Abstract
Background
To evaluate the size of a postoperative lymphocele in the coronal and axial reconstruction planes using multidetector computed tomography (MDCT) in kidney transplantation recipients.
Methods
We evaluated 92 recipients who underwent MDCT of the abdominopelvis at 1 month after kidney transplantation. The axial short axis, axial surface area, coronal short axis, and coronal surface area of the lymphocele were measured using the reconstructed MDCT coronal and axial images. Depending on the clinical manifestations and radiologic findings of the recipients, all lymphoceles were classified into symptomatic and asymptomatic. We compared the suitability of the size measurement on coronal and axial planes of MDCT reconstruction for symptomatic lymphocele in kidney transplant recipients using Spearman's correlation analysis and comparisons of receiver operating characteristic (ROC) curves.
Results
Areas under the ROC curves were 0.957 and 0.928 for the axial short axis and axial surface area and 0.968 and 0.966 for the coronal short axis and coronal surface area, respectively. In pairwise comparison of the ROC curve of the parameters of the symptomatic lymphoceles, the coronal measurement was significant in contrast to the axial measurement (short axis, P=0.357; surface area, P=0.047).
Recently, the number of kidney transplantations, including transplantation for high-risk recipients, has increased and the long-term results of kidney transplantation are better than ever [1]. A lymphocele is a lymphatic fluid collection near the allograft after kidney transplantation. Because of obesity, new immunosuppressants, and high-risk transplantation, among other factors, postoperative lymphoceles are reported in 12%–40% in kidney recipients [2]. Lymphocele have typically been overlooked until symptoms such as graft dysfunction, ureteric obstruction, perigraft distension, leg swelling, and abdominal pain have developed [3]. For such reasons, detection and assessment of lymphocele are very important to prevent complications. However, most clinicians rely on the transverse size of the axial short axis and intuition regarding the shape of lymphocele.
From an anatomical point of view, lymphoceles commonly have a caudo-cranial orientation that follows patterns of lymphatic flow. Thus, habitual size measurements of lymphoceles on the axial plane may differ from those on the coronal plane. Using multidetector computed tomography (MDCT), obtained isotropic voxel data can allow axial and coronal reformatting of the entire abdomen and pelvis. To the best of our knowledge, the axial and coronal sizes of lymphocele as evaluated using MDCT have not been compared yet. Therefore, we aimed to compare between the axial and coronal sizes of lymphoceles using MDCT and evaluate the feasibility of size measurements of lymphoceles using MDCT in the prediction of symptomatic lymphoceles in patients who have undergone kidney transplantation.
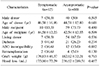
The present study is approved by the Investigation Review Committee of Korea University Hospital (No. ED15067). We evaluated 92 recipients who underwent MDCT of the abdominopelvis at 1 month after kidney transplantation from March 2012 to February 2015. In this center, the 1-month routine surveillance was performed, which included various laboratory tests, chest X-ray, and non-enhanced MDCT of the abdominopelvis, regardless of symptoms. Sixty-one patients received kidney transplantation from a living donor, with the transplanted kidney procured using the hand-assisted laparoscopic surgery technique. Thirty-one patients received the kidney from a deceased donor. The recorded baseline characteristics for symptomatic lymphoceles included sex, age of donor and recipient, donor type (living or deceased), diabetes, ABO incompatibility, retransplantation, graft weight, and blood loss. There were no statistical differences between the symptomatic and asymptomatic groups in terms of their baseline characteristics (Table 1).
Kidney transplantation was performed with a retroperitoneal approach; vein, artery, and ureter anastomoses were performed in a classical fashion. A double J catheter was placed from graft the hilum to the recipient's bladder. The recipients were usually discharged between postoperative day 10 and 14.
Symptomatic lymphoceles were defined as patient symptoms and anatomical distortion with suspicious fluid collection, suggestive of a lymphocele on MDCT of the abdominopelvis at 1 month after kidney transplantation. The symptoms included abdominal pain and swelling around the allograft, lower extremity swelling, and graft dysfunction. The anatomical distortion included bladder compression and kidney displacement on CT or ultrasound. After perigraft fluid analysis following aspiration, percutaneous drainage, fenestration, urinoma, abscess, and hematoma were excluded based on creatinine levels, fluid analysis, and culture. Asymptomatic lymphoceles included no suspicious fluid collections and small fluid collections without symptoms. Because there is a little fluid collection seen on most MDCT at 1 month, it is difficult to distinguish between an asymptomatic lymphocele and the absence of fluid collection.
