Abstract
Purpose
Surgeons may be uncertain about the optimal timing of appendectomy to decrease complications, especially for complicated appendicitis. The aim of the study was to compare clinical outcomes between early and late surgery for complicated appendicitis.
Methods
A prospectively maintained database of complicated appendicitis was queried. Elective interval surgery (EIS) group and early surgery (ES) were matched with propensity score and marked with a prefix ‘p.’ Patient characteristics and surgical outcomes were compared.
Results
The propensity score-matched EIS group had a lower chance to underwent ileo-cecectomy or right hemicolectomy (1.5% vs. 6.9%, P = 0.031), a tendency of lower rate of postoperative complication (6.9% vs. 13.7%, P = 0.067), a lower rate of wound infection (1.5% vs. 8.4%, P = 0.010), and shorter postoperative hospital stay (3.72 days vs. 5.82 days, P < 0.001) than the propensity score-matched ES group. Multivariate analysis showed that delayed surgery for more than 48 hours or urgent surgery due to failure of EIS and open conversion were independent risk factors for postoperative complications (P = 0.001 and P = 0.025, respectively). In subgroup analysis, high American Society of Anesthesiologists physical status classification and distant abscess or generalized ascites in initial CT increased the risk of failure of EIS.
Appendicitis is one of the most common diseases requiring emergency operation after the onset of symptoms [1]. It is generally accepted that prompt surgery is necessary to prevent disease progression which is associated with an increased risk of morbidity and mortality [2]. Recently, however, the timing for performing emergency operations for nonlife-threatening diseases has been under scrutiny because of new insights into the natural history of acute appendicitis due to developments in imaging and antibiosis that can improve preoperative assessment and treatment, allowing for nonoperative management of abscesses and phlegmons and potentially limiting the need for immediate operative intervention to halt disease progression [3].
The concept of the necessity of emergency operation for complicated appendicitis has been challenged by recent studies reporting semi-elective surgery after initial use of antibiotics [45]. In addition, several studies have reported that the administration of antibiotics alone enables surgeons to perform interval appendectomy at up to 6–8 weeks after the diagnosis of appendicitis [67]. However, such treatment of complicated appendicitis that might progress to abscess or generalized peritonitis without operative intervention remains controversial. A recent study has found that a substantial percentage of patients with suspected acute complicated appendicitis and a plan for interval appendectomy require unplanned readmission [8]. Additionally, 2 randomized control trials have demonstrated that patients undergoing immediate appendectomy have quicker return to normal activity, fewer adverse events, and lower cost to the system compared to those with late appendectomy [910]. A separate randomized trial enrolling only children with an appendiceal abscess has mixed findings in terms of clinical parameters when comparing early to late appendectomy [11].
Despite emerging data favoring early appendectomy, no consensus exists on the optimal management for complicated appendicitis in adults. In addition, practice patterns continue to vary dramatically. This might be partially due to the fact that most studies on this topic were single-center studies with small sample sizes and limited follow-up periods. Thus, the purpose of the present study was to compare surgical outcomes of early versus late surgical management for complicated appendicitis using a large-scale multicenter database, and to find the criteria to choose late surgical management.
A prospectively maintained database containing data for affected individuals who underwent surgery for complicated appendicitis was queried to evaluate the role of clinical and serologic markers with clinical phenotypes in acute appendicitis. We retrospectively reviewed medical records of all patients who were diagnosed with complicated appendicitis and underwent surgery at 2 hospitals (Hallym University Dongtan Sacred Heart Hospital and Hallym University Kangnam Sacred Heart Hospital) affiliated to Hallym University, Korea between January 2013 and June 2019. Complicated appendicitis was defined as gangrenous, perforated appendicitis, and periappendiceal abscess formation, and when there is a mention of perforation on formal reading of CT scan. Patients underwent either laparoscopic, single-port laparoscopic or open surgery.
