Abstract
Legionella species are abundant in the built environment and are increasingly recognized as a cause of Legionnaires' disease (LD). As the number of cases of Legionnaires' disease acquired by local communities in the Seoul metropolitan area in Korea has been increased, there was concern that changes in environmental factors could affect disease outbreaks. We described the association between climatic variables and occurrence of legionellosis in Korea and Legionella detection rate in Seoul area. A total of 418 cases of legionellosis were reported between 2014 and 2017. There was a seasonal peak in summer. LD continuously occurred from early spring to winter every year and rapidly increased in summer. In the regression analysis, the primary variables of interest- PM2.5 (µg/m3), NO2 (ppb), and a number of the date of issue O3 warning were not significant except for average temperature (R2=0.8075). The Legionella detection rate in Seoul, Korea showed a trend similar to precipitation (P=0.708, ANOVA). A relatively high proportion of Legionella detection rate was shown, especially cooling tower (17.7%) and public bath (19.3%). This finding is in line with current understanding of the ecological profile of this pathogen and supports the assertion that legionellosis occurs through contamination of water sources.
Legionella is a genus of pathogenic Gram-negative bacteria responsible for a serious disease known as legionellosis, which is transmitted via inhalation of this pathogen in aerosol form. There are two forms of Legionnaires' disease (LD), a potentially fatal pneumonia and Pontiac fever, a milder self-limiting flu-like illness (12).
Legionella, highly diverse (3) and pleomorphic (4) bacteria, can be found in a variety of environments and are naturally occurring in freshwater (3) and soil (5), because their life cycle typically involves endoparasitization and replication within eukaryotic host such as amoebae (6).
Incidence of LD has been rising consistently since the discovery of the disease (7), with a nearly 3.5-fold increase between 2000 and 2011 in the United States (8), 3 fold in Europe since 1995 (910), 2.5-fold increase between 2015 and 2016 in Korea (11), leading to legionellosis being considered an increasingly important disease from a public health standpoint.
Numerous factors could possibly contribute to an increase of notified LD cases in Europe, USA, and Korea. Previous studies have suggested that changing the environmental conditions, such as rainfall and temperature, can affect the incidence of sporadic community-acquired LD cases in Europe (121314). Additionally, population growth and increase in aging, which are accompanied with greater use of immunosuppressant drugs and higher incidence of comorbid conditions, are other important risk factors of incases in LD (15).
The objective of this study was to investigate the link between climatic changes and the prevalence of Legionella spp. and the incidence of Legionellosis in cooling towers and baths of public buildings in Seoul, Korea from 2013 to 2017.
Total 6,598 water samples were collected annually from the public use facilities from the 25 districts in Seoul, Korea between 2013 and 2017. Two litters of water samples were collected aseptically in sterile plastic containers and kept them at 6 −18℃ for transportation with light-free condition. The samples were categorized by their originated buildings, such as hospitals, decorative fountains, welfare facilities, subway, shopping malls, and department store.
One litter of water sample was filtered through 0.2-µm nitrocellulose membrane under vacuum. Each membrane was then placed on buffered charcoal yeast extract (BCYE) agar supplemented with L-cysteine and antibiotics followed by incubating for 10 days at 37℃. Colonies growing on BCYE agar, but not on blood agar, were identified as Legionella spp.
PCR analysis was performed to identify Legionella pneumophila and Legionella spp. by amplifying 16S rRNA and mip gene as described previously (Table 1) (1617). Amplification reactions were subjected to an initial denaturation step of 95℃ for 4 min, followed by 30 amplification cycles of 30 sec at 95℃, 30 sec at 55℃, and 30 sec at 72℃, followed by a final extension at 72℃ for 10 min.
Legionella isolates were identified by matrix assisted laser desorption and ionization time of flight mass spectrometry (MALDI-ToF; Bruker, Billerica, MA, USA) according to the manufacturer's protocols.
Legionellosis data were collected from the National Notifiable Diseases Surveillance System database of Korea Centers for Disease Control and Prevention (KCDC).
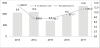