The CT examinations of the abdomen without administration of a contrast agent were performed using a 128-slice MDCT scanner (Definition AS Plus, Siemens Healthcare, Forchheim, Germany). After scanning, an automatic raw data analysis tool (Syngo and Somaris/5; Siemens Medical Solutions, Erlangen, Germany) was used for the transverse CT data reconstruction. The transverse section CT data were automatically reformatted for (1) the axial plane with 5-mm sections at 5-mm intervals and (2) the coronal plane with 2-mm sections at 2-mm intervals. For interpretation, both the axial and coronal image sets were routinely transferred to a Picture Archiving and Communication System (PACS) (INFINITT Healthcare, Seoul, Korea). Analysis of the abdominal CT images for measuring the short axis and the surface area was assessed using commercial software (Terarecon iNtuition; TeraRecon, Foster City, CA, USA) by two reviewers (HJ, SHH). The short axis and surface area were measured on the plane considered to have the largest area in the axial and coronal image sets.
Continuous data are expressed as the mean±standard deviation. Depending on previously established criteria [4], all patients with a lymphocele were classified into two groups: symptomatic and asymptomatic. The difference in baseline characteristics between the two groups was evaluated using the chi-square test and t-test. The relationship between the axial and coronal sizes of lymphocele was evaluated using Pearson's correlation coefficient. The comparisons of mean sizes between symptomatic and asymptomatic lymphoceles were performed using the paired t-test. We then compared the feasibility of size measurements of lymphoceles between the coronal and axial planes of MDCT in the prediction of symptomatic lymphocele using receiver operating characteristic (ROC) curves. Additionally, the area under the curve (AUC) for each size measurement of the lymphocele was also obtained. The pairwise comparisons of ROC curves for symptomatic lymphoceles were performed to assess the suitability of each difference (axial short axis-coronal short axis, axial surface area-coronal surface area). The difference between areas (DBA) represents the difference between each AUC. All statistical analyses were performed using Medcalc 15.2 (Medcalc Software, Ostend, Belgium). A P-value of less than 0.05 was considered statistically significant.
Ninety-two kidney recipients were evaluated using MDCT and medical records in the study period. Clinical characteristics of all recipients are summarized in Table 1. The recipients with symptomatic lymphocele included 10 men (83.3%) and two women (16.4%). The recipients with asymptomatic lymphocele included 59 men (73.7%) and 21 women (26.3%). The mean ages of the recipients with symptomatic and asymptomatic lymphocele were 44.58±12.23 and 42.54±12.55 years, respectively. Regarding recipients who received a kidney from a living donor, seven (58.3%) had a symptomatic lymphocele and 54 (67.5%) had asymptomatic lymphocele. Symptoms from the symptomatic lymphocele included flank swelling and discomfort in four recipients, wound discharge with swelling in three, elevated creatinine with hilar lymphocele in two, hydroureter with inferior lymphocele in two, and leg swelling in one.
With regard to the relationship between the axial and coronal sizes of the lymphocele, the axial short axis and the axial surface area correlated well with the coronal measurements (R=0.925 and R=0.962, respectively) (Fig. 1). In the comparisons between the mean size parameters, including the mean axial short axis of symptomatic and asymptomatic lymphocele (66.00±34.39 mm, 14.73±15.16 mm), mean axial surface area (2,730.55±2,444.53 mm2, 383.29±518.05 mm2), mean coronal short axis (100.83±62.18 mm, 17.32±19.23 mm), and mean coronal surface area (6,508.65±7,319.63 mm2, 405.13±686.89 mm2), there were significant differences between symptomatic and asymptomatic lymphoceles.
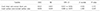
For the analysis of the performance of the test, the assessments of sensitivity, specificity, and cutoff value are very important. According to each parameter of the size measurements for symptomatic lymphocele, four ROC curves were plotted (Fig. 2). Areas under ROC curves were 0.957 and 0.928 for the axial short axis and axial surface areas and 0.968 and 0.966 for the coronal short axis and coronal surface areas, respectively. The AUC of the coronal measurement, including the coronal short axis and coronal surface area, was greater than that of the axial measurement. If the lymphocele is generally assumed to have an axial short axis of 40 mm [5], the cutoff values were axial surface area >1,241 mm2, coronal short axis >47.5 mm, and coronal surface area >1,580 mm2, based on the same specificity. In this situation, the sensitivity of the coronal measurements is greater than that of the axial measurement (coronal short axis, 91%; coronal surface area, 83%; axial short axis, 75%; axial surface area, 75%) (Table 2).
In the pairwise comparison of the ROC curve between the parameters for symptomatic lymphoceles, the difference in the AUC for the surface area between the coronal and axial measurements was statistically significant (P=0.047). Considering the AUC and DBA, there was a nonsignificant difference in the AUC of the short axis between the coronal and axial measurements (P=0.357), which means that the coronal measurement of the lymphocele is more significant and effective than the axial measurement in kidney recipients (Table 3).
