1. Kuivaniemi H, Elmore JR. Opportunities in abdominal aortic aneurysm research: epidemiology, genetics, and pathophysiology. Ann Vasc Surg. 2012; 26:862–870. PMID:
22794334.

2. Wang LJ, Prabhakar AM, Kwolek CJ. Current status of the treatment of infrarenal abdominal aortic aneurysms. Cardiovasc Diagn Ther. 2018; 8(Suppl 1):S191–S199. PMID:
29850431.

3. Lederle FA, Johnson GR, Wilson SE, Ballard DJ, Jordan WD Jr, Blebea J, et al. Veterans Affairs Cooperative Study #417 Investigators. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA. 2002; 287:2968–2972. PMID:
12052126.

4. Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg. 1991; 5:491–499. PMID:
1837729.

5. Schermerhorn ML, Bensley RP, Giles KA, Hurks R, O'malley AJ, Cotterill P, et al. Changes in abdominal aortic aneurysm rupture and short-term mortality, 1995-2008: a retrospective observational study. Ann Surg. 2012; 256:651–658. PMID:
22964737.
6. Kent KC, Zwolak RM, Egorova NN, Riles TS, Manganaro A, Moskowitz AJ, et al. Analysis of risk factors for abdominal aortic aneurysm in a cohort of more than 3 million individuals. J Vasc Surg. 2010; 52:539–548. PMID:
20630687.

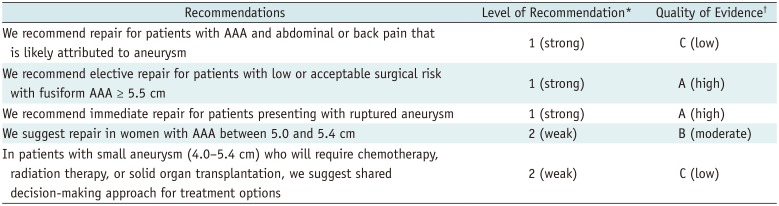
7. Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018; 67:2–77.e2. PMID:
29268916.

8. Sidloff D, Stather P, Dattani N, Bown M, Thompson J, Sayers R, et al. Aneurysm global epidemiology study: public health measures can further reduce abdominal aortic aneurysm mortality. Circulation. 2014; 129:747–753. PMID:
24249717.

9. Isselbacher EM. Thoracic and abdominal aortic aneurysms. Circulation. 2005; 111:816–828. PMID:
15710776.

10. Carino D, Sarac TP, Ziganshin BA, Elefteriades JA. Abdominal aortic aneurysm: evolving controversies and uncertainties. Int J Angiol. 2018; 27:58–80. PMID:
29896039.

11. Kuivaniemi H, Ryer EJ, Elmore JR, Tromp G. Understanding the pathogenesis of abdominal aortic aneurysms. Expert Rev Cardiovasc Ther. 2015; 13:975–987. PMID:
26308600.

12. Kuivaniemi H, Platsoucas CD, Tilson MD 3rd. Aortic aneurysms: an immune disease with a strong genetic component. Circulation. 2008; 117:242–252. PMID:
18195185.
13. Ailawadi G, Eliason JL, Upchurch GR Jr. Current concepts in the pathogenesis of abdominal aortic aneurysm. J Vasc Surg. 2003; 38:584–588. PMID:
12947280.

14. Heistad DD, Marcus ML. Role of vasa vasorum in nourishment of the aorta. Blood Vessels. 1979; 16:225–238. PMID:
41607.

15. Tsamis A, Krawiec JT, Vorp DA. Elastin and collagen fibre microstructure of the human aorta in ageing and disease: a review. J R Soc Interface. 2013; 10:20121004. PMID:
23536538.

16. Wolinsky H, Glagov S. Comparison of abdominal and thoracic aortic medial structure in mammals. Deviation of man from the usual pattern. Circ Res. 1969; 25:677–686. PMID:
5364644.
17. Lederle FA, Wilson SE, Johnson GR, Reinke DB, Littooy FN, Acher CW, et al. Aneurysm Detection and Management Veterans Affairs Cooperative Study Group. Immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med. 2002; 346:1437–1444. PMID:
12000813.

18. Cao P, De Rango P, Verzini F, Parlani G, Romano L, Cieri E. CAESAR Trial Group. Comparison of surveillance versus aortic endografting for small aneurysm repair (CAESAR): results from a randomised trial. Eur J Vasc Endovasc Surg. 2011; 41:13–25. PMID:
20869890.

19. Filardo G, Powell JT, Martinez MA, Ballard DJ. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst Rev. 2015; (2):CD001835. PMID:
25927098.

