Dear Editor,
CLL is a type of small cell lymphoma characterized by massive accumulation of mature CD5+ B lymphocytes in peripheral blood, bone marrow, spleen, and lymph nodes [1]. CML is a chronic clonal myeloproliferative disease characterized by the fusion of the BCR-ABL oncogene on the reciprocal translocation t(9;22)(q34;q11.2) [2]. Simultaneous occurrence of CLL and CML in the same patient has been documented [345]. Occurrence of CML as a secondary malignancy in the course of CLL after treatment with cytotoxic drugs has also been reported [345]. However, the prognosis of these diseases and whether the two leukemias are derived from the same clonal cells are yet to be elucidated [6]. We describe the first case with immunoglobulin heavy chain variable (IGHV) region gene mutation, positive for CLL without chemotherapy-mediated transformation into CML, in a patient who showed a favorable response to imatinib treatment while the IGHV-mutation was still present. The Institutional Review Board of The Second Affiliated Hospital of Fujian Medical University, Quanzhou, China, approved the study (approval no. 2018061). Informed consent was obtained from the patient.
An 80-year-old Chinese man was admitted to the Department of Hematology, The Second Affiliated Hospital of Fujian Medical University, in July 2012 for leukocytosis. Physical and computed tomography examinations showed mild splenomegaly and no lymphadenomegaly and hepatomegaly. Blood examination revealed a leukocyte count of 23.53×109/L with 81% lymphocytes, 16% neutrophils, 3% monocytes; Hb level of 147 g/L; and a platelet count of 167×109/L. The absolute lymphocyte count was 19.07×109/L. Peripheral blood flow cytometry revealed 48.9% of analyzed cells co-expressing CD5, CD19, and CD23 but lacking surface immunoglobulin light chains, FMC7, CD10, CD103, and CD38. Bone marrow aspirate and biopsy showed hypercellular bone marrow with diffuse interstitial and focal paratrabecular lymphocytic infiltrate. The lymphocytes were mature, small, and positive for CD19, CD79a, PAX-5, CD5, CD23, and CD20 but negative for cyclin D1 and CD10. Conventional cytogenetic tests and FISH revealed a normal karyotype with no additional karyotypic abnormalities. IGHV gene mutation was positive by multiplex PCR [7]. However, the TP53 mutation and deletion were not detected. The patient was diagnosed as having Rai stage II and Binet stage A CLL in August 2012. The patient chose treatment with watch and wait. He remained under surveillance until June 2017, when he developed anemia and significant constitutional symptoms.
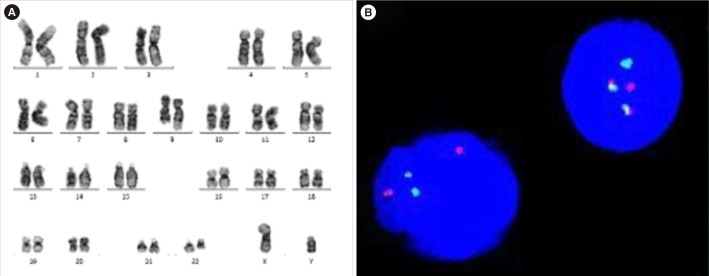
Blood examination showed an Hb level of 61 g/L and a leukocyte count of 296.3×109/L with 15% neutrophils, 2% eosinophils, 2% basophils, 3% lymphocytes, 1% monocytes, 2% blasts, 8% promyelocytes, 13% myelocytes, 25% metamyelocytes, and 29% band neutrophils. Platelet count was 299×109/L. No leukocyte alkaline phosphatase was detected during CLL (leukocyte alkaline phosphatase scores are used to identify CML and leukemoid reaction). Conventional cytogenetic tests on bone marrow revealed 46, XY, t(9;22)(q34;q11.2) [20] with no additional cytogenetic aberrations (Fig. 1A). FISH confirmed the presence of p210 BCR-ABL transcript in all analyzed cells from the same cytogenetic sample (Fig. 1B). Interestingly, mutated IGHV was still positive by multiplex PCR analysis. Therefore, the patient was diagnosed as having chronic phase CML transformed from CLL (Fig. 1).
He was started on the first-generation tyrosine kinase inhibitor (TKI) imatinib at a dose of 400 mg daily in June 2017. Consequently, his complete blood count normalized, and his spleen shrank. He achieved a complete hematologic response within three months of imatinib treatment and demonstrated a complete molecular response with a BCR-ABL/ABL ratio of 0.01%. Currently, the patient is healthy and still on oral imatinib, while the mutated IGHV gene is still positive by multiplex PCR analysis as of March 2019.
