Dear Editor,
Periodic monitoring of blood volume is a key performance indicator of high-quality blood culture procedures [1]. Although blood volume is the most important factor for successful blood culture [2], its measurement remains challenging. Automatic measurement of blood volume is currently possible because of technical developments and software advances. BACTEC FX (Becton-Dickinson Microbiology Systems, Sparks, MD, USA) calculates blood volume by measuring the CO2 production of red blood cells in ≥25 bottles [34]. However, its accuracy is significantly affected by low Hct (<30%) values [4]. The recently developed BacT/Alert Virtuo instrument (bioMérieux, Marcy l'Étoile, France) can measure blood volume by scanning the sample level of each bottle. This is the first study to evaluate the accuracy of blood volume measured by this instrument. We compared the volume measured using the Virtuo instrument (henceforth, virtual volume) with the volume determined by weighing each bottle with a scale and dividing it by 1.055, the specific gravity of whole blood (henceforth, actual volume) [5].
A total of 1,212 blood culture bottles were collected between September and December 2018 from Gyeongsang National University Changwon Hospital, Changwon, Korea. We used the Virtuo instrument (version 02.01.06.928) with Myla middleware (version 4.0.0.29; bioMérieux), which improves connectivity, laboratory workflow, and information management. Virtual volume of each bottle is automatically presented as an integer by the instrument.
Statistical analyses were performed using MedCalc for Windows, version 18.5 (MedCalc Software, Ostend, Belgium), and P<0.05 was considered significant. We used the Kolmogorov-Smirnov test for testing normal distribution and applied the interquartile range (IQR) rule to detect outliers (below the first quartile−1.5×IQR or above the third quartile+1.5×IQR). The Mann-Whitney test was used to compare the volume of aerobic and anaerobic bottles, and the Wilcoxon signed rank test was used to compare paired virtual and actual volumes. Spearman's rank correlation was calculated between virtual and actual volumes.
We excluded 71 outliers and analyzed the remaining 1,141 bottles (543 aerobic and 598 anaerobic). Median virtual volume was 6.0 (4.0–7.0) mL for all bottles and differed between aerobic and anaerobic bottles (6.0 [5.0–7.0] mL vs 5.0 [3.0–6.0] mL; P<0.0001). Median actual volume was 4.83 (3.70–5.88) mL for all bottles and did not differ significantly between aerobic and anaerobic bottles (4.83 [3.70–5.97] mL vs 4.79 [3.60–5.78] mL; P=0.7401). The optimal volume (8–12 mL) accounted for only 16.0% and 5.0% of virtual and actual volume, respectively (Fig. 1). Of all bottles, 400 pairs of aerobic and anaerobic bottles were collected from the same patients at the same time, and they had a median actual volume of 9.91 (7.87–11.09) mL.
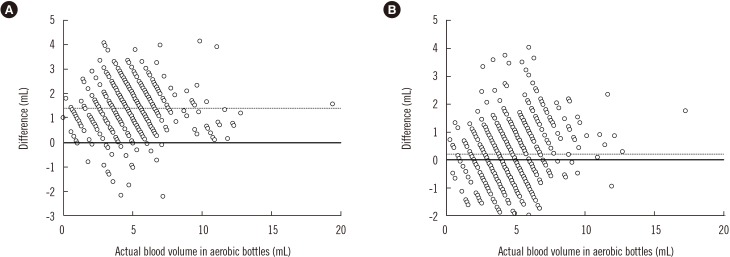
Virtual and actual volumes were strongly correlated (r=0.875 and 0.882 for aerobic and anaerobic bottles, respectively). The differences between virtual and actual volumes were larger in aerobic (median difference: 1.40 [0.82–1.88] mL) than in anaerobic (0.21 [−0.46–0.88] mL) bottles (P<0.0001; Fig. 2).
More blood was collected in aerobic than anaerobic bottles, in agreement with a previous report [6]. This phenomenon might be due to the initial inoculation in the aerobic bottles [2].
Another study on Aerobic/F bottles using BACTEC FX found a 0.2 mL difference between virtual and actual volume and a strong correlation between them (R2=0.715) [7]. Yet another study found a 0.3 mL difference using the same instrument [4]. We found a significant difference between virtual and actual volume in both types of bottles. However, the median difference in aerobic bottles (1.40 mL; 95% CI, 1.31–1.45) was greater than that in anaerobic bottles (0.21 mL; 95% CI, 0.07–0.31).
There is a need for caution in evaluating the adequacy of blood volume based on virtual volume because of the possibility of overestimation.
References
1. Lamy B, Ferroni A, Henning C, Cattoen C, Laudat P. How to: accreditation of blood cultures' proceedings. A clinical microbiology approach for adding value to patient care. Clin Microbiol Infect. 2018; 24:956–963. PMID: 29410246.
2. CLSI. Principles and procedures for blood cultures; approved guideline. M47-A. Wayne, PA: Clinical and Laboratory Standards Institute;2007.
3. Coorevits L, Van den Abeele AM. Evaluation of the BD BACTEC FX blood volume monitoring system as a continuous quality improvement measure. Eur J Clin Microbiol Infect Dis. 2015; 34:1459–1466. PMID: 25894984.
4. Cattoir L, Claessens J, Cartuyvels R, Van den Abeele AM. How to achieve accurate blood culture volumes: the BD BACTEC FX blood volume monitoring system as a measuring instrument and educational tool. Eur J Clin Microbiol Infect Dis. 2018; 37:1621–1626. PMID: 29882176.
5. Trudnowski RJ, Rico RC. Specific gravity of blood and plasma at 4 and 37 degrees C. Clin Chem. 1974; 20:615–616. PMID: 4826961.
6. Jones RL, Sayles HR, Fey PD, Rupp ME. Effect of clinical variables on the volume of blood collected for blood cultures in an adult patient population. Infect Control Hosp Epidemiol. 2017; 38:1493–1497. PMID: 29157318.
7. Chang J, Park JS, Park S, Choi B, Yoon NS, Sung H, et al. Impact of monitoring blood volume in the BD BACTEC FX blood culture system: virtual volume versus actual volume. Diagn Microbiol Infect Dis. 2015; 81:89–93. PMID: 25433403.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download