20. Ouriel K, Clair DG, Kent KC, Zarins CK. Positive Impact of Endovascular Options for treating Aneurysms Early (PIVOTAL) Investigators. Endovascular repair compared with surveillance for patients with small abdominal aortic aneurysms. J Vasc Surg. 2010; 51:1081–1087. PMID:
20304589.

21. United Kingdom Small Aneurysm Trial Participants. Powell JT, Brady AR, Brown LC, Fowkes FG, Greenhalgh RM, Ruckley CV, et al. Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med. 2002; 346:1445–1452. PMID:
12000814.

22. Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. The UK Small Aneurysm Trial Participants. Lancet. 1998; 352:1649–1655. PMID:
9853436.
23. Powell JT, Brown LC, Forbes JF, Fowkes FG, Greenhalgh RM, Ruckley CV, et al. Final 12-year follow-up of surgery versus surveillance in the UK Small Aneurysm Trial. Br J Surg. 2007; 94:702–708. PMID:
17514693.
24. Bryce Y, Rogoff P, Romanelli D, Reichle R. Endovascular repair of abdominal aortic aneurysms: vascular anatomy, device selection, procedure, and procedure-specific complications. Radiographics. 2015; 35:593–615. PMID:
25763741.

25. Aburahma AF, Campbell JE, Mousa AY, Hass SM, Stone PA, Jain A, et al. Clinical outcomes for hostile versus favorable aortic neck anatomy in endovascular aortic aneurysm repair using modular devices. J Vasc Surg. 2011; 54:13–21. PMID:
21324631.

26. AbuRahma AF, Yacoub M, Mousa AY, Abu-Halimah S, Hass SM, Kazil J, et al. Aortic neck anatomic features and predictors of outcomes in endovascular repair of abdominal aortic aneurysms following vs not following instructions for use. J Am Coll Surg. 2016; 222:579–589. PMID:
26905372.
27. Giménez-Gaibar A, González-Cañas E, Solanich-Valldaura T, Herranz-Pinilla C, Rioja-Artal S, Ferraz-Huguet E. Could preoperative neck anatomy influence follow-up of EVAR? Ann Vasc Surg. 2017; 43:127–133. PMID:
28390913.

28. Brunner-Ziegler S, Hammer A, Seidinger D, Willfort-Ehringer A, Koppensteiner R, Steiner S. The role of intraluminal thrombus formation for expansion of abdominal aortic aneurysms. Wien Klin Wochenschr. 2015; 127:549–554. PMID:
25994875.

29. Parr A, McCann M, Bradshaw B, Shahzad A, Buttner P, Golledge J. Thrombus volume is associated with cardiovascular events and aneurysm growth in patients who have abdominal aortic aneurysms. J Vasc Surg. 2011; 53:28–35. PMID:
20934838.

30. Arko FR, Rubin GD, Johnson BL, Hill BB, Fogarty TJ, Zarins CK. Type-II endoleaks following endovascular AAA repair: preoperative predictors and long-term effects. J Endovasc Ther. 2001; 8:503–510. PMID:
11718410.

31. Güntner O, Zeman F, Wohlgemuth WA, Heiss P, Jung EM, Wiggermann P, et al. Inferior mesenteric arterial type II endoleaks after endovascular repair of abdominal aortic aneurysm: are they predictable? Radiology. 2014; 270:910–919. PMID:
24475813.

32. Kuziez MS, Sanchez LA, Zayed MA. Abdominal aortic aneurysm type II endoleaks. J Cardiovasc Dis Diagn. 2016; 4:pii: 255.

33. Moll FL, Powell JT, Fraedrich G, Verzini F, Haulon S, Waltham M, et al. Management of abdominal aortic aneurysms clinical practice guidelines of the European Society for Vascular Surgery. Eur J Vasc Endovasc Surg. 2011; 41(Suppl 1):S1–S58. PMID:
21215940.

34. Briggs C, Babrowski T, Skelly C, Milner R. Anatomic and clinical characterization of the narrow distal aorta and implications after endovascular aneurysm repair. J Vasc Surg. 2018; 68:1030–1038.e1. PMID:
29802041.

35. Coulston J, Baigent A, Selvachandran H, Jones S, Torella F, Fisher R. The impact of endovascular aneurysm repair on aortoiliac tortuosity and its use as a predictor of iliac limb complications. J Vasc Surg. 2014; 60:585–589. PMID:
24797548.

36. Taudorf M, Jensen LP, Vogt KC, Grønvall J, Schroeder TV, Lönn L. Endograft limb occlusion in EVAR: iliac tortuosity quantified by three different indices on the basis of preoperative CTA. Eur J Vasc Endovasc Surg. 2014; 48:527–533. PMID:
24878235.