In total 6,598 water samples collected from 2013 to 2017 in Seoul, Korea, Legionella spp. were isolated by culture and identified by PCR and MALDI-TOF analysis. Legionella spp. was detected in 191 out of 1,092 (17.5%), 180 out of 1,015 (17.7%), 109 out of 920 (11.8%), 158 out of 1,149 (13.8%) and 306 out of 2,422 (12.6%) resulted positive to Legionella spp. by year indicating that an annual average isolation rate of Legionella spp. was 14.3% (Table 2).
Among 944 Legionella isolates, 17.7% (283 isolates out of 1,595 samples), 9.4% (190 isolate out of 2,025 samples), 19.3% (439 isolates out of 2,272 samples), 1.5% (2 isolates out of 132 samples), and 5.2% (30 isolates out of 574 samples) were isolated from cooling towers, hospitals, public bath, fountains, and others, respectively (Table 2).
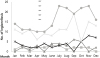
The surveillance of LD is coordinated by KCDC, and Legionellosis data were collected from the National Notifiable Diseases Surveillance System database of KCDC. The latest data from 2013 to 2017 revealed 443 cases of LD in Korean population. The incidence of LD steadily increased every year (Fig. 1). However, it must be noted that the incidence of LD in 2016 was increased 184.4% compared with previous year, 2015 (Fig. 1). The monthly distribution of LD case showed that it occurred throughout the year with peaks in September of 2014, November of 2015, September of 2016, and July and November of 2017 (Fig. 1).
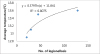
Correlation analysis between the incidence of LD and climatic factors showed no significant correlation except average temperature. The average temperature showed significantly positive linearity with the incidence of LD (R2=0.8075) (Table 3) (Fig. 2). In addition, changes in the isolation rate of Legionella spp. showed a similar trend to that of precipitation (P=0.708, ANOVA) (Fig. 3.).
During the summer of 2015, New York, NY, USA, had one of the largest and deadliest outbreaks of Legionnaires' disease in the history of the United States. A total of 138 cases and 16 deaths were linked to a single cooling tower in the South Bronx (18). Based on the increase in LD in Europe and Korea, we have explored the current knowledge about LD, engineering controls that might prevent future disease outbreaks and future research that is needed to investigate the seasonality of LD and its association with climatic factors to predict the epidemic in Korea (2). Reported LD incidence and patterns of disease can vary greatly based on political boundaries, potentially due to factors other than climate and geography (7).
Considering the high percentage of Legionella community-acquired infections, Italian and European literature data on Legionella contamination in air conditioning systems and hot water networks are available both for hospitals (1920), and small residential buildings (21). A previous report based on epidemiological data, suggests that one is more likely to contract legionellosis in public places, such as hospitals, hotels, and nursing homes in air conditioning systems, than in private ones (2223). Cooling towers are perhaps the most widely known source of legionellosis (2425). A relatively high proportion of detection rate, especially in cooling towers (17.7%) and public water bath (19.3%), is consistent with the results of other recent investigations on the Legionella distribution surveys (2627). The rapid increase in the number of cooling towers is the reason behind the recent large outbreaks, in the Bronx, NY, USA (28). Previous reports indicate that these devices can generate large volumes of aerosols from a heated water source that is frequently contaminated by Legionella, and their aerosols can be produced over extended periods of time and disseminated over long distances (2930). Legionellosis outbreaks have also been associated with water sources in the built environment including plumbing sources (e.g., showers, faucets, and toilets), cooling towers, respiratory devices (e.g., humidifiers, vaporizers, and nebulizers), swimming pools (including spas/hot tubs and whirlpools), steam-producing appliances, and ornamental fountains (23132333435).
Recently, a steady increase in LD has been described, and the increase has been reported to be consistent with the improvement in surveillance and effect of demographic change with increasing numbers of at-risk older people (13). Taken together, the reasons for this increase are unknown but might be partly a result of the increase in awareness about LD and the consequently increased testing for LD (923).
