Abstract
Purpose
Materials and Methods
Results
Conclusion
Notes
AUTHOR CONTRIBUTIONS:
Conceptualization: Seong Min Kim.
Data curation: Eun Jung Cho and Seong Min Kim.
Formal analysis: Seong Min Kim.
Investigation: Seong Min Kim.
Methodology: Seong Min Kim.
Project administration: Seong Min Kim.
Resources: Eun Jung Cho and Seong Min Kim.
Software: Eun Jung Cho.
Supervision: Seong Min Kim.
Validation: Seong Min Kim.
Visualization: Eun Jung Cho.
Writing—original draft: Eun Jung Cho.
Writing—review & editing: Seong Min Kim.
References
Fig. 1
Flow chart showing the management of adjustable gastric band (AGB) patients (n=267). The patients in the grey rectangle indicate those who are involved in this study. SL, slippage group; BE, band erosion group; IT, intolerance group; LSG, laparoscopic sleeve gastrectomy; SLi, isolated AGB explantation due to slippage; BEi, isolated AGB explantation due to band erosion; ITi, isolated AGB explantation due to intolerance.
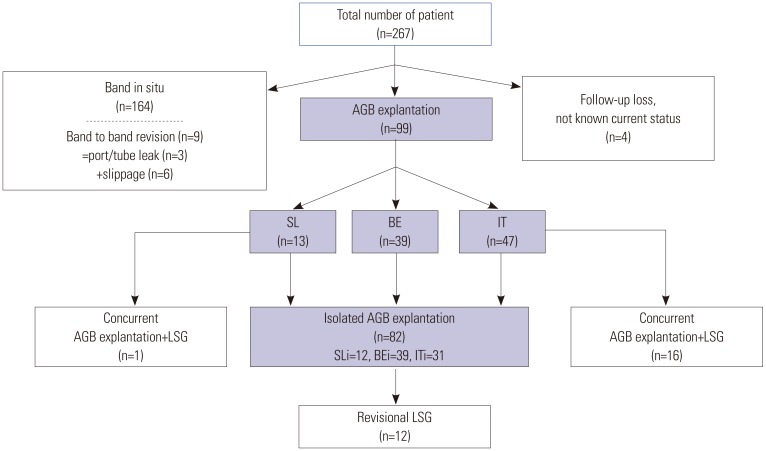
Fig. 2
Annual incidences and trends of adjustable gastric band (AGB) implantation/explantations over the study period.
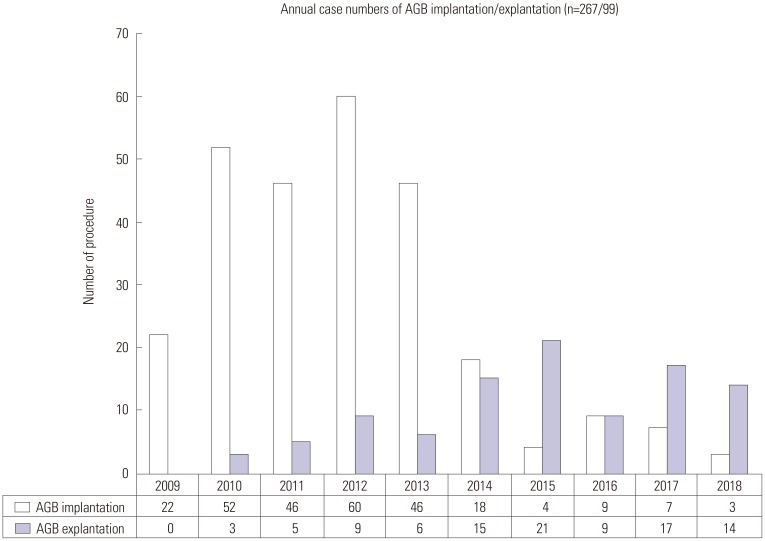
Fig. 3
Annual case numbers of adjustable gastric band (AGB) explantation according to etiology (n=99). SL, slippage group; BE, band erosion group; IT, intolerance group.