Most lymphoceles after kidney transplantation originate from recipients' iliac lymphatic leakage during vessel dissection [3]. Lymphatic leakage occurs in the donor's graft, such as in the renal hilum and surface [6]. The risk factors for postoperative lymphocele have been reported in various fields, including obesity (i.e., BMI >30 kg/m2), use of sirolimus, multiple renal arteries of graft, renal graft procured from the right, history of rejection, and steroid pulse therapy, among other [78]. Moreover, Chedid et al. [8] reported that multiple renal arteries can be risk factors. Ulrich et al. [4] reported that diabetes is an independent risk factor for lymphocele development.
Most lymphoceles were asymptomatic and self-limiting. The presentations of symptomatic lymphoceles include obstructive graft dysfunction, ureteric obstruction, perigraft distension, cutaneous lymphatic fistula, abdominal pain, and edema of the external genitalia, among others [3]. Rarely, lymphoceles may cause postoperative sepsis and deep vein thrombosis [24]. Eventually, many symptoms can lead to graft dysfunction without proper management.
Many clinicians often have their own standards for measuring the size of lymphoceles and criteria for symptomatic lymphocele requiring intervention. It was reported that lymphoceles with a volume of less than 50 cm3 and a diameter of less than 3 cm were well-absorbed with conservative management based on postoperative ultrasound assessment [9]. Regarding the method of lymphocele size measurement, the transverse diameter of the axial plane was generally used in CT or ultrasound. In many cases, the kind of plane used for size measurement was not specified exactly and the maximum length was used, regardless of the plane. In a German group, if the diameter is between 3 cm and 5 cm, percutaneous drainage was selected and if more than 5 cm, laparoscopic unroofing was selected [8]. Adani et al. [9] had defined any diameter more than 2.5 cm for symptomatic lymphocele. Giuliani et al. [5] had defined any diameter more than 4 cm on ultrasound. Król et al. [10] had defined the volume as more than 140 cm3 on ultrasound. A Singaporean group has the strategy of open drainage in cases of any lymphocele with a diameter of more than 6 cm on postoperative ultrasound [11].
From a similar perspective, based on a transverse diameter of more than 4 cm in axial planes, the intervention in asymptomatic patients was routine 1-month surveillance with nonenhanced CT in this center. On the basis of an axial short axis of 4 cm, the cutoff values of axial surface area, coronal short axis, and coronal surface area were analyzed with the same specificity in this study. In particular, a coronal short axis of more than 47.5 mm has a sensitivity of 91% and specificity of 95% for symptomatic lymphocele. This is a good cutoff value and can be helpful in planning for lymphoceles.
Often, clinicians refer to use planimeter because it is possible to measure without difficult reconstruction. Especially if the planimetry is not significantly different from the volumetry, the planimetry is readily available and can be greatly helpful in the clinic. Planimetry has been utilized in various fields, such as cerebral hematoma, cardiac chamber, cardiac valve, prostate volume, and acoustic neuroma [1213]. Dowlatshahi et al. [14] insisted that computer-assisted planimetry provides reliable measurement of intraventricular hematoma volume. Guinet et al. [15] reported that coronal measurements gives higher sensitivity than axial measurements in the assessment of mediastinal nodes of lung cancer. Selection of the proper planes with a more representative view of the anatomical features of the structure is crucial for clinicians in assessing the patients with a cross-section plane on CT.
This study has several limitations. In fact, the definition of lymphocele is often unclear in various reports. Large lymphoceles causing symptoms can be analyzed using aspiration, and hematoma and urinoma can be excluded. However, fluid analysis of small lymphoceles is not easy, and small lymphoceles are not clinically defined. In the coronal and axial planes, the lymphocele has the shape of an incomplete circle. The short axis measured in this study was identified according to what the measurer regarded as the short axis of the circle. In this study, it was difficult to clarify the temporal relationship between symptom onset and MDCT. Therefore, the predictive value of this study is limited as a diagnostic tool that can help diagnosis in advance.
For the prediction of symptomatic lymphocele using MDCT, the coronal measurement of postoperative lymphoceles can provide a significant improvement in diagnostic performance over axial measurements in kidney transplant recipients.
Figures and Tables
 | Fig. 1Linear regression analysis of lymphocele parameters between the axial and coronal planes. (A) The correlation between the axial and coronal short axes had a Pearson's coefficient of 0.925. (B) The correlation between the axial and coronal surface areas had a Pearson's coefficient of 0.962. |
 | Fig. 2Receiver operating characteristic curve and cutoff value for a symptomatic lymphocele that requires radiologic or surgical intervention. |
References
1. Hariharan S, Johnson CP, Bresnahan BA, Taranto SE, McIntosh MJ, Stablein D. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med. 2000; 342:605–612.

