INTRODUCTION
MATERIALS AND METHODS
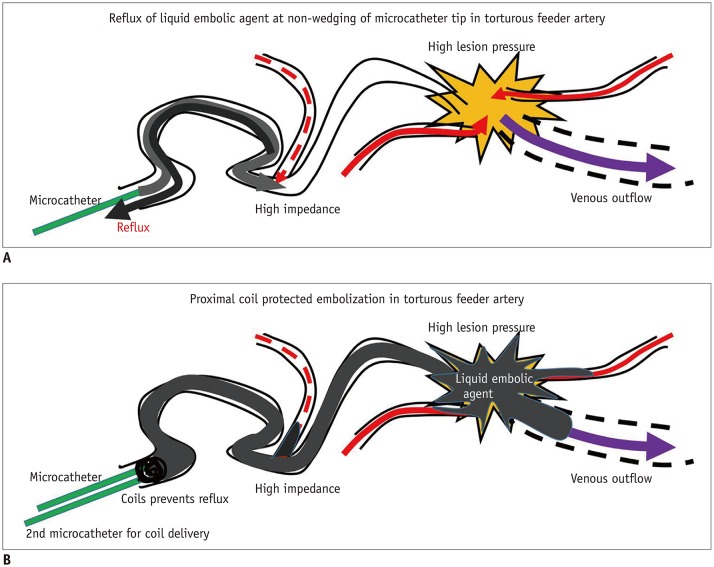 | Fig. 1Illustration of coil-protected technique.
A. During liquid embolization with non-wedging microcatheter tip due to arterial tortuosity, penetration of liquid embolic agent is impossible and early reflux occurs. B. Coil-protected technique makes it possible to deliver liquid embolic agent to target shunt without reflux proximal to coil mass.
|
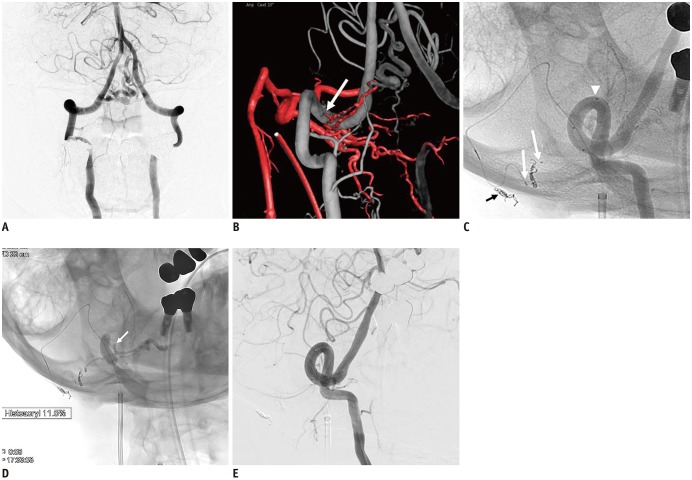 | Fig. 2Findings for 69-year-old man presenting with nausea and vomiting that had aggravated over 3 months.