Usually, in the summer and fall season (July to November), an increase in the cased of LD has been noted. A monthly analysis of cases in order to determine the proportion of Legionella infected patients with LD in 2017, revealed a peak of LD infection in July. The reason for such a high prevalence could be explained based on 2015 MERS Outbreak in Korea that led to increased awareness, testing, and susceptibility of the population. Although, there is no direct evidence, we speculated increase in Legionella in the environment, or some combination of factors as the possible cause.
Several studies strongly suggested that LD occurs mainly in the summer months (2336373839404142). In the United States, 62% of LD cases occur during June–October (Centers for Disease Control and Prevention (43), a period of generally warm weather when commercial air conditioning systems, including those with cooling towers (CTs), are in operation (44). Our results suggest that the incidence of LD varies considerably based on meteorological data and local weather pattern. Previous studies have demonstrated the effects of seasonality and weather patterns on LD. And the associations among weather, particularly tempera-ture and humidity, drive the summer spike in incidence (36374041). In the regression analysis, the primary variables of interest- PM2.5 (µg/m3), NO2 (ppb), and number of the date of issue O3 warning precipitation - were not significant with LD except for average temperature (R2=0.8075 Legionella detection rate in Seoul, Korea showed a trend similar to precipitation (P=0.708, ANOVA). A similar pattern of occurrence of LD in warm (60°–80°F) and very humid (≥80.0%) months of was observed in a few reports (45). Increase in rainfall led to an increase in the risk of occurrence; however, regardless of rainfall, warm and humid weather were a major risk factors. (13233845). In the absence of any direct evidence, we speculated that Legionella spp. thrives in warm, and wet environments, which support the survival of the pathogen and existence of aerosolization.
Since 2000, LD has been designated as reportable infectious disease in Korea, and the incidence was between 0.04 and 0.09 per 100,000 people from 2010 to 2015 (46). However, there has been a rise in the number of annual reported cases, with an incidence of 0.39 per 100,000 people in 2017 (11). The reason for the rapid increase in remains unclear, although increased testing for differential diagnosis of pneumonia, enhancement in reporting, and growth of the old-age population are considered as probable contributing factors (47). In recent years, large outbreaks of LD such as in the Bronx, NY, USA (28), have raised public attention and generated momentum for stronger prevention efforts. There are many factors that contribute to the increased incidence of Legionnaires' disease. Although, there is no direct evidence, we speculated that people are at increased risk because of aging of the population, greater use of immunosuppressant drugs, and higher prevalence of comorbid conditions. It is also possible that the change in environmental conditions facilitates human exposure to aerosolized water containing Legionella spp. (15).
To reduce the incidence of LD, the World Health Organization and the US Center for Disease Control and Prevention have rec-ommended the development of a regular monitoring program for water systems where Legionella is most likely to thrive (4849). It is well established that the heating process can degrade the level of disinfectant (49). Although our work has several limitations, we expect that the results will be useful for the design of a preventive approach for the surveillance of Legionella.
In conclusion, our work is the first study to evaluate the link between climatic variables in Korea from 2013 to 2017, monthly incidence of legionellosis, and the prevalence of Legionella spp. in cooling towers in public building and public baths in Korea.
In summary, our study describes that the prevalence of the recent increase in legionellosis was associated with marked summertime seasonality. In the regression analysis, the primary variables of interest, PM2.5 (µg/m3), NO2 (ppb), and the number of days of issue O3 warning, were not significant except for average temperature (R2=0.8075). The Legionella detection rate in Seoul, Korea showed a trend similar to precipitation (P=0.708, ANOVA). Although further studies are needed, our finding is consistent with the contention that contamination of cooling towers and public water bath are important causes of legionellosis. Our data promotes a preventive approach for the surveillance of Legionella in Seoul, Korea.
Figures and Tables
Table 2
Number of Legionella pneumophila and Legionella spp. positive samples from the public facilities in Seoul, Korea from 2013 to 2017