We included patients older than 18 years in this study. We excluded patients who underwent incidental appendectomy or negative appendectomy and those who were diagnosed with dysplasia or cancer.
Patients' characteristics included age, gender, and American Society of Anesthesiologists (ASA) physical status classification at initial diagnosis. CT scan was performed for diagnosis. CT finding was described based on modified Hinchey classification of diverticulitis [12]: Grade Ia, appendiceal wall thickening with periappendiceal soft tissue change; Grade Ib, Ia + periappendiceal abscess or ileo or cecal edema; grade II, Ia + distant abscess (generally deep in the pelvis or interloop regions); and grade III, free gas associated with localized or generalized ascites and possible peritoneal wall thickening.
Perioperative data included postoperative hospital stay, postoperative complications, cost for surgical treatment, and total cost. The ‘cost for surgical treatment’ was defined as total cost of admission for surgery while ‘total cost’ was defined as the total sum of cost for surgical treatment and cost of 1st admission for antibiotics.
Patients were divided into 2 groups according to the timing of surgery after hospital admission: (1) early surgery (ES) group, having surgery within 2 days during index admission; and (2) late surgery (LS) group, having surgery at more than 2 days after admission, whether during index admission or at subsequent one. Surgeons decided whether each patient would receive ES or LS, considering disease severity and condition of patient. We subdivided the LS group into 3 subgroups: patients who had surgery delayed more than 48 hours but during index admission (urgent > 48 hours), those who had surgery at urgent subsequent admission (failure of EIS), and those who had surgery on a planned date during an elective subsequent admission called elective interval surgery (EIS) (Fig. 1). In the EIS group, intravenous (IV) antibiotics were administered during index admission and oral antibiotics were prescribed after discharge. The most commonly used IV antibiotics were a combination of second-generation cephalosporin (cefuroxime) and metronidazole. Third-generation cephalosporin (ceftriaxone or cefotaxime) was used for cases with severe inflammation. If a patient was allergic to cephalosporin antibiotics, ciprofloxacin was administered. Prescribed oral antibiotics were either second generation (cefaclor) or third generation (cefditoren) cephalosporin. Occasionally, metronidazole was added if needed. Total duration of antibiotic use was about 2 weeks or more. Interval appendectomy was performed in 4 to 8 weeks after the initial presentation.
Operative types were classified as appendectomy, cecectomy, and ileo-cecectomy or right hemicolectomy. Postoperative complications were defined as wound infection, postoperative ileus, intra-abdominal abscess, or gastroenteritis occurring up to 30 days after surgical treatment, and they were also graded using the Clavien-Dindo classification [13].
For comparison of peri- and postoperative outcomes between the EIS group and the ES group, propensity score matching was performed. The propensity score-matched EIS (pEIS) group was then compared to the propensity score-matched ES (pES) group.
The first aim of this study was to compare surgical outcomes of the pEIS group and the pES group. The second aim was to identify risk factors associated with postoperative complications.
The study was reviewed and approved by the Institutional Review Boards (IRB) of Kangnam Sacred Heart Hospital (Seoul, Republic of Korea) (approval number: 2016-12-159). Informed consent was waived by the IRB because of the retrospective nature of the study and the analysis used anonymous clinical data.
