Abstract
Objective
Methods
Results
Figures and Tables
Figure 1
Region of interest (ROI) in quantification of bone microstructure (A) and new bone (NB) and old bone (OB) formation (B1 and B2). A, The furcation enclosed by the buccal and lingual roots of premolars was defined as the ROI (arrow) for measurements of bone microstructure. B, Magnification at hematoxylin and eosin (H&E) stain (×200) showing NB and OB. NB is defined as the amorphous eosinophilic material with porous bone and pale cement lines (black arrow). OB is the bone with a compact feature and prominent cement lines (white arrow) (B1); the total tissue area (outlined by the blue line) at H&E stain (×20) (B2).

Figure 2
Relative values of bone volume fraction (BV/TV) at the premolar regions compared to the control values in groups 1 (corticotomy + rapid maxillary expansion [RME]) and 2 (conventional RME) after 4 and 12 weeks of retention.

Figure 3
A, Relative values of bone volume fraction (BV/TV) values compared to the control values for the banded teeth (the first and third premolars) in groups 1 (corticotomy + rapid maxillary expansion [RME]) and 2 (conventional RME) after 4 and 12 weeks of retention. B, Alveolar trabecular bone microstructural images of group 1 after 4 (B1) and 12 weeks of retention (B3) and of group 2 after 4 (B2) and 12 weeks of retention (B4). C, Histological images at H&E stain (×100) showed that the bone volume in group 1 after 4 and 12 weeks of retention (C1 and C3) were higher than those in group 2 after 4 and 12 weeks of retention (C2 and C4) (H&E stain, ×100).

Table 1
Definition of parameters used in the quantification of bone microstructure and new bone formation in the region of interest (ROI)

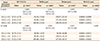
Table 2
Bony microstructural changes in groups 1–3 after the 4- and 12-week retention periods

Values are presented as mean ± standard deviation.
G, Group; G1, corticotomy + rapid maxillary expansion (RME); G2, conventional RME; G3, control; P1, first premolar; P2, second premolar; P3, third premolar.
*Two-way analysis of variance with Bonferroni post-hoc assessment for comparisons among groups.
See Table 1 for the definitions of each measurement.
Table 3
Differences in bony microstructural changes of pool banded teeth (P1 + P3) in groups 1–3 after the 4- and 12-week retention periods
Values are presented as mean ± standard deviation.
G, Group; G1, corticotomy + rapid maxillary expansion (RME); G2, conventional RME; G3, control.
*One-way analysis of variance with Bonferroni post-hoc assessment for comparison among groups.
See Table 1 for the definitions of each measurement.
Table 4
New and old bone components in supporting tissue in groups 1–3 after 4 and 12 weeks of retention

Values are presented as mean ± standard deviation.
G, Group; G1, corticotomy + rapid maxillary expansion (RME); G2, conventional RME; G3, control; P2, second premolar; P3, third premolar.
*Two-way analysis of variance with Bonferroni post-hoc assessment for comparison among groups.
See Table 1 for the definitions of each measurement.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download