Dear Editor,
Trueperella spp. are facultative anaerobic gram-positive bacilli usually found in the mammalian genital tract [1]. Of the five Trueperella spp., T. bernardiae and T. pyogenes have been isolated in human clinical specimens [23]. T. bernardiae has been reported as an opportunistic pathogen in chronic osteitis, prosthetic joint infection, and brain abscess cases [456]. However, bloodstream infections caused by T. bernardiae have been reported in only a few cases, mostly in immunocompromised patients [78]. We report the first case of T. bernardiae bacteremia in Korea. The Institutional Review Board for Human Research, Yonsei University, Severance Hospital, Seoul, Korea, approved this study (approval number: 4-2019-0343) and waived the need for informed consent.
An 83-year old woman with a history of diabetes mellitus, cerebrovascular disease, and paroxysmal atrial fibrillation was transferred to the emergency room at Severance Hospital from a geriatric hospital because of uncontrolled fever and hypotension in August 2016. Three days prior to admission, she had been treated with fluoroquinolone (200 mg, twice a day) in the geriatric hospital because of a Klebsiella pneumoniae urinary tract infection. In the emergency room, her mean blood pressure was 42 mmHg, heart rate was 58 beats/minutes, and body temperature was 35.8℃. Laboratory tests showed a blood leukocyte count of 14.73×109/L, neutrophil count of 13.04×109/L (88.5% of total leukocyte count), C-reactive protein (CRP) level of 1,668.57 nmol/L, and procalcitonin level of 3.91 µg/L. As K. pneumoniae septic shock was suspected, empirical antimicrobial treatment with meropenem was initiated. Ten milliliter of blood were collected in three sets of culture vials, including BacT/Alert FA Plus (bioMérieux, Marcy-l'Étoile, France) and BacT/Alert FN Plus (bioMérieux), which were incubated in a BacT/ALERT 3D automated blood culture system (bioMérieux) immediately. After four-day incubation, positive signals for bacterial growth were identified in two FA and two FN culture vials. Gram-positive cocci and gram-positive bacilli were observed on the smear preparation from the positive-signal culture vials. Following subculturing on blood agar, white, medium-sized colonies and grayish, pinpoint colonies were observed. The bacterial species were identified as S. aureus (identification log score: 2.163) and T. bernardiae (identification log score: 1.981), respectively, using a Bruker Biotyper matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) system (Bruker Daltonics, Bremen, Germany). Because of the low identification log score (under 2.0) for the latter isolate, indicating correct identification at the genus level, the 1,366 bp 16S rRNA gene was sequenced by Sanger sequencing and compared with the ezBiocloud database (https://www.ezbiocloud.net/identify). This showed 99.85% identity with GenBank sequence X79224 (T. bernardiae). Anti-microbial susceptibility was determined via gradient diffusion using an ETEST strip (bioMérieux) on Mueller-Hinton agar (Difco Laboratories, Detroit, MI, USA), according to the CLSI guidelines [9]. The isolate was resistant to penicillin G (minimum inhibitory concentration [MIC], 4 µg/mL) and erythromycin (MIC, 3 µg/mL) and was susceptible to gentamicin (MIC, 0.023 µg/mL) and vancomycin (MIC, 0.38 µg/mL).
A follow-up blood culture on the third day of hospitalization showed continual growth of both S. aureus and T. bernardiae; thus, antimicrobial treatment with teicoplanin (400 mg, once a day) was initiated. After 11 days of teicoplanin treatment, the patient's mean blood pressure was 93 mmHg, her fever subsided, and CRP level decreased to 69.52 nmol/L. The follow-up blood culture was also negative for bacterial growth. Following conservative management, the patient was discharged 47 days post-admission.
As the number of immunocompromised patients has increased rapidly over the past decades, microorganisms previously considered to be commensal are now regarded as significant pathogens [10]. Coryneform gram-positive bacilli are common flora of the skin and have been considered contaminants when recovered from blood cultures [8]. However, in our case, T. bernardiae isolates were identified from multiple sets of blood culture vials and two consecutive blood cultures on separate days. In addition, clinical improvement and bacterial elimination were observed following appropriate antimicrobial treatment. Therefore, we conclude that in our case, T. bernardiae constitutes a clinically significant pathogen rather than an incidental contaminant.
