Abstract
Purpose
This study investigated the optimal strategy to minimize budgetary constraints on National Health Insurance (NHI) services, while maximizing the number of diabetic macular edema (DME) patients who receive anti-vascular endothelial growth factor (anti-VEGF) therapy.
Methods
We estimated the potential budget impact of anti-VEGF treatments in DME patients based on perceived upcoming changes in reimbursement fees over the next 5 years (2018–2022). Four scenarios were evaluated: (1) current anti-VEGF treatment patterns, (2) the hypothetical reimbursement fee, (3) the introduction of a new molecule similar to current anti-VEGF treatments, and (4) the prescription of an off-label drug, bevacizumab. The number of patients, anti-VEGF treatments, and medical costs for each scenario were calculated using claims data from the Korean NHI system and anti-VEGF prescription data from a single hospital.
Results
The potential budget impact of anti-VEGF injections in patients with DME over the next 5 years was estimated to be about 97.7 billion and 106.2 billion KRW for scenarios 1 and 2, respectively. In scenario 3, in which a biosimilar product to anti- VEGF is used, the estimated budget of the NHI system would be approximately 98.4 billion KRW. If an off-label drug is reimbursed, roughly 79.5 billion KRW will be required for the NHI system's budget.
Conclusions
If the revised fee structure for AMD patients is similarly applied to anti-VEGF injections for DME patients, the NHI fiscal requirements will increase disproportionately over the next 5 years compared to current reimbursement conditions. Given the growth of DME patients in toda's patient population, the use of a biosimilar or off-label drug is a financially viable alternative to reduce the overall burden on the NHI system.
Figures and Tables
Table 4
Expectation of new patients of diabetic macular edema in the future (2018–2022) by scenario 1

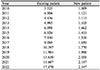
Table 5
Expectation of new patients of diabetic macular edema in the future (2018–2022) by scenario 2–4

Notes
References
1. Lu L, Jiang Y, Jaganathan R, Hao Y. Current advances in pharmacotherapy and technology for diabetic retinopathy: a systematic review. J Ophthalmol. 2018; 2018:1694187.

2. Dow C, Mancini F, Rajaobelina K, et al. Diet and risk of diabetic retinopathy: a systematic review. Eur J Epidemiol. 2018; 33:141–156.

3. Shi GJ, Shi GR, Zhou JY, et al. Involvement of growth factors in diabetes mellitus and its complications: a general review. Biomed Pharmacother. 2018; 101:510–527.

4. Rubsam A, Parikh S, Fort PE. Role of inflammation in diabetic retinopathy. Int J Mol Sci. 2018; 19.
5. Sivaprasad S, Gupta B, Crosby-Nwaobi R, Evans J. Prevalence of diabetic retinopathy in various ethnic groups: a worldwide perspective. Surv Ophthalmol. 2012; 57:347–370.

6. Kreft D, McGuinness MB, Doblhammer G, Finger RP. Diabetic retinopathy screening in incident diabetes mellitus type 2 in Germany between 2004 and 2013 - a prospective cohort study based on health claims data. PLoS One. 2018; 13:e0195426.

7. de Melo LGN, Morales PH, Drummond KRG, et al. Prevalence and risk factors for referable diabetic retinopathy in patients with type 1 diabetes: a nationwide study in Brazil. Acta Ophthalmol. 2018.

8. Acan D, Calan M, Er D, et al. The prevalence and systemic risk factors of diabetic macular edema: a cross-sectional study from Turkey. BMC Ophthalmol. 2018; 18:91.

9. Makwana T, Takkar B, Venkatesh P, et al. Prevalence, progression, and outcomes of diabetic retinopathy during pregnancy in Indian scenario. Indian J Ophthalmol. 2018; 66:541–546.

10. Jee D, Lee WK, Kang S. Prevalence and risk factors for diabetic retinopathy: the Korea National Health and Nutrition Examination Survey 2008-2011. Invest Ophthalmol Vis Sci. 2013; 54:6827–6833.

11. Lee BY, Jee D. Association between grapes intake and diabetic retinopathy: inhibitory effect of resveratol on diabetic retinopathy. J Korean Ophthalmol Soc. 2016; 57:276–282.

12. Jee D, Han K, Kim EC. Inverse association between high blood 25-hydroxyvitamin D levels and diabetic retinopathy in a representative Korean population. PLoS One. 2014; 9:e115199.

13. Jee D, Keum N, Kang S, Arroyo JG. Sleep and diabetic retinopathy. Acta Ophthalmol. 2016; 95:41–47.

14. Daruich A, Matet A, Moulin A, et al. Mechanisms of macular edema: Beyond the surface. Prog Retin Eye Res. 2018; 63:20–68.

15. Parodi Battaglia M, Iacono P, Cascavilla M, et al. A pathogenetic classification of diabetic macular edema. Ophthalmic Res. 2018; 60:23–28.

16. Liu E, Craig JE, Burdon K. Diabetic macular oedema: clinical risk factors and emerging genetic influences. Clin Exp Optom. 2017; 100:569–576.

17. Cai S, Bressler NM. Aflibercept, bevacizumab or ranibizumab for diabetic macular oedema: recent clinically relevant findings from DRCR.net Protocol T. Curr Opin Ophthalmol. 2017; 28:636–643.
18. Bahrami B, Hong T, Gilles MC, Chang A. Anti-VEGF therapy for diabetic eye diseases. Asia Pac J Ophthalmol (Phila). 2017; 6:535–545.

19. Fogli S, Del Re M, Rofi E, et al. Clinical pharmacology of intravitreal anti-VEGF drugs. Eye (Lond). 2018; 32:1010–1020.

20. Miller K, Fortun JA. Diabetic macular edema: current understanding, pharmacologic treatment options, and developing therapies. Asia Pac J Ophthalmol (Phila). 2018; 7:28–35.
21. Terasaki H, Ogura Y, Kitano S, et al. Management of diabetic macular edema in Japan: a review and expert opinion. Jpn J Ophthalmol. 2018; 62:1–23.

22. Lorence DP, Spink A. Regional variation in medical systems data: influences on upcoding. J Med Syst. 2002; 26:369–381.
23. Ziemssen F, Grisanti S, Bartz-Schmidt KU, Spitzer MS. Off-label use of bevacizumab for the treatment of age-related macular degeneration: what is the evidence? Drugs Aging. 2009; 26:295–320.




 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download