aNumber of Legionella pneumophila and Legionella spp. positive water samples; bNumber of water samples collected and tested for Legionella spp.; cWater samples of colling tower were collcted from cooling tower basins of large shopping malls, department stores, hotels, and large buildings; dWater samples were collected from toilets and showers in hospitals; eWater samples were collected from taps, showers, and hot tubes of public bath houses; fWater samples were obtained from the decorative fountains in the parks and squares.
References
1. Phin N, Parry-Ford F, Harrison T, Stagg HR, Zhang N, Kumar K, et al. Epidemiology and clinical management of Legionnaires' disease. Lancet Infect Dis. 2014; 14:1011–1021.

2. Prussin AJ, Schwake DO, Marr LC. Ten questions concerning the aerosolization and transmission of Legionella in the built environment. Build Environ. 2017; 123:684–695.

3. Cazalet C, Jarraud S, Ghavi-Helm Y, Kunst F, Glaser P, Etienne J, et al. Multigenome analysis identifies a worldwide distributed epidemic Legionella pneumophila clone that emerged within a highly diverse species. Genome Res. 2008; 18:431–441.

4. Robertson P, Abdelhady H, Garduño RA. The many forms of a pleomorphic bacterial pathogen-the developmental network of Legionella pneumophila. Front Microbiol. 2014; 5:670.

5. Morris GK, Steigerwalt A, Feeley JC, Wong ES, Martin WT, Patton CM, et al. Legionella gormanii sp. nov. J Clin Microbiol. 1980; 12:718–721.
6. Rowbotham TJ. Current views on the relationships between amoebae, legionellae and man. Isr J Med Sci. 1986; 22:678–689.
7. Dooling KL, Toews KA, Hicks LA, Garrison LE, Bachaus B, Zansky S, et al. Active bacterial core surveillance for legionellosis-United States, 2011-2013. MMWR Morb Mortal Wkly Rep. 2015; 64:1190–1193.

8. Neil K, Berkelman R. Increasing incidence of legionellosis in the United States, 1990-2005: changing epidemiologic trends. Clin Infect Dis. 2008; 47:591–599.

9. Garrison LE, Kunz JM, Cooley LA, Moore MR, Lucas C, Schrag S, et al. Vital Signs: Deficiencies in Environmental Control Identified in Outbreaks of Legionnaires' Disease-North America, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016; 65:576–584.

10. European Centre for Disease Prevention and Control. Legionnaires' disease in Europe. 2016. Retrieved from http://ecdc.europa.eu/en/publications/Publications/legionnaires-disease-2015.pdf.
11. Korea Centers for Disease Control and Prevention. 10th January 2018. Last modified: http://is.cdc.go.kr.
12. Sakamoto R. Legionnaire's disease, weather and climate. Bull World Health Organ. 2015; 93:435–436.

13. Beauté J, Sandin S, Uldum SA, Rota MC, Brandsema P, Giesecke J, et al. Short-term effects of atmospheric pressure, temperature, and rainfall on notification rate of community-acquired Legionnaires' disease in four European countries. Epidemiol Infect. 2016; 144:3483–3493.

14. European Environment Agency. Climate change, impacts and vulnerability in Europe 2012 an indicator based report. Luxembourg: EEA;2012. 2012. Retrieved from www.eea.europa.eu/publications/climate-impacts-and-vulnerability-2012/at_download/file.
15. Ruth LB, Amy P. Prevention of Legionnaires' Disease in the 21st Century by Advancing Science and Public Health Practice. Emerg Infect Dis. 2017; 23:1905–1907.

16. Lindsay DS, Abraham WH, Fallon RJ. Detection of mip gene by PCR for diagnosis of Legionnaires' disease. J Clin Microbiol. 1994; 32:3068–3069.

