Dear Editor,
P antigens, including P, P1, and Pk, are carbohydrate antigens. More than 99.9% of the population worldwide has the P1 (P+P1+Pk+) or P2 (P+P1−Pk+) phenotype; however, rarely, an individual may not express P antigens at all. In Europeans, the frequency of the p phenotype is approximately 5.8 in 1,000,000 [1]. However, its frequency in Asians remains difficult to predict because very few cases have been reported in the Japanese, Chinese, and Taiwanese populations [23456]. Individuals with this phenotype can develop naturally occurring anti-PP1Pk antibodies, which are clinically relevant and cause hemolytic transfusion reactions or hemolytic diseases of the fetus and newborn [7]. We report the first case with anti-PP1Pk antibodies in Korea.
In June 2018, a 66-year-old Korean woman was referred to Samsung Medical Center, Seoul, Korea, for a mass-like lesion found in the gallbladder through abdominal ultrasonography. Gallbladder malignancy was suspected in the magnetic resonance imaging result. Surgical management of malignancy was scheduled in July 2018, and screening studies were carried out. Her blood type was group A, D-positive. She had no known history of transfusion. However, antibody screening and identification tests using column agglutination (Bio-Rad, Cressier, Switzerland) showed panagglutination of uniform strength (3+) at 37℃ Coombs phase and 4℃ enzyme (papain) phase. Negative reactions to autologous red blood cells (RBCs) were observed, indicating the presence of alloantibodies to high-frequency antigens. The specimen obtained from the patient was sent to the central laboratory of the Swiss Red Cross (Bern, Switzerland) to identify alloantibodies to high-frequency antigens. The patient tested negative for P, P1, and Pk antigens, and anti-PP1Pk antibodies were observed. Autologous blood, blood from siblings lacking the rare-blood-group antigen, or allogenic blood (fresh or cryopreserved) from rare donor programs were considered for the patient's blood management. However, neither cryopreserved blood nor suitable blood donors were available. Therefore, the transfusion team at our hospital recommended the surgical team to postpone the surgery to prepare autologous blood via preoperative autologous deposit. However, our medical team chose an acute normovolemic hemodilution (ANH) without changing the surgery schedule. This procedure is simple and inexpensive and has the advantage that fresh autologous blood is readily available [8]. The patient's preoperative Hb and Hct levels were 129 g/L and 39.8%, respectively. Her estimated blood volume was calculated as 4,156 mL, using Nadler's equation [9]. Since our target Hct level was 33%, 800 mL of blood was drawn in one step through a radial arterial catheter into two 400-mL blood bags containing citrate-phosphate-dextrose-A solution after anesthetic induction. An equal volume of 6% hydroxyethyl starch solution was infused simultaneously through a separate intravenous line during the procedure. The patient underwent radical cholecystectomy and liver wedge resection with lymph node dissection, and two units of autologous blood were re-infused back to the patient during surgery. She was discharged 48 hours later with Hb level of 123 g/L.
A family study was performed with P1 phenotyping using anti-P1 serum (Ortho Clinical Diagnostics, Raritan, NJ, USA), by crossmatching with the patient's plasma containing anti-PP1Pk antibodies, and sequencing of the A4GALT gene [2]. This study was approved by the Institutional Review Board of Samsung Medical Center, Seoul, Korea (SMC 2018-08-098). In P1 phenotyping, the patient and her brother were negative, her sister was 2+, and her husband and two sons were 4+. In crossmatching between serum of the proband and RBCs of each family member, only her brother was negative. However, we could not exclude the effects of ABO blood group antibodies on crossmatching. The patient and her brother were homozygous for c.1029dupC, indicating a rare p phenotype. The test results for the patient and her family members are shown in Fig. 1.
