Abstract
Purpose
To compare the effects of bifocal versus trifocal diffractive intraocular lens (IOL) implantation on visual quality after phacoemulsification in patients with cataracts.
Methods
Eighty-eight eyes from 63 patients were analyzed. Trifocal (AT LISA tri 839MP), bifocal (AcrySof IQ ReSTOR) and bifocal (Tecnis MF ZLB00) IOLs were implanted into 53, 18, and 17 eyes, respectively. Uncorrected distance, intermediate and near visual acuity, refractive errors, contrast sensitivity, and patient satisfaction were measured at 1 week and 1 month after surgery. Refractive error was converted to a spherical equivalent and compared to predicted refraction calculated by IOL calculation formulas.
Results
Uncorrected distance, intermediate, and near visual acuity did not differ significantly between groups. One month after surgery, the mean refractive errors were −0.07 diopters (D) in the AT LISA tri 839MP group, +0.18 D in the AcrySof IQ ReSTOR group, and +0.31 D in the Tecnis MF ZLB00 group (p < 0.001). The predictive accuracy of IOL calculation formulas did not differ between groups. Contrast sensitivity, satisfaction, and spectacle independence in the trifocal group were comparable with those of the two bifocal groups.
With improvements in cataract surgery technique and intraocular lenses (IOL) technologies, patients presenting for cataract surgery expect to have good vision at distance and near ranges without using spectacles. However, standard IOLs are monofocal and offer only fixed focal distance. At different object distances, blur will occur [1]. Patients usually remain presbyopic in monofocal pseudophakic eyes due to this lack of accommodation. This problem can be partly resolved by using multifocal IOLs, because multifocal IOLs provide better near or intermediate visual acuity than monofocal IOLs [234].
Multifocal IOLs generate different foci to overcome visual limitations at near and intermediate distances that occur with classic monofocal IOLs. Multifocal IOLs provide good distance and near functional vision without requiring corrective lenses [5678]. However, some optical side effects have been reported, including decreased contrast sensitivity (CS), glare disability, and halos [391011], which can significantly affect visual performance and patient satisfaction.
At present, most multifocal IOLs are bifocal with only near and far foci. Visual quality for intermediate viewing activities such as computer use might be insufficient for daily life [121314]. Trifocal IOLs, which allow functional distance, intermediate, and near vision, have recently been introduced to overcome weaknesses of intermediate vision associated with bifocal IOLs [151617]. However, experimental studies and clinical studies have shown inconsistent results at distance, intermediate, and near focal points [131819].
In this study, we compared the visual and refractive outcomes of bifocal versus trifocal diffractive IOL implantation after phacoemulsification in patients with cataracts.
This study adhered to the tenets of the Declaration of Helsinki for the use of human participants in biomedical research. It was approved by the institutional review board of Seoul National University Hospital and Seoul National University Bundang Hospital (1708-108-879, B-1710/424-401). We retrospectively reviewed the medical records of patients who underwent cataract surgery from November 2009 to April 2017. Patient demographic data such as age, gender, laterality of the operated eye, preoperative corrected distance visual acuity, and distance-corrected intermediate and near visual acuity were collected.
Cataract patients who underwent uneventful phacoemulsification and multifocal IOL implantation during the study period were included in the sample. Those with histories of trauma, corneal opacity, and severe dry eye were excluded. Cases with intraoperative complications were also excluded.
Autokeratometry (KR-8900; Topcon, Tokyo, Japan), optical biometry (IOLMaster; Carl Zeiss Meditec, Jena, Germany) and topography (Orbscan IIz, Bausch & Lomb, Rochester, NY, USA; Atlas 9000, Carl Zeiss Meditec) were used for preoperative corneal power measurements. Axial length measurements were obtained using an IOLMaster with partial coherence tomography. The implanted IOL power was determined using the IOLMaster (n = 83) or A-scan (Axis II PR; Quantel Medical, Cournon d'Auvergne, France) (n = 5) to measure axial length and corneal refractive power.