All analyses were performed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). Continuous variables were analyzed using Student t-test or the Mann-Whitney U-test. Categorical variables were analyzed using Fisher exact test. Continuous variables including age and WBC count were categorized according to their mean values for inclusion in regression models. Propensity score statistical analysis was performed with IBM SPSS Statistics version 22.0 including R-Essentials for SPSS (IBM Co.) and Syntax version 4 software (EANCOM, United Nation's Directories for Electronic Data Interchange for Administration, Commerce and Transport). Patients were matched one-to-one by propensity score (random selection from severe near neighbour propensity score of which difference between the standard and the matching value less than 0.001, matching with logistic regression, caliper 0.2 without replacement) using the covariates of age, sex, initial CT finding, surgical approach (open, laparoscopy, and single-port laparoscopy), ASA physical status classification, body mass index, and WBC count. Categorical data were analyzed using χ2 and Mann-Whitney U-tests for comparison of peri- and postoperative outcomes between the pEIS group and the pES group. The likelihood ratio test was performed to determine trends in complications over time. Multivariable logistic regression analysis was performed to identify independent factors associated with postoperative complications and failure of EIS. P-values of 0.05 were considered statistically significant.
A total of 6,074 patients with acute appendicitis underwent appendectomy at Hallym University Dongtan Sacred Heart Hospital or Hallym University Kangnam Sacred Heart Hospital between January 2013 and June 2019. Of them, 1,627 patients underwent surgery for complicated appendicitis. A total of 360 patients were excluded for dysplasia or cancer (n = 8), age younger than 18 years (n = 332), or far delayed operation (>3 months) (n = 20). Two hundred patients had LS and 1,067 patients had ES (Fig. 1).
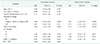
Characteristics of patients undergoing LS or ES for complicated appendicitis are summarized in Table 1. Patients with LS were significantly older than those with ES (mean: 48.1 years vs. 42.5 years, P < 0.001). Additionally, grades Ib and II on initial CT finding were significantly more prevalent in the LS group than those in the ES group (P < 0.001). The incidence of cecectomy and ileo-cecectomy or right hemicolectomy was more common than that of appendectomy in the LS group (77.5% vs. 85.2%, P < 0.001).
Postoperative complications occurred in a total of 124 patients (9.8%). The most common complication was wound infection (n = 77 [6.1%]), followed by postoperative ileus (n = 30 [2.4%]), intra-abdominal abscess (n = 14 [1.1%]), gastroenteritis (n = 2 [0.2%]), and port site herniation (n = 1 [0.1%]). Readmission was required in 50 patients (3.9%) and reoperation was needed in 1 patient (0.1%) (Table 2). According to Clavien-Dindo classification, grades I, II, and III were found to be in 86 (6.8%), 27 (2.1%), and 11 patients (0.9%), respectively.
Table 3 shows patient characteristics of the EIS group and the ES group before and after propensity score matching. These 2 groups were well matched especially for sex, initial CT finding, surgical approach, and WBC count. Surgical outcomes of the pEIS group and the pES group are shown in Table 4. Operation types were significantly different between the 2 groups. Ileo-cecectomy or right hemicolectomy was less prevalently performed in the pEIS group (P = 0.030). Open conversion rate was similar between the 2 groups (2.3% vs. 6.1%, P = 0.124). Among postoperative complications, wound infection rate was significantly lower in the EIS group (1.5% vs. 8.4%, P = 0.010) while intraabdominal abscess rate and ileus rate were similar between the 2 groups (P = 0.561 and P = 0.758, respectively). The pEIS group tended to have less prevalent grade I complication than the pES group (3.8% vs. 9.9%, P = 0.085), although total distribution of Clavien-Dindo classification was similar between the 2 groups. Postoperative hospital stay was significantly shorter in the pEIS group (3.7 vs. 5.8 days, P < 0. 0.001). Although the pEIS group had more cost for total treatment (P < 0. 0.001), its cost for surgical treatment only significantly less (P < 0. 0.001).
In univariate analysis, age (≥65 years), sex, ASA physical status classification, laboratory variables (WBC count), or body temperature did not increase the odds ratio of postoperative complications. Multivariate analysis showed that open conversion (odds ratio [OR], 4.94; P = 0.025) and delayed surgery for more than 48 hours or urgent surgery due to failure of EIS (OR, 2.55; P = 0.001) were independently associated with postoperative complications (Table 5).