37. Oshin OA, Fisher RK, Williams LA, Brennan JA, Gilling-Smith GL, Vallabhaneni SR, et al. Adjunctive iliac stents reduce the risk of stent-graft limb occlusion following endovascular aneurysm repair with the Zenith stent-graft. J Endovasc Ther. 2010; 17:108–114. PMID:
20199276.

38. Jean-Baptiste E, Batt M, Azzaoui R, Koussa M, Hassen-Khodja R, Haulon S. A comparison of the mid-term results following the use of bifurcated and aorto-uni-iliac devices in the treatment of abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2009; 38:298–304. PMID:
19608439.

39. Choke E, Munneke G, Morgan R, Belli AM, Dawson J, Loftus IM, et al. Visceral and renal artery complications of suprarenal fixation during endovascular aneurysm repair. Cardiovasc Intervent Radiol. 2007; 30:619–627. PMID:
17401761.

40. Miller LE, Razavi MK, Lal BK. Suprarenal versus infrarenal stent graft fixation on renal complications after endovascular aneurysm repair. J Vasc Surg. 2015; 61:1340–1349.e1. PMID:
25736780.

41. O'Donnell ME, Sun Z, Winder RJ, Ellis PK, Lau LL, Blair PH. Suprarenal fixation of endovascular aortic stent grafts: assessment of medium-term to long-term renal function by analysis of juxtarenal stent morphology. J Vasc Surg. 2007; 45:694–700. PMID:
17398377.
42. Guo X, Lu X, Yang J, Kassab GS. Increased aortic stiffness elevates pulse and mean pressure and compromises endothelial function in Wistar rats. Am J Physiol Heart Circ Physiol. 2014; 307:H880–H887. PMID:
25038146.

43. Hori D, Akiyoshi K, Yuri K, Nishi S, Nonaka T, Yamamoto T, et al. Effect of endoskeleton stent graft design on pulse wave velocity in patients undergoing endovascular repair of the aortic arch. Gen Thorac Cardiovasc Surg. 2017; 65:506–511. PMID:
28597335.

44. Mohan IV, Laheij RJ, Harris PL;. Risk factors for endoleak and the evidence for stent-graft oversizing in patients undergoing endovascular aneurysm repair. Eur J Vasc Endovasc Surg. 2001; 21:344–349. PMID:
11359336.

45. Sternbergh WC 3rd, Money SR, Greenberg RK, Chuter TA. Zenith Investigators. Influence of endograft oversizing on device migration, endoleak, aneurysm shrinkage, and aortic neck dilation: results from the Zenith Multicenter Trial. J Vasc Surg. 2004; 39:20–26. PMID:
14718806.

46. Dietrich CF, Horn R, Morf S, Chiorean L, Dong Y, Cui XW, et al. US-guided peripheral vascular interventions, comments on the EFSUMB guidelines. Med Ultrason. 2016; 18:231–239. PMID:
27239660.

47. Nelson PR, Kracjer Z, Kansal N, Rao V, Bianchi C, Hashemi H, et al. A multicenter, randomized, controlled trial of totally percutaneous access versus open femoral exposure for endovascular aortic aneurysm repair (the PEVAR trial). J Vasc Surg. 2014; 59:1181–1193. PMID:
24440678.

48. Buck DB, Karthaus EG, Soden PA, Ultee KH, van Herwaarden JA, Moll FL, et al. Percutaneous versus femoral cutdown access for endovascular aneurysm repair. J Vasc Surg. 2015; 62:16–21. PMID:
25827969.

49. Uhlmann ME, Walter C, Taher F, Plimon M, Falkensammer J, Assadian A. Successful percutaneous access for endovascular aneurysm repair is significantly cheaper than femoral cutdown in a prospective randomized trial. J Vasc Surg. 2018; 68:384–391. PMID:
29526378.

50. Huff CM, Silver MJ, Ansel GM. Percutaneous endovascular aortic aneurysm repair for abdominal aortic aneurysm. Curr Cardiol Rep. 2018; 20:79. PMID:
30046990.

51. Biancari F, Mäkelä J, Juvonen T, Venermo M. Is inferior mesenteric artery embolization indicated prior to endovascular repair of abdominal aortic aneurysm? Eur J Vasc Endovasc Surg. 2015; 50:671–674. PMID:
26319477.

52. Samura M, Morikage N, Mizoguchi T, Takeuchi Y, Ueda K, Harada T, et al. Identification of anatomical risk factors for type II endoleak to guide selective inferior mesenteric artery embolization. Ann Vasc Surg. 2018; 48:166–173. PMID:
29275128.

