plummer D. Sexuality and older people: revisiting the assumptions. Educ Gerontol. 1995; 21:497–513.

90. Meston CM, Levin RJ, Sipski ML, Hull EM, Heiman JR. Women's orgasm. Annu Rev Sex Res. 2004; 15:173–257. PMID: 16913280.
91. Palacios S, Tobar AC, Menendez C. Sexuality in the climacteric years. Maturitas. 2002; 43(Suppl 1):S69–S77. PMID: 12361890.

92. Alarslan D, Sarandol A, Cengiz C, Develioglu OH. Androgens and sexual dysfunction in naturally and surgically menopausal women. J Obstet Gynaecol Res. 2011; 37:1027–1034. PMID: 21481089.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download