A. Right vertebral angiogram shows dural arteriovenous fistula with engorged perimedullary draining vein at craniocervical junction. B. Fusion image obtained with dual 3-dimensional volume reconstruction shows relationship of two feeders, one from right vertebral artery (white color) and other from occipital artery (red color). Note that two feeders are connected near right vertebral artery (arrow). C. Non-subtracted angiogram obtained just before embolization. Arrows indicate tips of two microcatheters in feeding branch of right occipital artery, proximal microcatheter for coiling and distal microcatheter for injection of NBCA. Note coils placed between two catheter tips. Arrowhead indicates proximal marker of balloon catheter for protection of NBCA reflux into right vertebral artery during embolization. Short arrow indicates coil mass occluding another branch of right occipital artery, which is occluded to facilitate navigation of microcatheter into target feeding artery. D. Spot image obtained after injection of 11.5% NBCA. Arrow indicates reflux of NBCA into feeder arising from right vertebral artery, which is protected by inflated balloon. Use of inflated balloon during injection of NBCA prevents NBCA from refluxing into vertebral artery through its feeder, which joins with feeder of right occipital artery. E. Right vertebral angiogram shows complete occlusion of fistula. NBCA = N-butyl cyanoacrylate
|
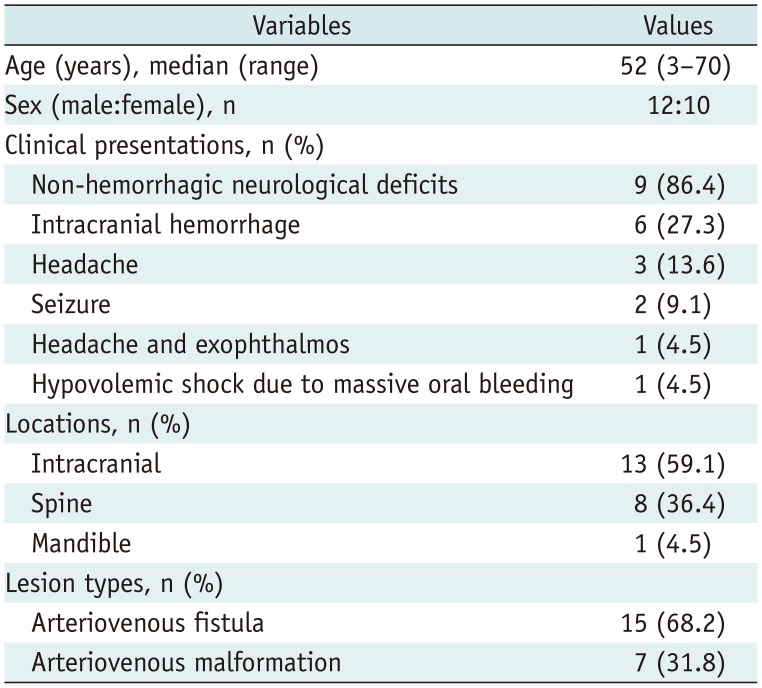
Table 1
Baseline Clinical and Angiographic Characteristics
Endovascular Procedure
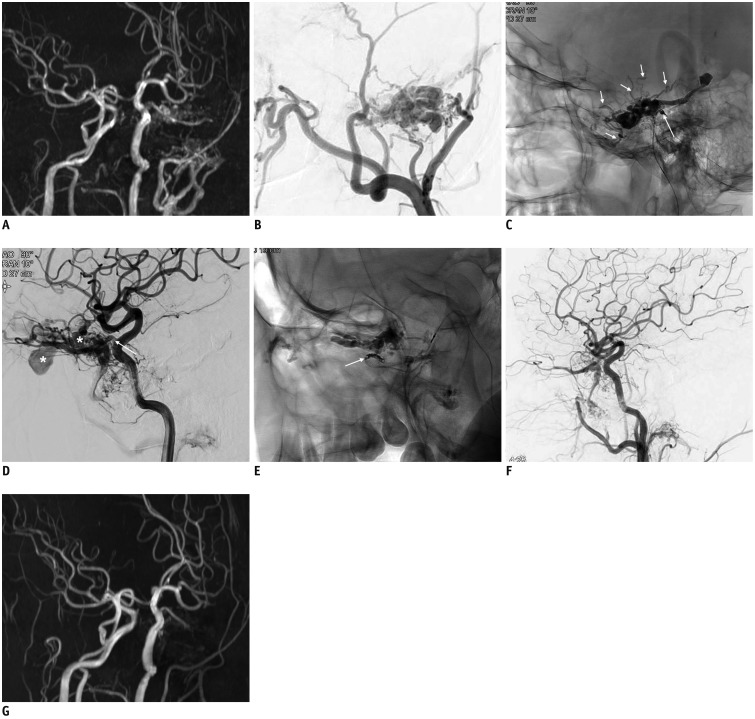 | Fig. 3Findings for 30-year-old man presenting with exophthalmos and tinnitus.