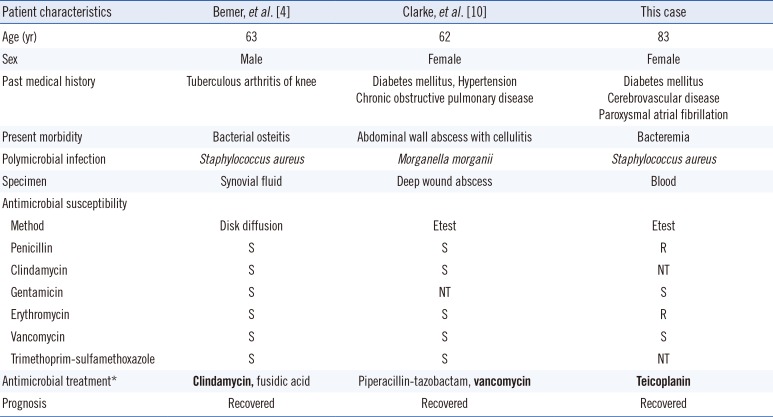
Whether the interaction between T. bernardiae and other bacteria is synergistic or competitive is not clear. Polymicrobial infection of T. bernardiae with other bacteria has been previously reported (Table 1). Bemer, et al. [4] reported a case of an immunocompromised patient with chronic osteitis caused by polymicrobial infection, and Clarke, et al. [10] reported a case of necrotizing fasciitis caused by Morganella morganii and T. bernardiae co-infection. Because of the slow growing nature of T. bernardiae, other co-infecting bacteria could hinder accurate diagnosis of T. bernardiae infection. In addition, adequate antimicrobial treatment effective against T. bernardiae infection should be considered for immunocompromised patients, although this bacterium is considered to be less virulent than others. In this case, the anti-staphylococcal agents effectively treated the T. bernardiae infection.
In conclusion, we report a case of T. bernardiae bacteremia confirmed by MALDI-TOF MS and 16S rRNA sequencing. This case increases our understanding on T. bernardiae and its pathogenicity in immunocompromised patients.
References
1. Hijazin M, Ulbegi-Mohyla H, Alber J, Lämmler C, Hassan AA, Timke M, et al. Identification of Arcanobacterium (Trueperella) abortisuis, a novel species of veterinary importance, by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS). Berl Munch Tierarztl Wochenschr. 2012; 125:32–37. PMID: 22372322.
2. Gahrn-Hansen B, Frederiksen W. Human infections with Actinomyces pyogenes (Corynebacterium pyogenes). Diagn Microbiol Infect Dis. 1992; 15:349–354. PMID: 1611850.
3. Weitzel T, Braun S, Porte L. Arcanobacterium bernardiae bacteremia in a patient with deep soft tissue infection. Surg Infect (Larchmt). 2011; 12:83–84. PMID: 21166597.
4. Bemer P, Eveillard M, Touchais S, Redon H, Corvec S. A case of osteitis due to Staphylococcus aureus and Arcanobacterium bernardiae coinfection. Diagn Microbiol Infect Dis. 2009; 63:327–329. PMID: 19097838.
5. Gilarranz R, Chamizo F, Horcajada I, Bordes-Benítez A. Prosthetic joint infection caused by Trueperella bernardiae. J Infect Chemother. 2016; 22:642–644. PMID: 26964529.
6. Parha E, Alalade A, David K, Kaddour H, Degun P, Namnyak S. Brain abscess due to Trueperella bernardiae. Br J Neurosurg. 2015; 29:728–729. PMID: 25833264.
7. Schneider UV, Ekenberg C, Sode N, Knudsen JD. A case of diabetic foot ulcers complicated by severe infection and sepsis with Trueperella bernardiae. JMM Case Rep. 2015; 2.
8. Weitzel T, Braun S, Porte L. Arcanobacterium bernardiae bacteremia in a patient with deep soft tissue infection. Surg Infect (Larchmt). 2011; 12:83–84. PMID: 21166597.
9. CLSI. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria. 3rd ed. Wayne, PA: Clinical and Laboratory Standards Institute;2015. CLSI M45-A3.
10. Clarke TM, Citron DM, Towfigh S. The conundrum of the gram-positive rod: are we missing important pathogens in complicated skin and soft-tissue infections? A case report and review of the literature. Surg Infect (Larchmt). 2010; 11:65–72. PMID: 19803730.
Table 1
Previous reports of polymicrobial infection of Trueperella bernardiae with other bacteria
| Patient characteristics | Bemer, et al. [4] | Clarke, et al. [10] | This case |
|---|---|---|---|
| Age (yr) | 63 | 62 | 83 |
| Sex | Male | Female | Female |
| Past medical history | Tuberculous arthritis of knee | Diabetes mellitus, Hypertension Chronic obstructive pulmonary disease | Diabetes mellitus Cerebrovascular disease Paroxysmal atrial fibrillation |
| Present morbidity | Bacterial osteitis | Abdominal wall abscess with cellulitis | Bacteremia |
| Polymicrobial infection | Staphylococcus aureus | Morganella morganii | Staphylococcus aureus |
| Specimen | Synovial fluid | Deep wound abscess | Blood |
| Antimicrobial susceptibility | |||
| Method | Disk diffusion | Etest | Etest |
| Penicillin | S | S | R |
| Clindamycin | S | S | NT |
| Gentamicin | S | NT | S |
| Erythromycin | S | S | R |
| Vancomycin | S | S | S |
| Trimethoprim-sulfamethoxazole | S | S | NT |
| Antimicrobial treatment* | Clindamycin, fusidic acid | Piperacillin-tazobactam, vancomycin | Teicoplanin |
| Prognosis | Recovered | Recovered | Recovered |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download