1. Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001; 83(8):1119–1124. PMID:
11764423.
2. Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br. 1950; 32(2):183–186. PMID:
15422015.

3. Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. Berlin: Springer Verlag;1993. p. 364–369.
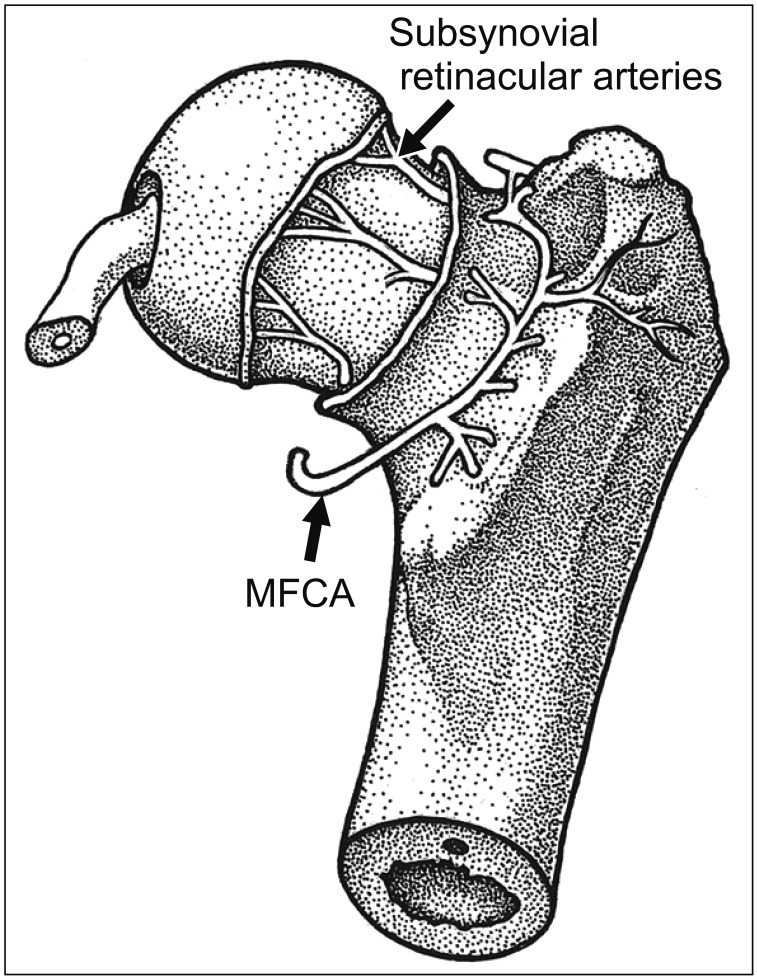
4. Gautier E, Ganz K, Krugel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000; 82(5):679–683. PMID:
10963165.

5. Watson-Jones R. Fractures of the neck of the femur. Br J Surg. 1936; 23(92):787–808.

6. Buess P, Morscher E. Osteotomy to lengthen the femur neck with distal adjustment of the trochanter major in coxa vara after hip dislocation. Orthopade. 1988; 17(6):485–490. PMID:
3217108.
7. Ribas M, Ledesma R, Cardenas C, Marin-Pena O, Toro J, Caceres E. Clinical results after anterior mini-open approach for femoroacetabular impingement in early degenerative stage. Hip Int. 2010; 20 Suppl 7:S36–S42. PMID:
20512770.

8. Ng VY, Arora N, Best TM, Pan X, Ellis TJ. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med. 2010; 38(11):2337–2345. PMID:
20489213.
9. Parvizi J, Huang R, Diaz-Ledezma C, Og B. Mini-open femoroacetabular osteoplasty: how do these patients do? J Arthroplasty. 2012; 27(8 Suppl):122–125.
10. Cohen SB, Huang R, Ciccotti MG, Dodson CC, Parvizi J. Treatment of femoroacetabular impingement in athletes using a mini-direct anterior approach. Am J Sports Med. 2012; 40(7):1620–1627. PMID:
22562788.

11. Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007; 15(7):908–914. PMID:
17479250.

12. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011; 27(10):1379–1388. PMID:
21862276.

13. Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011; 27(12):1720–1731. PMID:
22047925.

14. Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011; 39 Suppl:14S–19S. PMID:
21709027.

15. Alradwan H, Philippon MJ, Farrokhyar F, et al. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy. 2012; 28(10):1567–1576. PMID:
22795753.

16. Malviya A, Stafford GH, Villar RN. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J Bone Joint Surg Br. 2012; 94(4):466–470. PMID:
22434460.

17. Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Mid-term results of surgical treatment. Clin Orthop Relat Res. 2004; (418):67–73.
18. Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004; (429):178–181.
19. Beaule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007; 89(4):773–779. PMID:
17403799.
20. Yun HH, Shon WY, Yun JY. Treatment of femoroacetabular impingement with surgical dislocation. Clin Orthop Surg. 2009; 1(3):146–154. PMID:
19885050.

21. Kempthorne JT, Armour PC, Rietveld JA, Hooper GJ. Surgical dislocation of the hip and the management of femoroacetabular impingement: results of the Christchurch experience. ANZ J Surg. 2011; 81(6):446–450. PMID:
22295348.

22. Naal FD, Miozzari HH, Wyss TF, Notzli HP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011; 39(3):544–550. PMID:
21173196.

23. Papalia R, Del Buono A, Franceschi F, Marinozzi A, Maffulli N, Denaro V. Femoroacetabular impingement syndrome management: arthroscopy or open surgery? Int Orthop. 2012; 36(5):903–914. PMID:
22190060.

24. Sink EL, Fabricant PD, Pan Z, Dayton MR, Novais E. Results of treatment of femoroacetabular impingement in adolescents with a surgical hip dislocation approach. Clin Orthop Relat Res. 2013; 471(8):2563–2569. PMID:
23653097.

25. Shin SJ, Kwak HS, Cho TJ, et al. Application of Ganz surgical hip dislocation approach in pediatric hip diseases. Clin Orthop Surg. 2009; 1(3):132–137. PMID:
19885048.

26. Trueta J, Harrison MH. The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg Br. 1953; 35(3):442–461. PMID:
13084696.

27. Sevitt S, Thompson RG. The distribution and anastomoses of arteries supplying the head and neck of the femur. J Bone Joint Surg Br. 1965; 47(3):560–573. PMID:
14341080.

28. McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001; (393):25–37. PMID:
11764355.
29. Mintz DN, Hooper T, Connell D, Buly R, Padgett DE, Potter HG. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy. 2005; 21(4):385–393. PMID:
15800516.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download