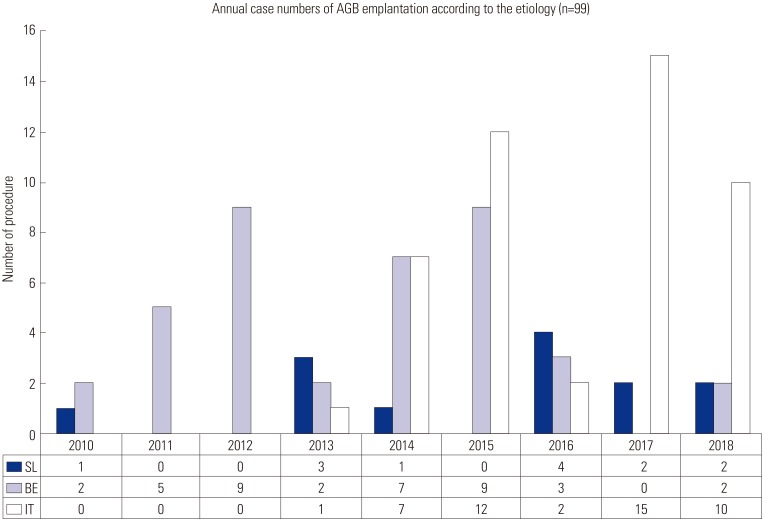
Table 1
Demographic and Anthropometric Data of the Patients at Time of Band Explantation (n=99)
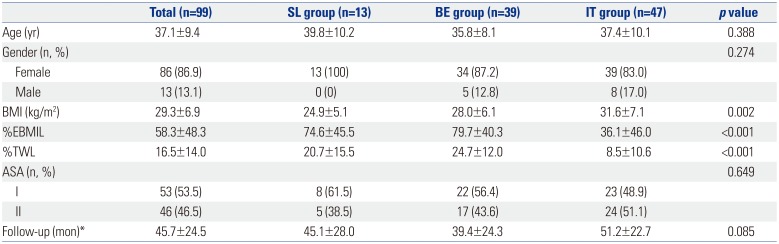
SL, slippage; BE, band erosion; IT, intolerance; BMI, body mass index; ASA, the American Society of Anesthesiologists physical status classification system.
Continuous variables are expressed as mean±standard deviation or n (%) unless otherwise indicated. ‘%EBMIL’ means ‘% excess BMI loss=[(BMI at band implantation−BMI at band explantation)/(BMI at band implantation−23)]×100’. ‘%TWL’ means ‘%Total weight loss=% of weight loss at band explantation compared with weight at band implantation’. ‘I’ means ‘normal healthy patient’. ‘II’ means ‘mild systemic disease [e.g., current smoker, social alcohol drinker, pregnancy, obesity (30<BMI<40), well-controlled diabetes mellitus/hypertension, mild lung disease].
*Time from band implantation to explantation.
Table 2
Perioperative Data of Patients that Underwent Isolated AGB Explantation (n=82)
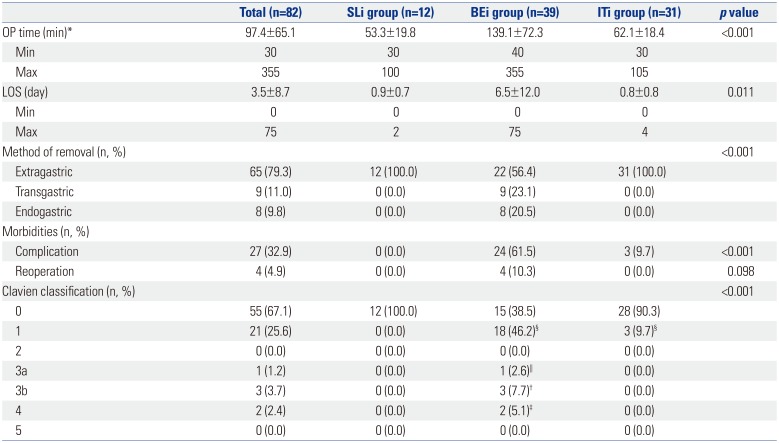
SLi, isolated adjustable gastric band (AGB) explantation due to slippage; BEi, isolated AGB explantation due to band erosion; ITi, Isolated AGB explantation due to intolerance; OP, operation time; LOS, postoperative length of hospital stay; Extragastric, laparoscopic extragastric removal; Transgastric, laparoscopic transgastric removal; Endogastric, endoscopic removal.