Risk factor analysis was performed for failure of EIS. A total of 34 patients (18.2%) needed urgent operation before planned surgical date. In univariate analysis, high ASA physical status classification (III vs. I or II) (OR, 5.26; P = 0.007), and Grades Ib (OR, 4.65; P = 0.001) and II/III (OR, 6.0; P = 0.002) on CT finding were risk factors for failure of EIS. For CT findings, only 1.7% in grade Ia, 6.7% in grade Ib. and 10.0% in grade II/III resulted in failure of EIS. In multivariate analysis, OR for failure of EIS was 6.85 for ASA physical status classification of III, 4.60 for grade Ib, and 7.85 for grade II/III on initial CT finding (Table 6).
There were significant differences in sex, age, initial CT findings, surgical approach, and operation times between the LS group and the ES group. EIS was defined as patients who underwent LS on a planned date, excluding delayed surgery for more than 48 hours or urgent surgery due to failure of EIS. The EIS group was propensity score-matched with the ES group. They were redefined as the pEIS group and the pES group. Finally, surgical outcomes were compared between the pEIS group and the pES group.
The pEIS group in this study showed a lower rate of ileo-cecectomy or right hemicolectomy, a shorter hospital stay, and a lower rate of wound infection compared to the pES group. However, delayed surgery for more than 48 hours or urgent surgery due to failure of EIS significantly increased the risk of postoperative complications. Our subgroup analysis showed that high ASA physical status classification and initial CT findings of grades II/III were independently associated with failure of EIS.
Acute appendicitis was initially described in terms of its natural history and progression in 1886 by Reginald H. Fitz (quoted from [14]). Since then, it has become widely accepted that untreated appendicitis can progress to perforation which is associated with significant increases in morbidity, mortality, hospital stay, and resource usage [215]. Complicated appendicitis generally increases the risk of postoperative complications [16]. Thus, new strategies such as nonsurgical treatment and interval appendectomy after initial antibiotics treatment are discussed. Recent studies in pediatric patients suggest that hydration and administration of antibiotics can allow surgeons to delay surgery without detrimental effects on patient outcome [1718]. Furthermore, randomized controlled trials have suggested that antibiotic therapy without surgery is a safe treatment option for acute appendicitis [1920]. Some recent studies have reported that nonoperative management without interval appendectomy after treatment with antibiotics could be an alternative option for complicated appendicitis, and this is supported by evidence of relatively low rates (<10%) of recurrence of appendicitis or abscess after conservative management as well as reportedly high complication rates (as high as 12%–23%) in patients undergoing interval appendectomy [212223]. However, another study concluded that interval appendectomy should be strongly considered in those over the age of 40 because the rate of neoplasm in patients over 40 was 10 of 62 (16%) compared to 1 of 27 (4%) in those under age 40 [24]. In our study, 187 patients (14.8%) were planned to undergo EIS following initial antibiotics treatment. Of 187 patients, 34 (18.2%) were refractory to initial treatment. They underwent urgent surgery.
Several recent studies have also investigated the relationship between preoperative hospital delay (i.e., time from admission to surgery) and postoperative outcomes [252627]. Previous randomized controlled trials have reported that patients with suspected complicated appendicitis but no abscess have lower cost, shorter length of hospital stay, and lower complication rate when they are treated with early rather than late appendectomy [910]. A separate randomized trial has evaluated early versus delayed surgical management of appendiceal abscess and found that operating time and time to food intake in the early operation group are significantly longer [11]. Additionally, they did not find differences in recurrence of abscess or hospital charges [11]. Positive association between the increase of postoperative complications and delayed surgery for more than 48 hours or urgent surgery due to failure of EIS in this study might be due to delayed surgical management of appendiceal abscess or inflammation. However, the pEIS group showed significantly reduced wound infection rate and a tendency of decreased overall complications. Surgical complications that are known to be associated with acute inflammation might be decreased in the pEIS group because patients in the EIS group were treated with antibiotics for sufficient period and acute inflammation had fully subsided. In addition, we