Abstract
Purpose
This study was undertaken to compare fracture and flexural strength of provisional restorative resins fabricated by additive manufacturing, subtractive manufacturing, and conventional direct technique.
Materials and methods
Five types of provisional restorative resin made with different methods were investigated: Stereolithography apparatus (SLA) 3D printer (S3Z), two digital light processing (DLP) 3D printer (D3Z, D3P), milling method (MIL), conventional method (CON). For fracture strength test, premolar shaped specimens were prepared by each method and stored in distilled water at 37℃ for 24 hours. Compressive load was measured using a universal testing machine (UTM). For flexural strength test, rectangular bar specimens (25 × 2 × 2 mm) were prepared by each method according to ISO 10477 and flexural strength was measured by UTM.
Results
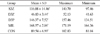
Fracture strengths of the S3Z, D3Z, and D3P groups fabricated by additive manufacturing were not significantly different from those of MIL and CON groups (P>.05/10=.005). On the other hand, the flexural strengths of S3Z, D3P, and MIL groups were significantly higher than that of CON group (P<.05), but the flexural strength of D3Z group was significantly lower than that of CON group (P<.05).
Figures and Tables
 | Fig. 1Specimens prepared by each method for fracture strength test. (A) S3Z, (B) D3Z, (C) D3P, (D) MIL, (E) CON. S3Z, Resin printed by ZENITH SLA 3D printer; D3Z, Resin printed by ZENITH DLP 3D printer; D3P, Resin printed by PROBO DLP 3D printer; MIL, milled resin; CON, conventionally self-cured resin. |
 | Fig. 3Specimens for flexural strength test. (A) S3Z, (B) D3Z, (C) D3P, (D) MIL, (E) CON. S3Z, Resin printed by ZENITH SLA 3D printer; D3Z, Resin printed by ZENITH DLP 3D printer; D3P, Resin printed by PROBO DLP 3D printer; MIL, milled resin; CON, conventionally self-cured resin. |
 | Fig. 5Fracture strength values of tested group (unit: N). Values followed by the same letter were significantly different (P < .05/10 = .005). |
 | Fig. 6Flexural strength values (mean ± SD) of tested group (unit: MPa). Values followed by the same letter were significantly different (P < .05). |
References
1. Park JS, Park MG. Effect of aging treatment on the flexural properties of polymer provisional restoration materials. Korean J Dent Mater. 2013; 40:215–221.
2. Shillingburg HT Jr, Hobo S, Whitsett LD. Fundamentals of fixed prosthodontics. 3rd ed. Chicago: Quintessence Publishing Co;1997. p. 225–227.
3. Song KY, Sorensen JA. Marginal adaptation of new provisional materials for fixed prosthodontics. J Dent Rehabil Appl Sci. 1997; 13:247–255.
4. Song ES, Kim BJ, Lim YJ, Lee JJ. Survey study on the preference of dental medical personnel for dental CAD/CAM milling machines. J Korean Acad Prosthodont. 2018; 56:188–198.

5. DeLong R, Heinzen M, Hodges JS, Ko CC, Douglas WH. Accuracy of a system for creating 3D computer models of dental arches. J Dent Res. 2003; 82:438–442.

6. Fuster-Torres MA, Albalat-Estela S, Alcañiz-Raya M, Peñarrocha-Diago M. CAD / CAM dental systems in implant dentistry: update. Med Oral Patol Oral Cir Bucal. 2009; 14:E141–E145.
7. Lee S. Prospect for 3D printing technology in medical, dental, and pediatric dental field. J Korean Acad Pediatr Dent. 2016; 43:93–108.

8. Hazeveld A, Huddleston Slater JJ, Ren Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am J Orthod Dentofacial Orthop. 2014; 145:108–115.

9. Karaokutan I, Sayin G, Kara O. In vitro study of fracture strength of provisional crown materials. J Adv Prosthodont. 2015; 7:27–31.

10. Alt V, Hannig M, Wöstmann B, Balkenhol M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent Mater. 2011; 27:339–347.

11. Nejatidanesh F, Momeni G, Savabi O. Flexural strength of interim resin materials for fixed prosthodontics. J Prosthodont. 2009; 18:507–511.

12. Mehrpour H, Farjood E, Giti R, Barfi Ghasrdashti A, Heidari H. Evaluation of the flexural strength of interim restorative materials in fixed prosthodontics. J Dent (Shiraz). 2016; 17:201–206.
13. Seo DG, Roh BD. The comparison of relative reliability on biaxial and three point flexural strength testing methods of light curing composite resin. J Korean Acad Conserv Dent. 2006; 31:58–65.

14. Mörmann WH, Brandestini M, Lutz F, Barbakow F. Chairside computer-aided direct ceramic inlays. Quintessence Int. 1989; 20:329–339.
15. Alharbi N, Osman R, Wismeijer D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J Prosthet Dent. 2016; 115:760–767.

16. Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, Ferracane JL, Bertassoni LE. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018; 34:192–200.

17. Matsumura H, Leinfelder KF. Three-body wear of four types of light-activated composite resin veneering materials. Quintessence Int. 1994; 25:425–430.
18. Peutzfeldt A. Resin composites in dentistry: the monomer systems. Eur J Oral Sci. 1997; 105:97–116.

19. Weaver RE, Goebel WM. Reactions to acrylic resin dental prostheses. J Prosthet Dent. 1980; 43:138–142.

20. Mair LH, Stolarski TA, Vowles RW, Lloyd CH. Wear: mechanisms, manifestations and measurement. Report of a workshop. J Dent. 1996; 24:141–148.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download