17. Jeon SJ, Jung JH, Jin YH, Lee JK, Oh YH, Choi SM. Molecular Epidemiology of Legionella pneumophila Isolated from Bath Facilities of Public Establishments in Seoul. J Bacteriol Virol. 2011; 41:295–300.

18. Lapierre P, Nazarian E, Zhu Y, Wroblewski D, Saylors A, Passaretti T, et al. Legionnaires' Disease Outbreak Caused by Endemic Strain of Legionella pneumophila, New York, New York, USA, 2015. Emerg Infect Dis. 2017; 23:1784–1791.

19. Casini B, Buzzigoli A, Cristina ML, Spagnolo AM, Del Giudice P, Brusaferro S, et al. Long-term effects of hospital water network disinfection on Legionella and other waterborne bacteria in an Italian university hospital. Infect Control Hosp Epidemiol. 2014; 35:293–299.

20. Cristina ML, Spagnolo AM, Casini B, Baggiani A, Del Giudice P, Brusaferro S, et al. The impact of aerators on water contamination by emerging gram-negative opportunists in at-risk hospital departments. Infect Control Hosp Epidemiol. 2014; 35:122–129.

21. Whiley H. Legionella risk management and control in potable water systems: Argument for the abolishment of routine testing. Int J Environ Res Public Health. 2016; 14:E12.

22. Muder RR, Yu VL, Woo AH. Mode of transmission of Legionella pneumophila. A critical review. Arch Intern Med. 1986; 146:1607–1612.

23. Fields BS, Benson RF, Besser RE. Legionella and Legionnaires' disease: 25 years of investigation. Clin Microbiol Rev. 2002; 15:506–526.

24. Weiss D, Boyd C, Rakeman JL, Greene SK, Fitzhenry R, McProud T, et al. A Large Community Outbreak of Legionnaires' Disease Associated With a Cooling Tower in New York City, 2015. Public Health Rep. 2017; 132:241–250.

25. Walser SM, Gerstner DG, Brenner B, Höller C, Liebl B, Herr CE. Assessing the environmental health relevance of cooling towers--a systematic review of legionellosis outbreaks. Int J Hyg Environ Health. 2014; 217:145–154.

26. Lee HK, Shim JI, Kim HE, Yu JY, Kang YH. Distribution of Legionella species from environmental water sources of public facilities and genetic diversity of L. pneumophila serogroup 1 in South Korea. Appl Environ Microbiol. 2010; 76:6547–6554.

27. Kim C, Jeon S, Jung J, Oh Y, Kim Y, Lee J, et al. Isolation of Legionella pneumophila from cooling towers, public baths, hospitals, and fountains in Seoul, Korea, from 2010 to 2012. J Environ Health. 2015; 77:58–62.
28. Fitzhenry R, Weiss D, Cimini D, Balter S, Boyd C, Alleyne L, et al. Legionnaires' disease outbreaks and cooling towers, New York City, New York, USA. Emerg Infect Dis. 2017; 23:1769–1776.

29. Ferré MR, Arias C, Oliva JM, Pedrol A, García M, Pellicer T, et al. A Community outbreak of Legionnaires' disease associated with a cooling tower in Vic and Gurb, Catalonia (Spain) in 2005. Eur J Clin Microbiol Infect Dis. 2009; 28:153–159.

30. Türetgen I, Sungur EI, Cotuk A. Enumeration of Legionella pneumophila in cooling tower water systems. Environ Monit Assess. 2005; 100:53–58.

31. Den Boer JW, Yzerman EP, Schellekens J, Lettinga KD, Boshuizen HC, Van Steenbergen JE, et al. A large outbreak of Legionnaires' disease at a flower show, the Netherlands, 1999. Emerg Infect Dis. 2002; 8:37–43.