could avoid an unnecessary ileocecectomy or right-hemicolectomy likewise. Recent meta-analysis has shown that immediate surgical treatment of enclosed appendiceal inflammation is associated with a more than 3-fold increase in morbidity compared with conservative management and that it may result in an unnecessary ileocecal resection or right-sided hemicolectomy for technical reasons or suspicion of malignancy in about 3% of patients [26]. Our data showed a 4-fold increase of postoperative complication rate in the group having delayed surgery for more than 48 hours or urgent surgery due to failure of EIS. Similar increased postoperative complications were reported in delayed appendectomy for more than 48 hours [26] and 36 hours [5].
Postoperative hospital day was significantly reduced probably because of avoiding unnecessary ileo-cecectomy or right hemicolectomy in the pEIS group. The cost for surgical treatment was also significantly lower in the pEIS group in this study. However, total hospital stay was longer and total cost was higher in the pEIS group due to a total of 2 admissions.
Recent meta-analysis has shown that use of preoperative abdominal CT is associated with lower negative appendectomy rates [28]. In our study, all patients underwent preoperative CT scan for diagnosis of appendicitis and grading severity of inflammation. Our data showed that the grading system using CT scan was very important to select patients for EIS with complicated appendicitis. In univariate analysis, failure of EIS was associated with a 4.65-fold increase of initial CT finding for grade Ib and a 6-fold increase for grade II/III. It means that patients, who were initially planned to undergo EIS, experienced failure of EIS in only 1.7%, 6.7%, and 10.0% in grade Ia, Ib, and II/III, respectively. Hashizume et al. [29] have classified pathologic grades and CT grades into four grades and reported a close relationship between CT findings and pathologic findings. Kim et al. [30] have also investigated correlations of CT findings with WBC count and CRP levels and shown that WBC count might be useful for grade I appendicitis (normal) (P < 0.001) and CRP levels might be useful for grade IV appendicitis (perforated appendicitis) (P < 0. 0.001).
EIS is a good option for reducing surgeon's fatigue. A high overnight caseload might cause excessive fatigue and sleep deprivation among hospital and surgical staff. Several studies have reported negative effects of sleep deprivation on cognitive abilities [1011]. Accordingly, sleep deprivation could adversely affect surgical performance and patient safety. In addition, some surgical procedures such as appendectomy could be delayed in a semi-elective manner to reduce overnight caseload and avoid negative effects of sleep deprivation.
This study has several limitations. First, this study was performed retrospectively. Thus, there might be selection bias and recall bias. However, because the data collector retrieved these data from medical records without knowledge of the primary endpoint, results were less likely to be affected by data collection bias. Second, although the present study was conducted at 2 hospitals, the number of patients was not enough to reach a definitive conclusion.
In conclusion, the pEIS group showed a lower rate of ileo-cecectomy or right hemicolectomy, a tendency of lower rate of overall complication, a lower rate of wound infection, and a shorter postoperative hospital stay, although total hospital stay was longer and total cost was higher in the pEIS group. Failure of EIS increased the risk of postoperative complications. High ASA physical status classification (III) and CT finding of grades Ib and II/II were risk factors for failure of EIS. EIS can be a useful surgical option in adults with complicated appendicitis, especially for patients with low ASA physical status classification (I or II) and initial CT finding of grade Ia. We recommend that patients should be fully informed that EIS is beneficial in all CT grades, but the higher the grade, the greater the likelihood of failure of EIS.
Figures and Tables
Fig. 1
Flow chart showing the selection of patients. ES, early surgery within 2 days during index admission; LS, late surgery delayed more than 2 days; Urgent > 48 hours, late surgery delayed for more than 2 days during index admission; failure of EIS, surgery at urgent subsequent admission; pES, propensity score-matched early surgery; pEIS, propensity score-matched elective interval surgery on a planned date in 4–8 weeks.