In a small cohort of CLL patients, Richter's transformation (RT) to non-Hodgkin's lymphoma, including highly malignant diffuse large B-cell lymphoma, was frequently documented and had a poor prognosis [6]. Risk factors for CLL progression to RT include TP53 mutation or deletion, 14q, 17p deletion abnormalities, and unmutated IGHV status [8]. In the present patient, cytogenetic tests revealed a normal karyotype, and molecular studies confirmed the absence of the TP53 mutation and unmutated IGHV. He was characterized by the presence of p210 BCR/ABL transcript and t(9;22)(q34;q11.2). Most importantly, he had a favorable response to imatinib treatment and achieved complete molecular remission, unlike previous cases [345].
IGHV mutations have been observed in CML patients who progressed to the blast crisis phase [910]. Our patient presented with the absence of BCR/ABL p210 transcript and t(9;22)(q34;q11.2) after treatment with TKIs. However, mutated rearrangement of the IGHV gene was still observed. This result suggests that the two disorders developed from two different leukemia stem cells.
IGHV mutations in our patient were detected by a third-party authoritative testing agency. Because of the long time span since the detection of the IGHV mutations, the mutation figures of CLL and CML could not be provided, which is a limitation of our study.
In conclusion, we describe a case of the transformation of IGHV mutation in CLL into CML with a favorable response to imatinib therapy. The origin of the two disorders in the same or in two distinct cell clones can be demonstrated by means of molecular analysis of IGHV when IGHV-mutated CLL transformed into another malignancy with distinct molecular aberrations.
References
1. Hatoum HA, Mahfouz RA, Otrock ZK, Hudaib AR, Taher AT, Shamseddine AI. Acute myeloid leukemia with T-cell receptor gamma gene rearrangement occurring in a patient with chronic lymphocytic leukemia: a case report. Am J Hematol. 2007; 82:69–72. PMID: 16947317.
2. Garcia-Manero G, Faderl S, O'Brien S, Cortes J, Talpez M, Kantarjan HM. Chronic myelogenous leukemia: a review and update of therapeutic strategies. Cancer. 2003; 98:437–457. PMID: 12879460.
3. Mansat-De Mas V, Rigal-Huguet F, Cassar G, Kuhlein E, Laurent G, Dastugue N. Chronic myeloid leukemia associated with B-cell chronic lymphocytic leukemia: evidence of two separate clones as shown by combined cell-sorting and fluorescence in situ hybridisation. Leuk Lymphoma. 2003; 44:867–869. PMID: 12802927.
4. Morrison VA, Rai KR, Peterson BL, Kolitz JE, Elias L, Appelbaum FR, et al. Therapy-related myeloid leukemias are observed in patients with chronic lymphocytic leukemia after treatment with fludarabine and chlorambucil: results of an intergroup study, cancer and leukemia group B 9011. J Clin Oncol. 2002; 20:3878–3884. PMID: 12228208.
5. Crescenzi B, Sacchi S, Marasca R, Temperani P, La Starza R, Matteucci C, et al. Distinct genomic events in the myeloid and lymphoid lineages in simultaneous presentation of chronic myeloid leukemia and B-chronic lymphocytic leukemia. Leukemia. 2002; 16:955–956. PMID: 11986962.
6. Tsimberidou AM, Keating MJ. Richter's transformation in chronic lymphatic leukemia. Semin Oncol. 2006; 33:250–256. PMID: 16616072.
7. Jelinek DF, Tschumper RC, Geyer SM, Bone ND, Dewald GW, Hanson CA, et al. Analysis of clonal B-cell CD38 and immunoglobulin variable region sequence status in relation to clinical outcome for B-chronic lymphocytic leukaemia. Br J Haematol. 2001; 115:854–861. PMID: 11843819.
8. Parikh SA, Shanafelt TD. Risk factors for Richter syndrome in chronic lymphocytic leukemia. Curr Hematol Malig Rep. 2014; 9:294–299. PMID: 25218362.
9. Spencer A, Szydlo R, Grand FH, Goldman JM, Melo JV. Abnormal patterns of immunoglobulin heavy chain gene DNA fingerprinting during chronic phase chronic myeloid leukemia. Leuk Lymphoma. 1999; 32:299–307. PMID: 10037027.
10. Kiyoi H, Fukutani H, Yamauchi T, Kubo K, Ohno R, Yamamori S, et al. Continuing immunoglobulin heavy chain gene rearrangements in chronic myeloid leukemia with recurrent B-lymphoid blast crisis after bone marrow transplantation. Leukemia. 1995; 9:265–270. PMID: 7869762.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download