32. O'Loughlin RE, Kightlinger L, Werpy MC, Brown E, Stevens V, Hepper C, et al. Restaurant outbreak of Legionnaires' disease associated with a decorative fountain: an environmental and case-control study. BMC Infect Dis. 2007; 7:93.
33. Haupt TE, Heffernan RT, Kazmierczak JJ, Nehls-Lowe H, Rheineck B, Powell C, et al. An outbreak of Legionnaires disease associated with a decorative water wall fountain in a hospital. Infect Control Hosp Epidemiol. 2012; 33:185–191.

34. Richard LT, Eva SL, Elicia KB, Donald KM, James MB. Home humidifiers as a potential source of exposure to microbial pathogens, endotoxins, and allergens. Indoor Air. 1995; 5:171–178.

35. Hines SA, Chappie DJ, Lordo RA, Miller BD, Janke RJ, Lindquist HA, et al. Assessment of relative potential for Legionella species or surrogates inhalation exposure from common water uses. Water Res. 2014; 56:203–213.

36. Fisman DN, Lim S, Wellenius GA, Johnson C, Britz P, Gaskins M, et al. It's not the heat, it's the humidity: wet weather increases legionellosis risk in the greater Philadelphia metropolitan area. J Infect Dis. 2005; 192:2066–2073.

37. Hicks LA, Rose CE Jr, Fields BS, Drees ML, Engel JP, Jenkins PR, et al. Increased rainfall is associated with increased risk for legionellosis. Epidemiol Infect. 2007; 135:811–817.

38. Gleason JA, Kratz NR, Greeley RD, Fagliano JA. Under the weather: legionellosis and meteorological factors. EcoHealth. 2016; 13:293–302.

39. Farnham A, Alleyne L, Cimini D, Balter S. Legionnaires' disease incidence and risk factors, New York, New York, USA, 2002–2011. Emerg Infect Dis. 2014; 20:1795–1802.

40. Ricketts KD, Charlett A, Gelb D, Lane C, Lee JV, Joseph CA. Weather patterns and Legionnaires' disease: a meteorological study. Epidemiol Infect. 2009; 137:1003.

41. Karagiannis I, Brandsema P, Van Der Sande M. Warm, wet weather associated with increased Legionnaires' disease incidence in the Netherlands. Epidemiol Infect. 2009; 137:181–187.

42. Brandsema PS, Euserm SM, Karagiannis I, Den Boer JW, Van Der Hoek W. Summer increase of Legionnaires' disease 2010 in The Netherlands associated with weather conditions and implications for source finding. Epidemiol Infect. 2014; 142:2360–2371.

43. Centers for Disease Control and Prevention (CDC). Legionellosis-United States, 2000–2009. MMWR Morb Mortal Wkly Rep. 2011; 60:1083–1086.
44. Bhopal RS, Fallon RJ, Buist EC, Black RJ, Urquhart JD. Proximity of the home to a cooling tower and risk of non-outbreak Legionnaires' disease. BMJ. 1991; 302:378–383.

45. Simmering JE, Polgreen LA, Hornick DB, Sewell DK, Polgreen PM. Weather-Dependent Risk for Legionnaires' Disease, United States. Emerg Infect Dis. 2017; 23:1843–1851.

46. Korea Centers for Disease Control and Prevention. Guideline of Legionnaires' disease. Cheongju: KCDC;2016. p. 20–73.
47. Ameneshoa W, Lee JH, Carlo JT. Community-acquired Legionnaires' disease in Dallas county, Texas. J Environ Health. 2016; 78:E1–E6.
48. American Institute of Architects. Guidelines for design and construction of hospital and health care facilities, 2001. 2017. Retrieved from https://www.fgiguidelines.org/wp-content/uploads/2015/08/2001guidelines.pdf.
49. Demirjian A, Lucas CE, Garrison LE, Kozak-Muiznieks NA, States S, Brown EW, et al. The importance of clinical surveillance in detecting legionnaires’ disease outbreaks: a large outbreak in a hospital with a Legionella disinfection system-Pennsylvania, 2011-2012. Clin Infect Dis. 2015; 60:1596–1602.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download