Two surgeons (MKK and JYH) performed all cataract surgeries by standard phacoemulsification with IOL implantation using the same measurement and surgical instruments. Surgical procedures were performed with an on-astigmatic axis clear corneal incision. Eye drops with 0.5% levofloxacin (Cravit; Santen, Osaka, Japan) and 0.1% fluorometholone (Flarex; Alcon Laboratories, Fort Worth, TX, USA) were instilled four times daily for 4 weeks. Follow-up examinations were performed at 1 day, 1 week, and 1 month after surgery.
AT LISA tri 839MP (Carl Zeiss Meditec, add power +3.33 D/+1.66 D), AcrySof IQ ReSTOR SN6AD1, or SND1T# (Alcon Laboratories, add power +3.0 D), or Tecnis MF ZLB00 (Abbott Medical Optics, Abbott Park, IL, USA; add power +3.25 D) IOLs were implanted.
Postoperative uncorrected distance visual acuity (UDVA), uncorrected intermediate visual acuity (UIVA), and uncorrected near visual acuity (UNVA), respectively, were assessed 1 and 4 weeks after the surgery. Distance visual acuity was measured using a 5-m Hahn's visual acuity chart (Hahn Chun Suk test chart). Intermediate and near visual acuities were measured using Logarithmic Visual Acuity Chart 2000 New ETDRS Chart 1 (Precision Vision, La Salle, IL, USA).
Objective refractive spherical and cylindrical powers were examined by autokeratometry (KR-8900) before and after surgery and converted to spherical equivalent (SE). Mean numerical error (MNE) was defined as the value obtained by subtracting the target refractive power calculated by IOL formulas from postoperative SE. Mean absolute error (MAE) was defined as the absolute value of the difference between actual and predictive refractive error. Both MNE and MAE were assessed at 4 weeks after surgery. The refractive error was converted to SE and compared to the expected refraction obtained from IOL calculation formulas. MNE was the actual postoperative SE minus predicted SE while MAE was the average absolute value of MNE. A negative MNE indicated that the patient had a postoperative refraction that was more myopic than intended while a positive MNE indicated that the patient had more hyperopic refraction than intended.
IOL power was determined to be the target diopter closest to emmetropia after surgery considering axial length and depth of the anterior chamber measured by the IOL-Master or in unavailable cases (n = 5) by contact A-scan ultrasonography using SRK-T, Haigis, Hoffer Q, Holladay, and Barrett formulas.
CS testing was performed using a Vision Contrast Test System (VCTS 6500; Vistech Consultants, Dayton, OH, USA) under mesopic conditions (3 cd/m2) with only dim light at a chart luminance of 220 Lux. The testing distance was 3 m. Monocular measurements were carried out at 1 month after surgery without correction. CS was tested at spatial frequencies of 1.5, 3, 6, 12, or 18 cycles per degree (cpd).
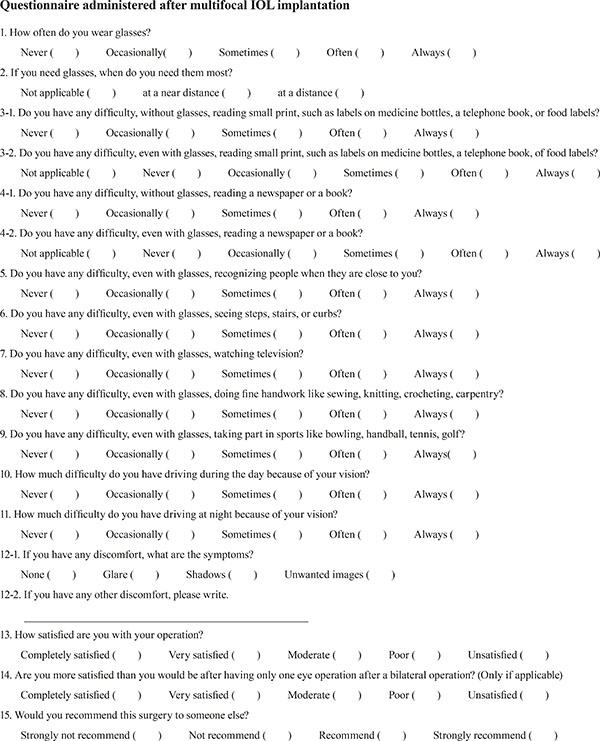
One month postoperatively, patient satisfaction was evaluated with a modified Korean version of the Visual Function Index (VF-14) questionnaire (Appendix 1). Reasons for dissatisfaction and dependence on wearing glasses were investigated. Satisfaction and necessity of wearing glasses were scored on a scale from 0 to 4 points.
Decimal visual acuity was converted to logarithm of the minimal angle of resolution (logMAR) scale for statistical analyses. All CS data were transformed to logarithmic units and logCS values were compared in each group. All continuous data were expressed as mean ± standard deviation of the mean. Statistical analysis was performed with IBM SPSS Statistics ver. 22.0 (IBM Corp., Armonk, NY, USA). Statistical analyses of quantitative data, including descriptive statistics, were performed for all items. Categorical variables were compared using Fisher's exact test. The Kruskal-Wallis test was used to compare results among the three IOL groups. For post hoc analysis, Mann-Whitney U-test with Bonferroni adjustment was used to avoid experimental error. A p-value less than 0.05 was considered statistically significant.
Eighty-eight eyes from 63 patients were analyzed, including 33 (52.4%) female patients. The mean age of patients at the time of cataract surgery was 57.93 ± 12.04 years. Of 88 eyes, 53 eyes (60.2%) from 40 patients were implanted with trifocal IOLs (AT LISA tri 839MP), 18 eyes (20.5%) from 11 patients were implanted with bifocal IOLs (AcrySof IQ ReSTOR), and 17 eyes (19.3%) from 12 patients were implanted with bifocal IOLs (Tecnis MF ZLB00). Patient demographics and clinical data are summarized in Table 1.
Mean UDVA (logMAR) at 1 week after surgery was 0.03 ± 0.10 in the AT LISA tri 839MP group, 0.09 ± 0.15 in the AcrySof IQ ReSTOR group, and 0.08 ± 0.12 in the Tecnis MF ZLB00 group. There were no significant differences among groups (p = 0.229) (Table 2). Mean UDVA (logMAR) at 1 month after the surgery was 0.05 ± 0.08 in the AT LISA tri 839MP group, 0.06 ± 0.10 in the AcrySof IQ ReSTOR group, and 0.09 ± 0.09 in the Tecnis MF ZLB00 group (p = 0.327) (Table 2). There were no statistically significant differences in UDVA, UIVA, or UNVA among the three groups at either 1 or 4 weeks following surgery.