53. Kouvelos GN, Katsargyris A, Antoniou GA, Oikonomou K, Verhoeven EL. Outcome after interruption or preservation of internal iliac artery flow during endovascular repair of abdominal aorto-iliac aneurysms. Eur J Vasc Endovasc Surg. 2016; 52:621–634. PMID:
27600731.

54. Pua U, Tan K. Radiology of advanced EVAR techniques in complex abdominal aortic aneurysms. Eur Radiol. 2012; 22:387–397. PMID:
21927792.

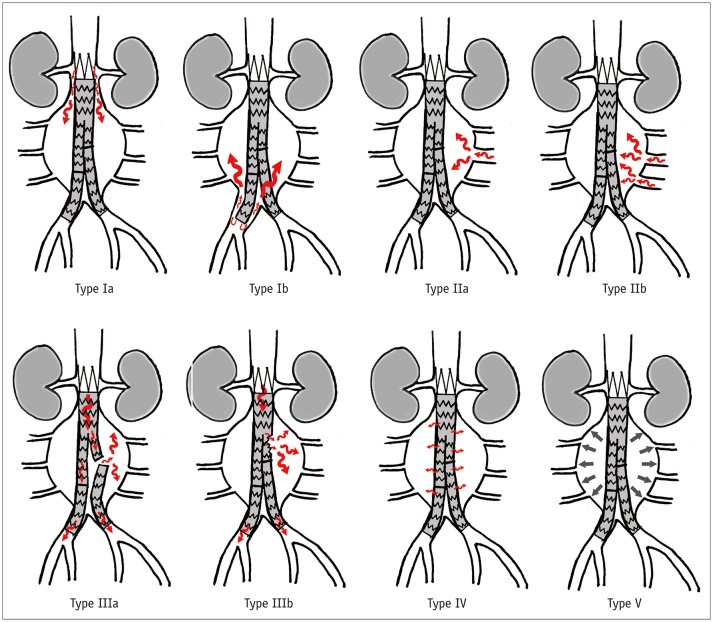
55. Amin S, Schnabel J, Eldergash O, Chavan A. [Endovascular aneurysm repair (EVAR): complication management]. Radiologe. 2018; 58:841–849. PMID:
30083939.
56. Fernandez JD, Craig JM, Garrett HE Jr, Burgar SR, Bush AJ. Endovascular management of iliac rupture during endovascular aneurysm repair. J Vasc Surg. 2009; 50:1293–1299. discussion 1299–1300. PMID:
19703755.

57. Arnaoutoglou E, Kouvelos G, Koutsoumpelis A, Patelis N, Lazaris A, Matsagkas M. An update on the inflammatory response after endovascular repair for abdominal aortic aneurysm. Mediators Inflamm. 2015; 2015:945035. PMID:
26166953.

58. Daye D, Walker TG. Complications of endovascular aneurysm repair of the thoracic and abdominal aorta: evaluation and management. Cardiovasc Diagn Ther. 2018; 8(Suppl 1):S138–S156. PMID:
29850426.

59. Arnaoutoglou E, Kouvelos G, Papa N, Kallinteri A, Milionis H, Koulouras V, et al. Prospective evaluation of post-implantation inflammatory response after EVAR for AAA: influence on patients' 30 day outcome. Eur J Vasc Endovasc Surg. 2015; 49:175–183. PMID:
25579873.

60. Kakisis JD, Moulakakis KG, Antonopoulos CN, Mylonas SN, Giannakopoulos TG, Sfyroeras GS, et al. Volume of newonset thrombus is associated with the development of postimplantation syndrome after endovascular aneurysm repair. J Vasc Surg. 2014; 60:1140–1145. PMID:
24953900.

61. Spanos K, Karathanos C, Saleptsis V, Giannoukas AD. Systematic review and meta-analysis of migration after endovascular abdominal aortic aneurysm repair. Vascular. 2016; 24:323–336. PMID:
26056151.

62. de la Motte L, Falkenberg M, Koelemay MJ, Lönn L. Is EVAR a durable solution? Indications for reinterventions. J Cardiovasc Surg (Torino). 2018; 59:201–221.

63. Tadros RO, Faries PL, Ellozy SH, Lookstein RA, Vouyouka AG, Schrier R, et al. The impact of stent graft evolution on the results of endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2014; 59:1518–1527. PMID:
24589162.
64. Maleux G, Poorteman L, Laenen A, Saint-Lèbes B, Houthoofd S, Fourneau I, et al. Incidence, etiology, and management of type III endoleak after endovascular aortic repair. J Vasc Surg. 2017; 66:1056–1064. PMID:
28434700.