Values are presented as mean±standard deviation or n (%) unless otherwise indicated.
*Operation time required for band explantation; †Intra-abdominal abscess, re-laparoscopy (n=2), laparotomy (n=1); ‡Septic shock (n=1), hemorrhagic shock (n=1): both required intensive care unit admission; §Antipyretics used for recurrent spiking fever (>38.0℃). ∥Intra-abdominal abscess, percutaneous drainage insertion (n=1).
Table 3
Perioperative Complications (Clavien-Dindo) Encountered after Isolated AGB Explantation in Band Erosion Group (BEi) according to Surgical Approaches (n=39) (p=0.019)
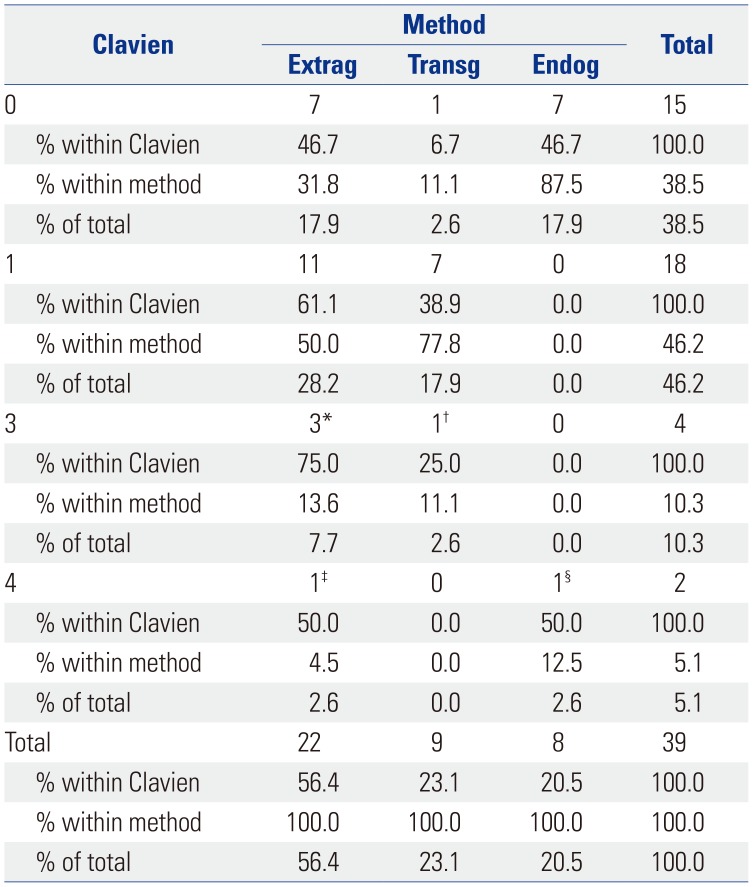
AGB, adjustable gastric band; Extrag, extragastric approach; Transg, transgastric approach; Endog, endogastric approach.
*Intra-abdominal abscess: Clavien 3a [n=1, percutaneous drainage (PCD)]+Clavien 3b (n=2, re-laparoscopy); †Intra-abdominal abscess: Clavien 3b (n=1, laparotomy); ‡Intra-abdominal abscess: Clavien 4 [n=1, PCD, intensive care unit (ICU) admission]; §Hemorrhagic shock after endoscopic removal: Clavien 4 (n=1, laparotomy, ICU admission).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download