Fig. 1A and 1B shows percentages of eyes with logMAR uncorrected visual acuities better than 0, 0.1, and 0.3 in patients with different multifocal IOLs. One week after surgery, 49.1% of the AT LISA tri 839MP group, 22.2% of the AcrySof IQ ReSTOR group, and 47.1% of the Tecnis MF ZLB00 group had logMAR UDVA better than 0 (Snellen equivalent: 20 / 20). Four weeks after surgery, 45.3% of the AT LISA tri 839MP group, 33.3% of the AcrySof IQ ReSTOR group, and 41.2% of the Tecnis MF ZLB00 group had logMAR UDVA better than 0 (20 / 20) (Fig. 1).
One week after surgery, the mean spherical equivalents were −0.30 diopters (D) in the AT LISA tri 839MP group, −0.04 D in the AcrySof IQ ReSTOR group, and +0.18 D in the Tecnis MF ZLB00 group (p < 0.001) (Fig. 2A). One month after surgery, the mean spherical equivalents were −0.07 D in the AT LISA tri 839MP group, +0.18 D in the AcrySof IQ ReSTOR group, and +0.31 D in the Tecnis MF ZLB00 group (p < 0.001) (Fig. 2B). Patients with AT LISA tri 839MP insertion showed significant myopia tendencies compared to those with Tecnis MF ZLB00 insertion at 1 and 4 weeks postoperatively (p < 0.001 at both 1 and 4 weeks) (Fig. 2). Patients with AT LISA tri 839MP insertion showed significant myopia tendencies compared to those with AcrySof IQ ReSTOR insertion only at 4 weeks postoperatively (p = 0.011) (Fig. 2).
The predictive accuracy of formulas was analyzed by comparing MNE and MAE of the refractive error. MNE and MAE of all five IOL calculation formulas (SRK-T, Haigis, Hoffer Q, Holladay, and Barrett equations) for each IOL at one month after the surgery were compared (Table 3). There were no significant differences in results obtained with different IOL calculation formulas (Fig. 3A, 3B).
CS values of trifocal and bifocal IOL groups were comparable. There were no significant differences among the three groups at any spatial frequencies except 6 cpd (p = 0.005) (Table 4 and Fig. 4). The CS value of the Tecnis MF ZLB00 group at 6 cpd was significantly decreased compared to that of the AcrySof IQ ReSTOR group (p = 0.004).
Differences in satisfaction or rates of spectacle independence between groups were not significant (Fig. 5).
In this study, the visual performance of trifocal IOL was compared to that of two different bifocal IOLs. We found that all three different multifocal IOLs achieved satisfactory UDVA, UIVA, and UNVA without showing significant differences. The trifocal IOL and both bifocal IOLs showed comparable visual acuities. In general, previous studies evaluating diffractive trifocal IOLs have similarly shown good distance, intermediate, and near visual acuity [2021222324]. In comparison, Mojzis et al. [15] compared visual outcomes of 60 eyes of 30 patients who were bilaterally implanted with diffractive trifocal AT LISA tri 839MP or diffractive bifocal AT LISA 801 IOL and reported that intermediate visual acuities in diffractive trifocal IOL were better than those with bifocal IOL. Corrections of both spherical and longitudinal chromatic aberrations are important for visual acuity [25]. Most on-bench studies are performed in monochromatic light [2627]. Since the real world is polychromatic, experimental results may not capture real-world variation in visual quality analysis. In a previous study of other diffractive trifocal IOLs, objective and subjective longitudinal chromatic aberrations showed differences [28]. We hypothesize that these aberrations may have affected the visual outcomes of trifocal IOL implantation, which did not show superior performance compared to bifocal IOLs at intermediate distances.
Before surgery, there were no significant differences among the three IOL groups except for preoperative astigmatism, which was significantly greater in the AcrySof IQ ReSTOR group than in the AT LISA tri 839MP group or the Tecnis MF ZLB00 group. This result might be due to the inclusion of AcrySof IQ ReSTOR Toric IOL patients.
Although postoperative refractive error in the two bifocal IOL groups did not differ significantly, the postoperative refractive error of the trifocal IOL group was more likely to show myopic tendencies compared to the bifocal IOL groups at 1 month after cataract surgery.
Since postoperative refractive errors were important for satisfaction in patients with multifocal IOLs, the predictive accuracies of formulas were analyzed by comparing the MNE and MAE of refractive error. There were no significant differences among the five IOL calculation formulas (SRK-T, Haigis, Hoffer Q, Holladay, and Barrett equations) used in this study.