A. MR angiogram shows multiple fistulas in left orbital and left temporal regions. B. Left external angiogram in working projection shows intraosseous fistula fed by multiple feeders in left temporal bone. C. Non-subtracted spot image obtained just after injection of 12% NBCA by proximal coil-protected technique. Note refluxes to other feeders (short arrows) from fistula, which mimics phenomenon during Onyx (Medtronic) embolization. Long arrow indicates coil mass and final coil is not detached. D. Left internal carotid angiogram in working projection. Enlarged left ophthalmic artery is main feeding artery into shunt, which forms multiple venous pouches (asterisks) and then drains through superior ophthalmic vein and pterygoid plexus. E. Spot image obtained just after proximal coil-protected NBCA embolization. Coil delivery catheter is located at lacrimal branch of left ophthalmic artery (arrow). Final coil is not yet detached. F. Left common carotid angiogram shows complete occlusion of left temporal bone fistula and near-complete occlusion of left orbit fistula. G. 12-month follow-up MR angiogram shows no recurrence of fistulas in left orbit and left temporal bone. MR = magnetic resonance
|
 | Fig. 4Findings for 8-year-old boy presenting with intracerebral hemorrhage from de novo arteriovenous malformation.
A. Frontal angiogram shows arteriovenous malformation with intranidal aneurysm (arrow), which is rupture point. B. Non-subtracted image of angiogram obtained just after embolization. Note segment of feeding artery where coil mass is placed (arrowheads). Straight and curved arrows indicate microcatheter for coiling and microcatheter for Onyx injection, respectively. C. 26-month follow-up delayed arterial phase angiogram shows complete occlusion of arteriovenous malformation.
|
Statistical Analysis
RESULTS
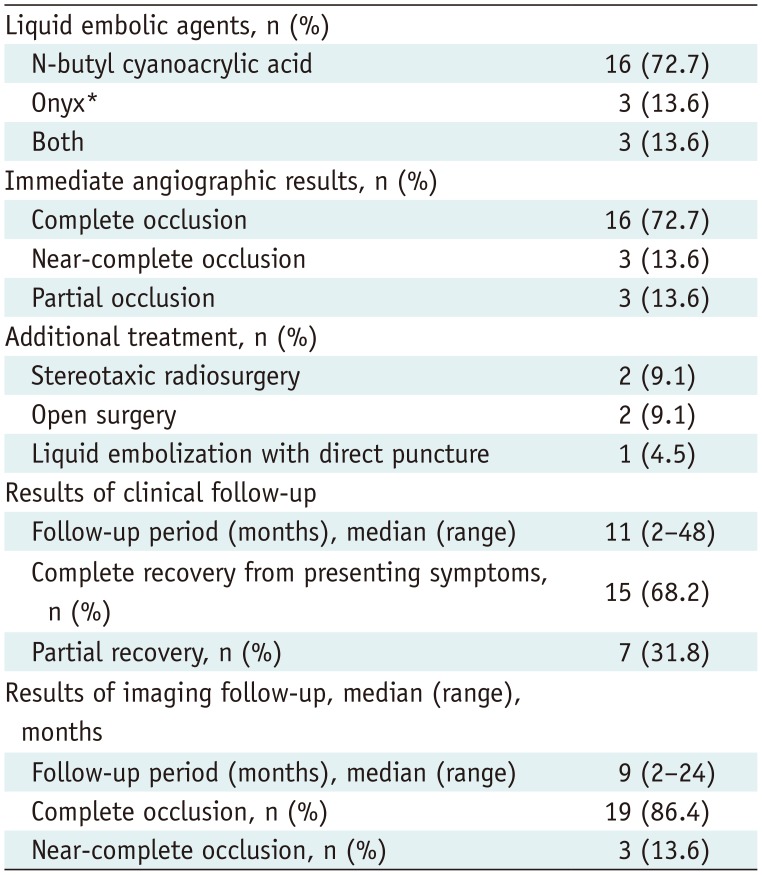
Table 2
Liquid Embolic Agents and Immediate and Follow-Up Outcomes




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download