This article has been
cited by other articles in ScienceCentral.
Abstract
Atypical fractures associated with prolonged bisphosphonate (BP) therapy rarely occur outside the femur, and the diagnostic criteria, appropriate treatment principles, and fixation methods for atypical ulnar fractures have not been established. The authors experienced the use of internal fixation with a metal plate and a new internal fixation method with an intramedullary nail in the treatment of an atypical ulnar fracture in a patient who had been on BP therapy for 10 to 20 years. This paper reports findings along with a review of the relevant literature.
Keywords: Ulna, Ulna atypical fracture, Osteoporosis, Bisphosphonate, Intra-medullary nail, Ender nail, Metal plate
Bisphosphonates (BPs) are the first choice and most commonly used drugs for osteoporosis. They increase bone density in the spine and femur and prevent vertebral or nonvertebral fractures. Since the first report of a subtrochanteric fracture without a trauma in a patient who had been taking BPs in 2005,
1) interest has increased in the side effects associated with prolonged BP use, especially with respect to atypical fractures.
However, atypical fractures rarely occur outside the femur; in particular, there are no reports of the fixation methods that are used during surgical treatment of atypical ulnar fractures and their effectiveness. We experienced two cases of patients with atypical ulnar fractures who had been taking BPs for over 10 years. One patient was treated with open reduction and fixation using a plate, and the other was treated with intramedullary nail fixation after closed reduction. Accordingly, we report the findings here and hope that clinicians will use these findings as guidelines for treating future cases of atypical ulnar fractures.
Case Reports
1. Case 1
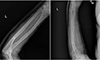
An 80-year-old female was admitted to Inje University Busan Paik Hospital for left elbow pain that occurred after lifting something heavy three days prior to admission. She had hypertension and osteoporosis as underlying diseases. She was diagnosed with osteoporosis at a local clinic 20 years ago and had since been under a treatment regimen of ibandronate injections, in 3-month intervals, with 1 to 2 year drug holiday after 5 years of medication. She did not present prodromal symptoms and was found to have direct tenderness in her left proximal forearm on physical examination. The X-rays that were taken during her first visit showed a transverse fracture without displacement in the proximal third of the shaft (
Fig. 1).
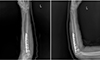
Her blood calcium level was 9.2 mg/dl (8.6–10.4 mg/dl), and her phosphorus level was 2.7 mg/dl (2.6–4.4 mg/dl). Her 1,25-dihydroxyvitamin D3 level was 27.2 pg/ml (19.6–54.3 pg/ml) and her C-telopeptide level was 0.264 ng/ml (premenopausal<0.573 ng/ml, postmenopausal<1.008 ng/ml). Her bone mineral density (BMD) T-score was 0.6 in the vertebra and −2.1 in the femoral neck. Three days after her first visit, open reduction and internal fixation of the ulnar fracture was performed using metal plates (
Fig. 2). After the surgery, BP was discontinued, and a parathyroid hormone (PTH) injection was administered. Her forearm was immobilized using a cast with her elbow neutrally flexed to 90° for three weeks. One year and two months after surgery, the callus formation, indicating early fracture union (
Fig. 3). She completely recovered her elbow range of motion at 16 months.
2. Case 2
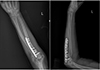
A 77-year-old female had been diagnosed with osteoporosis 10 years ago at a local clinic and had been taking risedronate, which contained nitrogen (risedronate Sodium Tab., 150 mg once a month, and 5 years after her first treatment, she was offered a “drug holiday” of 2 years). Since then, she complained of pain and swelling in the left forearm for 3 months, before visiting the clinic. She reported a cracking sound that occurred as she lifted herself up from a chair using her left hand on the day of the visit. She had pressure, pain, and swelling over her left proximal ulna on physical examination. The X-rays showed a transverse ulnar fracture in the proximal third of the shaft, without displacement (
Fig. 4). Her blood calcium level was 9.5 mg/dl (8.6–10.4 mg/dl) and her phosphorus level was 2.7 mg/dl (2.6–4.4 mg/dl). Her 1,25-dihydroxyvitamin D
3 level was 45.7 (19.6–54.3 pg/ml) and her C-telopeptide level was 0.234 ng/ml (premenopausal<0.573 ng/ml, postmenopausal<1.008 ng/ml). Her BMD T-scores were 1.4 in the vertebra and −1.4 in the femoral neck. After a diagnosis of knee arthritis, a local clinic prescribed steroids for 6 months. The patient's skin was thin and lacked elasticity. Because of concerns regarding wound healing after surgical treatment of the ulnar fracture, closed reduction and internal fixation using intramedullary nails was performed 2 weeks later (
Fig. 5). After the surgery, she was prescribed a PTH injection (teriparatide, 20 µg daily), in addition to calcium and vitamin D, and the BP was discontinued. Her forearm was immobilized, with the elbow extended for 8 weeks.
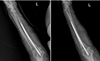
Nine months of the surgery, although the pain reduced, callus formation was not observed and displacement was found (
Fig. 6). The patient complained of a continuous sense of pressure at the fracture site and was informed about the possibility of nonunion. Since bone union had not taken place, additional surgery was planned.
Discussion
The patient in case 1, with an atypical ulnar fracture, showed union at the fracture site 14 months after open reduction and internal fixation using metal plates and has maintained usual activities, without pain.
In case 2, closed reduction and internal fixation using intramedullary nails was performed. Closed reduction and internal fixation was performed through a small soft tissue incision, without exposing the fracture while conserving the periosteum. Therefore, the procedure may be performed when blood flow can be preserved and the soft tissues are in poor condition. With respect to treatment choices for atypical femoral fractures, the method that uses open reduction and internal fixation with a metal plate tends to have a higher frequency of complications, such as infection and nonunion, than the method that uses closed reduction and intramedullary fixture. The metal plate method is also known to have a negative impact on bone union because of extensive dissection of the soft tissue and periosteum. Accordingly, the closed reduction and intramedullary nail fixation method is commonly used to treat femoral fractures because of the reduced dissection that is required and since biological bone graft effects can be achieved by reaming.
In case 2, intramedullary nails were inserted. However, ulnar intramedullary reaming was difficult, in contrast to insertion into the proximal femur. The results were inadequate, because the medullary cavity was too narrow and curved. Consequently, it was difficult to expect adequate effects of the intramedullary nail fixation because of difficulty with intramedullary reaming. As a result, callus formation may not have developed in this patient because of the absence of hematomas and an inflammatory phase.
The ulna is brittle, has a low bone turnover rate, and lacks the ability to heal when affected by atypical fractures; Therefore, open reduction and internal fixation using metal plates is considered more advisable than use of intramedullary nails for treatment of atypical fractures. The problematic anatomical structure also affects the healing of other common ulnar fractures. Ceasing the use of BPs is necessary to prevent atypical fractures. Although there is no consensus regarding the length of time BPs should be avoided, ceasing use or decreasing the dose should be considered if BMD values have increased to a certain level. Clinicians should be aware that atypical ulnar fractures can develop as a result of long-term use of BPs; In addition, patients should be informed of the problems associated with the long-term use of osteoporosis medications, and forearm pain should be evaluated.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download