Table 1
Characteristics of patients undergoing late surgery or early surgery for complicated appendicitis

Table 3
Subgroup analysis of patients of elective interval surgery versus early surgery for complicated appendicitis before and after propensity score matching

Table 4
Surgical outcomes between propensity score-matched elective interval surgery and early surgery for complicated appendicitis

ACKNOWLEDGEMENTS
The statistical analysis of this study was supported by the Division of Biostatistics, Hallym Institute for Clinical Medicine, Hallym University Medical Center. This research was supported by Hallym University Research Fund 2016 (HURF-2016-43).
References
1. Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat 13. 1998; (139):1–119.
2. Karp MP, Caldarola VA, Cooney DR, Allen JE, Jewett TC Jr. The avoidable excesses in the management of perforated appendicitis in children. J Pediatr Surg. 1986; 21:506–510.

3. Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007; 246:741–748.
4. Ingraham AM, Cohen ME, Bilimoria KY, Ko CY, Hall BL, Russell TR, et al. Effect of delay to operation on outcomes in adults with acute appendicitis. Arch Surg. 2010; 145:886–892.

5. Kim M, Kim SJ, Cho HJ. Effect of surgical timing and outcomes for appendicitis severity. Ann Surg Treat Res. 2016; 91:85–89.

6. Friedell ML, Perez-Izquierdo M. Is there a role for interval appendectomy in the management of acute appendicitis? Am Surg. 2000; 66:1158–1162.
7. Lai HW, Loong CC, Wu CW, Lui WY. Watchful waiting versus interval appendectomy for patients who recovered from acute appendicitis with tumor formation: a cost-effectiveness analysis. J Chin Med Assoc. 2005; 68:431–434.

8. Bufo AJ, Shah RS, Li MH, Cyr NA, Hollabaugh RS, Hixson SD, et al. Interval appendectomy for perforated appendicitis in children. J Laparoendosc Adv Surg Tech A. 1998; 8:209–214.

9. Blakely ML, Williams R, Dassinger MS, Eubanks JW 3rd, Fischer P, Huang EY, et al. Early vs interval appendectomy for children with perforated appendicitis. Arch Surg. 2011; 146:660–665.

10. Myers AL, Williams RF, Giles K, Waters TM, Eubanks JW 3rd, Hixson SD, et al. Hospital cost analysis of a prospective, randomized trial of early vs interval appendectomy for perforated appendicitis in children. J Am Coll Surg. 2012; 214:427–434.

11. St Peter SD, Aguayo P, Fraser JD, Keckler SJ, Sharp SW, Leys CM, et al. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg. 2010; 45:236–240.
12. Bates DB, Fernandez MB, Ponchiardi C, von Plato M, Teich JP, Narsule C, et al. Surgical management in acute diverticulitis and its association with multi-detector CT, modified Hinchey classification, and clinical parameters. Abdom Radiol (NY). 2018; 43:2060–2065.

13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.
14. Seal A. Appendicitis: a historical review. Can J Surg. 1981; 24:427–433.
15. Blomqvist PG, Andersson RE, Granath F, Lambe MP, Ekbom AR. Mortality after appendectomy in Sweden, 1987-1996. Ann Surg. 2001; 233:455–460.

16. Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg. 2010; 34:2026–2040.

17. Yardeni D, Hirschl RB, Drongowski RA, Teitelbaum DH, Geiger JD, Coran AG. Delayed versus immediate surgery in acute appendicitis: do we need to operate during the night? J Pediatr Surg. 2004; 39:464–469.

18. Surana R, Quinn F, Puri P. Is it necessary to perform appendicectomy in the middle of the night in children? BMJ. 1993; 306:1168.

19. Hansson J, Korner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009; 96:473–481.

20. Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006; 30:1033–1037.

21. Willemsen PJ, Hoorntje LE, Eddes EH, Ploeg RJ. The need for interval appendectomy after resolution of an appendiceal mass questioned. Dig Surg. 2002; 19:216–220.

22. Puapong D, Lee SL, Haigh PI, Kaminski A, Liu IL, Applebaum H. Routine interval appendectomy in children is not indicated. J Pediatr Surg. 2007; 42:1500–1503.

23. Quartey B. Interval appendectomy in adults: a necessary evil? J Emerg Trauma Shock. 2012; 5:213–216.

24. Wright GP, Mater ME, Carroll JT, Choy JS, Chung MH. Is there truly an oncologic indication for interval appendectomy? Am J Surg. 2015; 209:442–446.

25. Chen CC, Ting CT, Tsai MJ, Hsu WC, Chen PC, Lee MD, et al. Appendectomy timing: Will delayed surgery increase the complications? J Chin Med Assoc. 2015; 78:395–399.

26. United Kingdom National Surgical Research Collaborative. Bhangu A. Safety of short, in-hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta-analysis. Ann Surg. 2014; 259:894–903.
27. Saluja S, Sun T, Mao J, Steigman SA, Oh PS, Yeo HL, et al. Early versus late surgical management of complicated appendicitis in children: a statewide database analysis with one-year follow-up. J Pediatr Surg. 2018; 53:1339–1344.

28. Krajewski S, Brown J, Phang PT, Raval M, Brown CJ. Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg. 2011; 54:43–53.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download