65. Fransen GA, Desgranges P, Laheij RJ, Harris PL, Becquemin JP. EUROSTAR Collaborators. Frequency, predictive factors, and consequences of stent-graft kink following endovascular AAA repair. J Endovasc Ther. 2003; 10:913–918. PMID:
14656182.

66. van Zeggeren L, Bastos Gonçalves F, van Herwaarden JA, Zandvoort HJ, Werson DA, Vos JA, et al. Incidence and treatment results of Endurant endograft occlusion. J Vasc Surg. 2013; 57:1246–1254. discussion 1254. PMID:
23395203.

67. Cochennec F, Becquemin JP, Desgranges P, Allaire E, Kobeiter H, Roudot-Thoraval F. Limb graft occlusion following EVAR: clinical pattern, outcomes and predictive factors of occurrence. Eur J Vasc Endovasc Surg. 2007; 34:59–65. PMID:
17400004.

68. Laohapensang K, Arworn S, Orrapin S, Reanpang T, Orrapin S. Management of the infected aortic endograft. Semin Vasc Surg. 2017; 30:91–94. PMID:
29248126.

69. O'Connor S, Andrew P, Batt M, Becquemin JP. A systematic review and meta-analysis of treatments for aortic graft infection. J Vasc Surg. 2006; 44:38–45. PMID:
16828424.
70. Murphy EH, Szeto WY, Herdrich BJ, Jackson BM, Wang GJ, Bavaria JE, et al. The management of endograft infections following endovascular thoracic and abdominal aneurysm repair. J Vasc Surg. 2013; 58:1179–1185. PMID:
23830947.

71. Miyahara T, Hoshina K, Ozaki M, Ogiwara M. Efficacy of Preoperative Antibiotic Therapy for the Treatment of Vascular Graft Infection. Ann Vasc Dis. 2018; 11:191–195. PMID:
30116410.

72. Zaiem F, Almasri J, Tello M, Prokop LJ, Chaikof EL, Murad MH. A systematic review of surveillance after endovascular aortic repair. J Vasc Surg. 2018; 67:320–331.e37. PMID:
28662928.

73. Tacher V, Lin M, Desgranges P, Deux JF, Grünhagen T, Becquemin JP, et al. Image guidance for endovascular repair of complex aortic aneurysms: comparison of two-dimensional and three-dimensional angiography and image fusion. J Vasc Interv Radiol. 2013; 24:1698–1706. PMID:
24035418.

74. Jones DW, Stangenberg L, Swerdlow NJ, Alef M, Lo R, Shuja F, et al. Image fusion and 3-dimensional roadmapping in endovascular surgery. Ann Vasc Surg. 2018; 52:302–311. PMID:
29793018.

75. Cantisani V, Grazhdani H, Clevert DA, Iezzi R, Aiani L, Martegani A, et al. EVAR: benefits of CEUS for monitoring stent-graft status. Eur J Radiol. 2015; 84:1658–1665. PMID:
26198116.

76. Chisci E, Harris L, Guidotti A, Pecchioli A, Pigozzi C, Barbanti E, et al. Endovascular aortic repair follow up protocol based on contrast enhanced ultrasound is safe and effective. Eur J Vasc Endovasc Surg. 2018; 56:40–47. PMID:
29673811.

77. Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, et al. The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012; 33:33–59. PMID:
21874631.

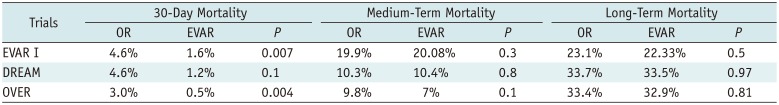
78. Lederle FA, Freischlag JA, Kyriakides TC, Padberg FT Jr, Matsumura JS, Kohler TR, et al. Open Versus Endovascular Repair (OVER) Veterans Affairs Cooperative Study Group. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009; 302:1535–1542. PMID:
19826022.
79. Patel R, Sweeting MJ, Powell JT, Greenhalgh RM. EVAR trial investigators. Endovascular versus open repair of abdominal aortic aneurysm in 15-years' follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial. Lancet. 2016; 388:2366–2374. PMID:
27743617.

80. Prinssen M, Verhoeven EL, Buth J, Cuypers PW, van Sambeek MR, Balm R, et al. Dutch Randomized Endovascular Aneurysm Management (DREAM) Trial Group. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004; 351:1607–1618. PMID:
15483279.












 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download