It was previously noted that the addition of a third focal point with implantation of trifocal IOL may increase halos. However, it is unlikely to increase visual disturbances or reduce mesopic CS function compared to bifocal IOLs [293031]. In our study, trifocal IOL and bifocal IOLs showed comparable postoperative CS. At 6 cpd, the CS value of the Tecnis MF ZLB00 group was significantly decreased compared to that of the AcrySof IQ ReSTOR group. Studies of CS with defocus show that the optimum focus is dependent on spatial frequency [32]. In addition, AcrySof IQ ReSTOR IOL and Tecnis MF ZLB00 IOL have different add powers, the former being +3.00 D and the latter being +3.25 D. Low add power multifocal IOLs are associated with fewer concentric diffractive rings, which may result in fewer aberrations and incidences of postoperative visual disturbances.
Patient satisfaction was assessed by a modified Korean version of the VF-14 questionnaire. Our study showed that patient satisfaction was not significantly different among the three IOL groups, consistent with the results of previous studies documenting comparable levels of satisfaction between trifocal and bifocal groups [131416].
The main limitation of this study was that the postoperative observation period was short (1 month). Nevertheless, the results of our study are meaningful, since previous studies showed similar results at one month and three months after surgery [333435]. It is also meaningful to evaluate early visual performance and adverse reactions at one month. Second, there were differences in the numbers of patients in each group, which might have reduced the statistical power of our analysis because it was a retrospective study. Third, two surgeons conducted surgeries. This might have affected our outcome analysis due to surgeon-related factors. However, all procedures were standardized, from clear corneal incision to intracapsular IOL insertion. Thus, such factors should have negligible impacts on study outcomes. Last, IOL type was not randomized, since different IOLs were introduced during the study period. Nevertheless, the results of our study agree with those of previous studies, and provide new information about preferable IOL calculation formulas for each type of IOL.
In conclusion, trifocal and two different bifocal IOLs had comparable visual performances. Postoperative refractive errors show myopic tendencies after implantation of AT LISA tri 839MP and slight hyperopic tendencies after implantation of AcrySof IQ ReSTOR and Tecnis MF ZLB00.
Figures and Tables
 | Fig. 1Percentages of eyes with logarithm of the minimal angle of resolution uncorrected visual acuities better than 0, 0.1, and 0.3 (Snellen equivalent: 20 / 20, 20 / 25, and 20 / 40) with different multifocal intraocular lenses at (A) 1 week and (B) 1 month after surgery. UDVA = uncorrected distant visual acuity; UIVA = uncorrected intermediate visual acuity at an 80-cm distance; UNVA = uncorrected near visual acuity at a 40-cm distance. |
 | Fig. 2Postoperative mean spherical equivalent at (A) 1 week and (B) 1 month after surgery. The AT LISA tri 839MP group showed myopic tendencies compared to the AcrySof IQ ReSTOR and Tecnis MF ZLB00 groups. A p-value was determined using Mann-Whitney U-tests. IOL = intraocular lens. |
 | Fig. 3Predictive accuracy of five intraocular lens (IOL) calculation formulas in different multifocal IOL groups. (A) Comparison of mean numerical error (MNE). MNE was the actual postoperative spherical equivalent minus predicted spherical equivalent. (B) Comparison of mean absolute error (MAE). MAE was the average absolute value of MNE. |
 | Fig. 4Contrast sensitivity (CS) at five spatial frequencies in patients implanted with different multifocal intraocular lenses (IOLs) at 1 month postoperatively. The results for the AT LISA tri 839MP group were comparable to those of the two bifocal IOL groups. The bar represents standard deviation. A p-value was determined using Kruskal-Wallis tests. |
 | Fig. 5Patient-reported satisfaction and spectacle independence after implantations of different multifocal intraocular lenses (IOLs). Satisfaction was scored from 0 to 4 points (4 = completely satisfied, 3= very satisfied, 2 = moderate, 1 = poor, 0 = unsatisfied). Necessity of wearing glasses was scored from 0 to 4 points (4 = never, 3 = occasionally, 2 = sometimes, 1 = often, 0 = always). The bar represents standard deviation. |
Table 1
Demographic and clinical data of patients undergoing multifocal IOL implantation