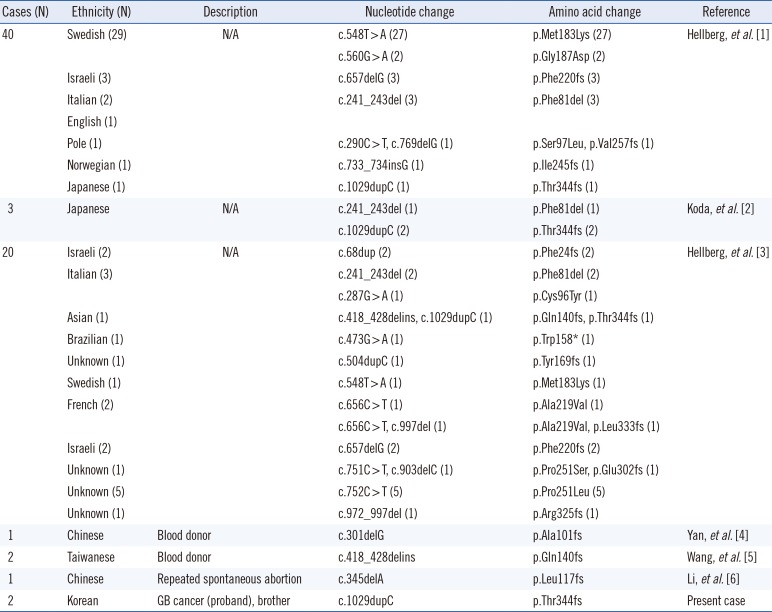
Representative cases with anti-PP1Pk antibodies, the p phenotype, and A4GALT mutation are described in Table 1. Mutation of the A4GALT gene results in changes in the protein product, inducing the rare p phenotype, regardless of the status of the B3GALNT1 gene. A single-base pair duplication (c.1029dupC) was first reported in a Japanese individual [2]; this one-base pair duplication causes a reading frame shift and loss of the stop codon, resulting in a gene product with an additional 92 amino acids. We found the c.1029dupC mutation in the proband and her brother.
Anti-PP1Pk antibodies can be produced in individuals with the p phenotype without exposure to P antigens through transfusion or pregnancy. Anti-PP1Pk antibody positivity in patients without a history of P antigen exposure have been reported [45]. Our patient had delivered two children fathered by her non-p phenotype husband (P1 antigen positivity was confirmed by P1 phenotyping), but she had no history of transfusion. Her brother also had no history of transfusion but showed anti-PP1Pk antibody positivity.
Our report on the first case of anti-PP1Pk antibody positivity in the Korean population demonstrates that autologous transfusion via ANH is a good alternative to allogenic transfusion in patients alloimmunized to high-frequency antigens. Further investigations are needed on the effect of ANH on hemostasis and on applying ANH to a broader spectrum of patients, such as those on dialysis.
Acknowledgment
We thank the Central Laboratory of the Swiss Red Cross (Bern, Switzerland) for their help with identifying the antibody.
References
1. Hellberg A, Steffensen R, Yahalom V, Sojka BN, Heier HE, Levene C, et al. Additional molecular bases of the clinically important p blood group phenotype. Transfusion. 2003; 43:899–907. PMID: 12823750.
2. Koda Y, Soejima M, Sato H, Maeda Y, Kimura H. Three-base deletion and one-base insertion of the alpha(1,4)galactosyltransferase gene responsible for the P phenotype. Transfusion. 2002; 42:48–51. PMID: 11896312.
3. Hellberg A, Ringressi A, Yahalom V, Safwenberg J, Reid ME, Olsson ML. Genetic heterogeneity at the glycosyltransferase loci underlying the GLOB blood group system and collection. Br J Haematol. 2004; 125:528–536. PMID: 15142124.
4. Yan L, Zhu F, Xu X, Zantek ND. Molecular basis for p blood group phenotype in China. Transfusion. 2004; 44:136–138. PMID: 14692982.
5. Wang YC, Chang CF, Lin HC, Lin KS, Lin KT, Hung CM, et al. Functional characterisation of a complex mutation in the alpha(1,4)galactosyltransferase gene in Taiwanese individuals with p phenotype. Transfus Med. 2011; 21:84–89. PMID: 21092013.
6. Li X, Diao X, Xia X, Hong X, Zhu F. A novel mutation in A4GALT was identified in a Chinese individual with p phenotype. Transfusion. 2017; 57:215–216. PMID: 27612185.
7. Fung MK EA, Spitalnik SL, et al. Technical Manual. 19th ed. Bethesda, Maryland: American Association of Blood Banks;2018. p. 286–290.
8. Matot I, Scheinin O, Jurim O, Eid A. Effectiveness of acute normovolemic hemodilution to minimize allogeneic blood transfusion in major liver resections. Anesthesiology. 2002; 97:794–800. PMID: 12357142.
9. Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962; 51:224–232. PMID: 21936146.