2. Zietek Z, Sulikowski T, Tejchman K, Sieńko J, Janeczek M, Iwan-Zietek I, et al. Lymphocele after kidney transplantation. Transplant Proc. 2007; 39:2744–2747.

3. Ebadzadeh MR, Tavakkoli M. Lymphocele after kidney transplantation: where are we standing now? Urol J. 2008; 5:144–148.
4. Ulrich F, Niedzwiecki S, Fikatas P, Nebrig M, Schmidt SC, Kohler S, et al. Symptomatic lymphoceles after kidney transplantation: multivariate analysis of risk factors and outcome after laparoscopic fenestration. Clin Transplant. 2010; 24:273–280.

5. Giuliani S, Gamba P, Kiblawi R, Midrio P, Ghirardo G, Zanon GF. Lymphocele after pediatric kidney transplantation: incidence and risk factors. Pediatr Transplant. 2014; 18:720–725.

6. Gomes AS, Scholl D, Feinberg S, Simmons RL, Amplatz K. Lymphangiography and ultrasound in management of lymphoceles. Urology. 1979; 13:104–108.

7. Goel M, Flechner SM, Zhou L, Mastroianni B, Savas K, Derweesh I, et al. The influence of various maintenance immunosuppressive drugs on lymphocele formation and treatment after kidney transplantation. J Urol. 2004; 171:1788–1792.

8. Chedid MF, Muthu C, Nyberg SL, Lesnick TG, Kremers WK, Prieto M, et al. Living donor kidney transplantation using laparoscopically procured multiple renal artery kidneys and right kidneys. J Am Coll Surg. 2013; 217:144–152.

9. Adani GL, Baccarani U, Bresadola V, Lorenzin D, Montanaro D, Risaliti A, et al. Graft loss due to percutaneous sclerotherapy of a lymphocele using acetic acid after renal transplantation. Cardiovasc Intervent Radiol. 2005; 28:836–838.

10. Król R, Kolonko A, Chudek J, Ziaja J, Pawlicki J, Mały A, et al. Did volume of lymphocele after kidney transplantation determine the choice of treatment modality? Transplant Proc. 2007; 39:2740–2743.

11. Sim A, Ng LG, Cheng C. Occurrence of a lymphocele following renal transplantation. Singapore Med J. 2013; 54:259–262.

12. Yu YL, Lee MS, Juan CJ, Hueng DY. Calculating the tumor volume of acoustic neuromas: comparison of ABC/2 formula with planimetry method. Clin Neurol Neurosurg. 2013; 115:1371–1374.

13. Saura D, de la Morena G, Flores-Blanco PJ, Oliva MJ, Caballero L, González-Carrillo J, et al. Aortic valve stenosis planimetry by means of three-dimensional transesophageal echocardiography in the real clinical setting: feasibility, reliability and systematic deviations. Echocardiography. 2015; 32:508–515.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download