Values are presented as mean ± standard deviation or number; Continuous variables were assessed with Kruskal-Wallis tests while categorical data (sex) were assessed with Fisher's exact tests.
IOL = intraocular lens; SE = spherical equivalent; CDVA = corrected distance visual acuity; DCIVA = distance-corrected intermediate visual acuity at an 80-cm distance; DCNVA = distance-corrected near visual acuity at a 40-cm distance.
Table 2
Uncorrected distance, intermediate visual acuity and near visual acuity for subjects with diffractive multifocal intraocular lenses at 1 week and 1 month after surgery

References
1. Martinez Palmer A, Gomez Faina P, Espana Albelda A, et al. Visual function with bilateral implantation of monofocal and multifocal intraocular lenses: a prospective, randomized, controlled clinical trial. J Refract Surg. 2008; 24:257–264.

2. Agresta B, Knorz MC, Kohnen T, et al. Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: a systematic review. J Refract Surg. 2012; 28:426–435.

3. Leyland M, Zinicola E. Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology. 2003; 110:1789–1798.
4. Souza CE, Muccioli C, Soriano ES, et al. Visual performance of AcrySof ReSTOR apodized diffractive IOL: a prospective comparative trial. Am J Ophthalmol. 2006; 141:827–832.

5. Alio JL, Elkady B, Ortiz D, Bernabeu G. Clinical outcomes and intraocular optical quality of a diffractive multifocal intraocular lens with asymmetrical light distribution. J Cataract Refract Surg. 2008; 34:942–948.
6. Kohnen T, Allen D, Boureau C, et al. European multicenter study of the AcrySof ReSTOR apodized diffractive intraocular lens. Ophthalmology. 2006; 113:584.e1.