Fig. 1
Family study results of the anti-PP1Pk family. (A) P1 phenotype pedigree based on standard serologic method. The proband is indicated by an arrow. (B) Sequencing results were determined on the basis of the combined data from PCR and sequencing of A4GALT gene. The affected individuals (II-1, II-4) were homozygous for c.1029dupC. The carrier individual (II-3) was heterozygous for c.1029dupC but also carried another allele with a combined normal.
Abbreviation: dup, duplication.
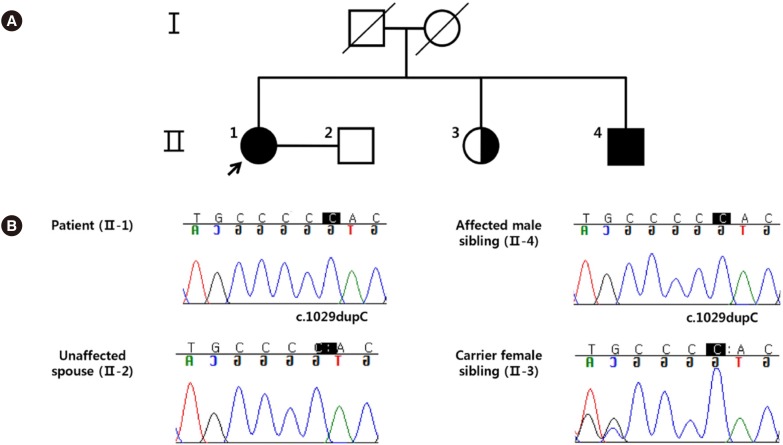
Table 1
Representative published cases with anti-PP1Pk, p-phenotype, and A4GALT mutation confirmed by genotyping
| Cases (N) | Ethnicity (N) | Description | Nucleotide change | Amino acid change | Reference |
|---|---|---|---|---|---|
| 40 | Swedish (29) | N/A | c.548T > A (27) | p.Met183Lys (27) | Hellberg, et al. [1] |
| c.560G > A (2) | p.Gly187Asp (2) | ||||
| Israeli (3) | c.657delG (3) | p.Phe220fs (3) | |||
| Italian (2) | c.241_243del (3) | p.Phe81del (3) | |||
| English (1) | |||||
| Pole (1) | c.290C > T, c.769delG (1) | p.Ser97Leu, p.Val257fs (1) | |||
| Norwegian (1) | c.733_734insG (1) | p.Ile245fs (1) | |||
| Japanese (1) | c.1029dupC (1) | p.Thr344fs (1) | |||
| 3 | Japanese | N/A | c.241_243del (1) | p.Phe81del (1) | Koda, et al. [2] |
| c.1029dupC (2) | p.Thr344fs (2) | ||||
| 20 | Israeli (2) | N/A | c.68dup (2) | p.Phe24fs (2) | Hellberg, et al. [3] |
| Italian (3) | c.241_243del (2) | p.Phe81del (2) | |||
| c.287G > A (1) | p.Cys96Tyr (1) | ||||
| Asian (1) | c.418_428delins, c.1029dupC (1) | p.Gln140fs, p.Thr344fs (1) | |||
| Brazilian (1) | c.473G > A (1) | p.Trp158* (1) | |||
| Unknown (1) | c.504dupC (1) | p.Tyr169fs (1) | |||
| Swedish (1) | c.548T > A (1) | p.Met183Lys (1) | |||
| French (2) | c.656C > T (1) | p.Ala219Val (1) | |||
| c.656C > T, c.997del (1) | p.Ala219Val, p.Leu333fs (1) | ||||
| Israeli (2) | c.657delG (2) | p.Phe220fs (2) | |||
| Unknown (1) | c.751C > T, c.903delC (1) | p.Pro251Ser, p.Glu302fs (1) | |||
| Unknown (5) | c.752C > T (5) | p.Pro251Leu (5) | |||
| Unknown (1) | c.972_997del (1) | p.Arg325fs (1) | |||
| 1 | Chinese | Blood donor | c.301delG | p.Ala101fs | Yan, et al. [4] |
| 2 | Taiwanese | Blood donor | c.418_428delins | p.Gln140fs | Wang, et al. [5] |
| 1 | Chinese | Repeated spontaneous abortion | c.345delA | p.Leu117fs | Li, et al. [6] |
| 2 | Korean | GB cancer (proband), brother | c.1029dupC | p.Thr344fs | Present case |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download