Abstract
Purpose
To investigate the efficacy and factors affecting the success rates of nasolacrimal probing and silicone intubation (SI) in patients with congenital nasolacrimal duct obstruction (CNLDO).
Methods
We retrospectively reviewed the medical records of patients including 69 eyes of 59 patients who received probing and 61 eyes of 49 patients who received SI. In patients with probing, the age, sex, and history of conservative treatment were analyzed in the success and failure groups, and a success rate comparison was conducted by dividing these values into postnatal group 1 (< 6 months), group 2 (6–12 months), and group 3 (≥ 12 months) following their age. In patients with SI, the age, sex, retention period of the tube, and history of probing and conservative treatment were analyzed in the success and failure groups.
Results
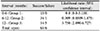
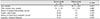
In the failure group involving probing, the average age was significantly higher compared with the success group (p = 0.005), and the success rate of group 3 was significantly lower compared with group 2 (p = 0.005). In the failure group involving SI, the age was significantly higher (p = 0.015); however, the retention period was shorter (p = 0.006), and the history of probing also showed a statistically significant difference between the two groups (p = 0.009). Logistic regression analysis showed that the age and history of probing had an effect on the success rate (p = 0.049 and p = 0.047, respectively); however, the retention period was not statistically significant (p = 0.411).
Figures and Tables
Table 2
The interval likelihood ratios and confidence intervals for success of nasolacrimal probing based on different age groups
References
1. Lee SY, Chung HS, Kim HB, et al. The incidence of congenital nasolacrimal duct obstruction in Korean neonates. J Korean Ophthalmol Soc. 1989; 30:5–8.
2. Oh HS, Ahn Y. The incidence and medical treatment of congenital nasolacrimal duct obstruction in Korean infants. J Korean Ophthalmol Soc. 1995; 36:1007–1013.
3. Paul TO. Medical management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 1985; 22:68–70.

4. Petersen RA, Robb RM. The natural course of congenital obstruction of the nasolacrimal duct. J Pediatr Ophthalmol Strabismus. 1978; 15:246–250.

5. el-Mansoury J, Calhoun JH, Nelson LB, Harley RD. Results of late probing for congenital nasolacrimal duct obstruction. Ophthalmology. 1986; 93:1052–1054.

6. Moon JS, Choi WC. Office probing of congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 1999; 40:2357–2361.
7. Katowitz JA, Welsh MG. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology. 1987; 94:698–705.

8. Cho SJ, Byon DS, Moon YS. The clinical outcome of probing and silicone tube intubation for congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2001; 42:1661–1665.
9. Sturrock SM, MacEwen CJ, Young JD. Long-term results after probing for congenital nasolacrimal duct obstruction. Br J Ophthalmol. 1994; 78:892–894.

10. Shin SG, Eum YH, Chung EH. Usefulness of early probing in congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 1994; 35:972–976.
11. Mannor GE, Rose GE, Frimpong-Ansah K, Ezra E. Factors affecting the success of nasolacrimal duct probing for congenital nasolacrimal duct obstruction. Am J Ophthalmol. 1999; 127:616–617.

12. Havins WE, Wilkins RB. A useful alternative to silicone intubation in congenital nasolacrimal duct obstructions. Ophthalmic Surg. 1983; 14:666–670.

13. Ahn DH, Lew H, Kim HY, Lee SY. The effect of probing for congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 1998; 39:836–840.
14. Paul TO, Shepherd R. Congenital nasolacrimal duct obstruction: natural history and the timing of optimal intervention. J Pediatr Ophthalmol Strabismus. 1994; 31:362–367.

15. Young JD, MacEwen CJ. Managing congenital lacrimal obstruction in general practice. BMJ. 1997; 315:293–296.
16. Welsh MG, Katowitz JA. Timing of silastic tubing removal after intubation for congenital nasolacrimal duct obstruction. Ophthalmic Plast Reconstr Surg. 1989; 5:43–48.

17. Migliori ME, Putterman AM. Silicone intubation for the treatment of congenital lacrimal duct obstruction: successful result removing the tubes after six weeks. Ophthalmology. 1988; 95:792–795.
18. Kraft ST, Crawford JS. Silicone tube intubation in disorders of the lacrimal system in children. Am J Ophthalmol. 1982; 94:290–299.

19. Lee JJ, Ahn JH, Kim JL, Yang JW. The clinical outcome of endoscopic silicone tube intubation for congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2012; 53:929–933.

20. Park J, Lee YJ, Kim SJ, Jang JW. Factors affecting the outcome of silicone intubation for congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2011; 52:266–271.

21. Engel JM, Hichie-Schmidt C, Khammar A, et al. Monocanalicular silastic intubation for the initial correction of congenital nasolacrimal duct obstruction. J AAPOS. 2007; 11:183–186.

22. Ghuman T, Gonzales C, Mazow ML. Treatment of congenital nasolacrimal duct obstruction. Am Orthopt J. 1999; 49:163–168.

23. Lim CS, Martin F, Beckenham T, Cumming RG. Nasolacrimal duct obstruction in children: outcome of intubation. J AAPOS. 2004; 8:466–472.

24. Yoon TJ, Na KS, Yoon WJ. The effect of silicone tube intubation in pediatric nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2002; 43:155–159.
25. Pediatric Eye Disease Investigator Group. Repka MX, Melia BM, et al. Primary treatment of nasolacrimal duct obstruction with nasolacrimal duct intubation in children younger than 4 years of age. J AAPOS. 2008; 12:445–450.
26. Peterson NJ, Weaver RG, Yeatts RP. Effect of short-duration silicone intubation in congenital nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 2008; 24:167–171.

27. Sener EC, Onerci M. Reappraisal of probing of the congenital obstruction of the nasolacrimal system: is nasal endoscopy essential? Int J Pediatr Otorhinolaryngol. 2001; 58:65–68.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download