7. Alio JL, Tavolato M, De la Hoz F, et al. Near vision restoration with refractive lens exchange and pseudoaccommodating and multifocal refractive and diffractive intraocular lenses: comparative clinical study. J Cataract Refract Surg. 2004; 30:2494–2503.
8. Yoshino M, Bissen-Miyajima H, Minami K, Taira Y. Five-year postoperative outcomes of apodized diffractive multifocal intraocular lens implantation. Jpn J Ophthalmol. 2013; 57:510–513.

9. Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009; 35:992–997.

10. Montes-Mico R, Alio JL. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J Cataract Refract Surg. 2003; 29:703–711.
11. Pieh S, Lackner B, Hanselmayer G, et al. Halo size under distance and near conditions in refractive multifocal intraocular lenses. Br J Ophthalmol. 2001; 85:816–821.

12. Bilbao-Calabuig R, Gonzalez-Lopez F, Amparo F, et al. Comparison between mix-and-match implantation of bifocal intraocular lenses and bilateral implantation of trifocal intraocular lenses. J Refract Surg. 2016; 32:659–663.

13. Gundersen KG, Potvin R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin Ophthalmol. 2016; 10:455–461.
14. Cochener B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J Refract Surg. 2016; 32:146–151.

15. Mojzis P, Kukuckova L, Majerova K, et al. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg. 2014; 30:666–672.

16. Jonker SM, Bauer NJ, Makhotkina NY, et al. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015; 41:1631–1640.

17. Voskresenskaya A, Pozdeyeva N, Pashtaev N, et al. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1299–1306.

18. Madrid-Costa D, Ruiz-Alcocer J, Ferrer-Blasco T, et al. Optical quality differences between three multifocal intraocular lenses: bifocal low add, bifocal moderate add, and trifocal. J Refract Surg. 2013; 29:749–754.

19. Montes-Mico R, Madrid-Costa D, Ruiz-Alcocer J, et al. In vitro optical quality differences between multifocal apodized diffractive intraocular lenses. J Cataract Refract Surg. 2013; 39:928–936.
20. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013; 39:343–349.

21. Law EM, Aggarwal RK, Kasaby H. Clinical outcomes with a new trifocal intraocular lens. Eur J Ophthalmol. 2014; 24:501–508.

22. Mojzis P, Pena-Garcia P, Liehneova I, et al. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014; 40:60–69.

23. Cochener B, Vryghem J, Rozot P, et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012; 6:1421–1427.

24. Kohnen T, Titke C, Bohm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removal. Am J Ophthalmol. 2016; 161:71–77.
25. Schwarz C, Canovas C, Manzanera S, et al. Binocular visual acuity for the correction of spherical aberration in polychromatic and monochromatic light. J Vis. 2014; 14:DOI: 10.1167/14.2.8.

26. Vega F, Alba-Bueno F, Millan MS. Energy distribution between distance and near images in apodized diffractive multifocal intraocular lenses. Invest Ophthalmol Vis Sci. 2011; 52:5695–5701.

27. Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013; 39:1093–1099.

28. Vinas M, Gonzalez-Ramos A, Dorronsoro C, et al. In vivo measurement of longitudinal chromatic aberration in patients implanted with trifocal diffractive intraocular lenses. J Refract Surg. 2017; 33:736–742.

29. Gundersen KG, Potvin R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol. 2016; 10:805–811.
30. Carson D, Hill WE, Hong X, Karakelle M. Optical bench performance of AcrySof((R)) IQ ReSTOR((R)), AT LISA((R)) tri, and FineVision((R)) intraocular lenses. Clin Ophthalmol. 2014; 8:2105–2113.
31. Plaza-Puche AB, Alio JL, Sala E, Mojzis P. Impact of low mesopic contrast sensitivity outcomes in different types of modern multifocal intraocular lenses. Eur J Ophthalmol. 2016; 26:612–617.

32. Green DG, Campbell FW. Effect of focus on the visual response to a sinusoidally modulated spatial stimulus. J Opt Soc Am. 1965; 55:1154–1157.

33. Tan N, Zheng D, Ye J. Comparison of visual performance after implantation of 3 types of intraocular lenses: accommodative, multifocal, and monofocal. Eur J Ophthalmol. 2014; 24:693–698.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download