Abstract
A trichobezoar is a type of bezoar that is composed of hair. In most cases, it is confined to the stomach, but in rare cases, it may extend to the small intestine. This condition is referred to as Rapunzel syndrome. The therapeutic method for bezoar removal depends on its type, location, and size. Generally, the treatment for Rapunzel syndrome involves surgical laparotomy. Endoscopic removal has also been effective in some cases. On the other hand, complications, such as respiratory difficulty and esophageal impaction may be encountered during endoscopic removal. Until now, the successful endoscopic removal of trichobezoars has been limited to the stomach or duodenum. This paper reports the case of a 4-year-old female patient with Rapunzel syndrome whose trichobezoar reached the proximal jejunum. The trichobezoar was removed without complications using an electrosurgical knife and snare through a single-balloon enteroscopy. The trichobezoar can be removed successfully using enteroscopy under general anesthesia without abdominal laparotomy in young children. Therefore, this method of removal can be considered preferentially for children with Rapunzel syndrome.
Figures and Tables
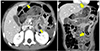 | Fig. 1Abdomen computed tomography scan pictures of (A) and (B) show that the bezoar-like materials are found in the stomach and jejunum (yellow arrows) with mucosal thickening. |
References
1. Kajal P, Bhutani N, Tyagi N, Arya P. Trichobezoar with and without Rapunzel syndrome in paediatric population: a case series from a tertiary care centre of Northern India. Int J Surg Case Rep. 2017; 40:23–26.

2. Finale E, Franceschini P, Danesino C, Barbaglia M, Guala A. Rapunzel syndrome: how to orient the diagnosis. Pediatr Rep. 2018; 10:7689.

3. Wang Z, Cao F, Liu D, Fang Y, Li F. The diagnosis and treatment of Rapunzel syndrome. Acta Radiol Open. 2016; 5:1–4.

4. Nettikadan A, Ravi MJ, Shivaprasad M. Recurrent Rapunzel syndrome - a rare tale of a hairy tail. Int J Surg Case Rep. 2018; 45:83–86.

5. Al-Osail EM, Zakary NY, Abdelhadi Y. Best management modality of trichobezoar: a case report. Int J Surg Case Rep. 2018; 53:458–460.

6. Hamid M, Chaoui Y, Mountasser M, et al. Giant gastric trichobezoar in a young female with Rapunzel syndrome: case report. Pan Afr Med J. 2017; 27:252.

7. Kim SC, Kim SH, Kim SJ. A case report: large trichobezoar causing Rapunzel syndrome. Medicine (Baltimore). 2016; 95:e3745.
8. Park SE, Ahn JY, Jung HY, et al. Clinical outcomes associated with treatment modalities for gastrointestinal bezoars. Gut Liver. 2014; 8:400–407.

9. Fallon SC, Slater BJ, Larimer EL, Brandt ML, Lopez ME. The surgical management of Rapunzel syndrome: a case series and literature review. J Pediatr Surg. 2013; 48:830–834.

10. Kao EY, Scalzitti NJ, Dion GR, Bowe SN. Trichobezoar causing air-way compromise during esophagogastroduodenoscopy. Case Rep Med. 2015; 2015:806857.

11. Park SH, Moon JS, Huh TG. Esophageal impaction of trichobezoar caused by endoscopic removal. Korean J Gastrointest Endosc. 2009; 39:222–225.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download